CASE REPORT
A 90-year-old female patient came to the Hospital Central de la Defensa Gómez Ulla emergency room due to general malaise, fever and dry cough. Her personal history included hypertension, dyslipidemia, left inguinal hernioplasty, peripheral arterial disease and a thirty-year history of recurrent syncope of probable vasovagal origin. Examination showed BP 130/60 HR 79 BPM SAt 78% ambient Tº 36 celsius. Chest X-ray showed bilateral interstitial infiltrate.
Routine laboratory findings found significantly elevated C-reactive protein, Prothrombin time and D-dimer, and decreased levels of fibrinogen and fibrinogen degradation product (FDP). She was admitted to the hospital with the diagnosis of bilateral pneumonia and secondary acute respiratory failure. Polimerase Chain Reaction test result positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and she received treatment with hydroxychloroquine, ceftriaxone, clexane, and corticosteroids.
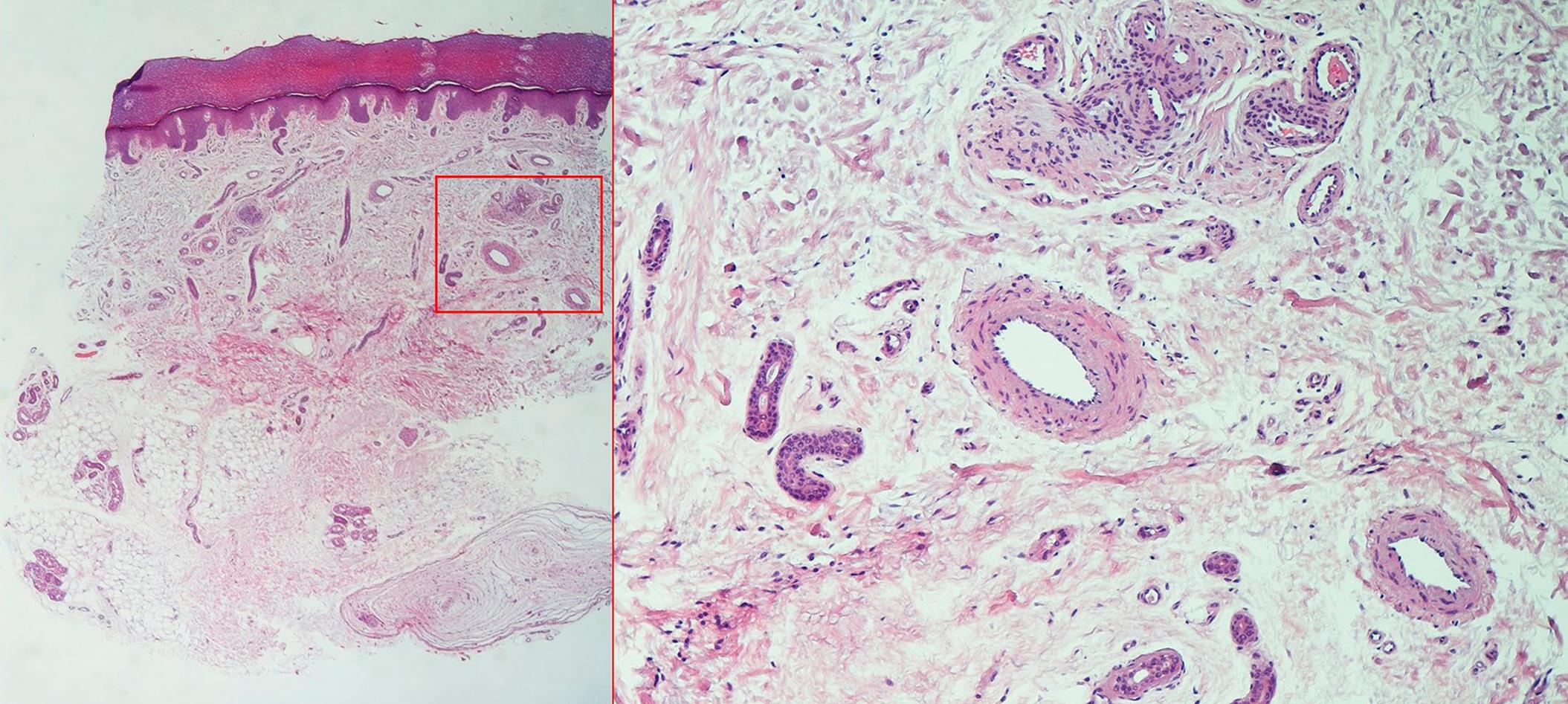
Five days after admission, she developed skin lesions on all the balls of both hands, consisting in macular lesions without palpable component, erythematous and violaceous, with a grayish background, and slow capillary filling (figure 1). A 4 mm punch biopsy was obtained from the edge of a lesion of the third finger of the left hand to clarify the diagnosis and rule out other diseases with similar clinical characteristics, like intravascular thrombosis, vasculitis and chilblain.
DISCUSSION
Coronavirus disease 2019 has become a pandemic condition, yet very little is known about its dermatologic manifestations. The present case was positive in the PCR specific tests for detection of COVID-19, so the possibility that the skin lesions observed could be related to the clinical course of said disease was raised.
Histologically (figure 2), showed an epidermis without significant changes and a dermis with extensive areas of edema, even myxoid changes, and occupied by dilated vessels. There was no vacuolar alteration along the basal layer of the epidermis. Structures made up of medium caliber vascular lumens and a wall endowed with smooth myocytes were observed, which presented a tortuous line in a woll ball-like structure, and were surrounded by nerve tracts and laminated collagen material, forming glomus-like structures. No significant inflammation, vasculitis, acantholysis, or intraluminal fibrin thrombi were identified, thus ruling out the three main diagnoses of clinical suspicion.
Skin specimens of COVID-19 patients show a broad spectrum of cutaneous clinical and histopathological features that may all be linked to the virus interplay with the skin1-3.
According with studies already carried out, some patientes may show epidermal changes like parakeratosis, acanthosis, dyskeratosis, and phenomena of acantholyisis and necrosis of keratinocytes, some of them with lymphocytic satelitosis, others with pseudo-herpetic features4.
Dermal changes most frecuently observed are pictures of perivascular and perianexal lymphocytic infiltrates, and intravascular thrombosis, some accompanied by vasculitis phenomena and the presence of nuclear debris, as well as blood extravasation5.
To date, we do not know any publications in medical literature that describe, in patients with COVID-19, cutaneous lesions that include woll-ball like vascular structures, although evidence of endothelial damage has been found in other organs6.
Among skin pathologies in which a virus is implicated, we can see various types of manifestations in the cutaneous district involved. Clinicopathological features of skin eruption in patients with COVID-19 may reflect a full spectrum of viral interaction with the skin. Further histopathological studies are necessary to clarify the relationship between skin and COVID-19.