Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Andaluza de Medicina del Deporte
versión On-line ISSN 2172-5063versión impresa ISSN 1888-7546
Rev Andal Med Deporte vol.8 no.4 Sevilla dic. 2015
https://dx.doi.org/10.1016/j.ramd.2014.08.003
Effect of aquatic exercise training on lipids profile and glycaemia: A systematic review
Efeito do treinamento físico aquático no perfil lipídico e da glicemia: uma revisão sistemática
R. Delevatti, E. Marson and L. Fernando Kruel
Exercise Research Laboratory, Physical Education School, Federal University of Rio Grande do Sul, Porto Alegre, Brazil
The authors specially thank CAPES, CNPQ and FAPERGS government associations for their support to this study.
ABSTRACT
The objective of this study was to investigate the acute and chronic effects of aquatic exercise training on glycaemia and lipids profile. A systematic review of clinical trials was performed assessing the effects of aquatic exercise and/or training in upright position on lipids profile and glycaemic index. Two raters independently assessed the eligibility criteria and the methodological quality of the studies using the PEDro scale. Average and standard deviation of all variables significantly altered by the interventions were extracted for calculating percentage alterations. Three studies involving the acute effect of aquatic aerobic exercise on the variables of interest were analysed, with two of them demonstrating the efficacy of this type of training in improving lipids profile. Nine studies involving the chronic effects of aquatic training on the same variables were also analysed; eight of them, which assessed different training interventions for different populations, reported benefits of exercise regarding these variables. In conclusion, the improvements found in response to aquatic exercise training in upright position in glycaemia and lipids profile indicate the aquatic environment as a favourable environment for conducting exercise programmes.
Key words: Aquatic exercise. Glucose metabolism. Lipid metabolism.
RESUMEN
El objetivo de este estudio fue investigar los efectos agudos y crónicos del entrenamiento acuático en el perfil lipídico y la glucemia. Se llevó a cabo una revisión sistemática valorando los efectos del ejercicio acuático y/o el entrenamiento en posición erecta sobre índices lipídicos y glucémicos. Dos investigadores valoraron independientemente los criterios de selección y la calidad metodológica de los estudios mediante la escala PEDro. La media y la desviación estándar de todas las variables que se alteraron significativamente por las intervenciones fueron extraídas para calcular el porcentaje de alteración. Se analizaron tres estudios relativos al efecto agudo del ejercicio aeróbico acuático en las variables de interés, dos de ellos demostraron la eficacia de este tipo de entrenamiento sobre el perfil lipídico. Se analizaron también nueve estudios relativos al efecto crónico del entrenamiento acuático sobre las mismas variables, ocho de ellos que valoraron diferentes intervenciones en el entrenamiento con distintas poblaciones, encontraron beneficios del ejercicio en relación a estas variables. En conclusión, las mejoras encontradas en respuesta al ejercicio acuático en posición erecta, sobre el perfil lipídico y la glucemia, indican que el medio acuático es un entorno favorable para llevar a cabo programas de ejercicio.
Palabras clave: Ejercicio acuático. Metabolismo de glucosa. Metabolismo de lípidos.
RESUMO
O objetivo deste estudo foi investigar os efeitos agudos e crônicos do treinamento físico aquático sobre a glicemia e o perfil lipídico. Uma revisão sistemática de ensaios clínicos foi realizada avaliando os efeitos do exercício e/ou treinamento aquático em posição vertical sobre os lipídios do perfil e índice glicêmico. Dois examinadores avaliaram independentemente os critérios de elegibilidade e a qualidade metodológica dos estudos utilizando a escala PEDro. Média e desvio padrão de todas as variáveis significativamente alterados pelas intervenções foram extraídos para calcular alterações percentuais. Foram analisados três estudos envolvendo o efeito agudo do exercício aeróbico aquático sobre as variáveis de interesse, com duas delas demonstrando a eficácia desse tipo de treinamento em melhorar o perfil lipídico. Nove estudos envolvendo os efeitos crônicos do treinamento aquático nas mesmas variáveis também foram analisadas; oito deles, que avaliou diferentes intervenções de treinamento para diferentes populações, relatou benefícios do exercício referentes a essas variáveis. Em conclusão, as melhorias encontradas em resposta ao treinamento de exercício aquático na posição vertical na glicemia e o perfil lipídico indicam o ambiente aquático como um ambiente favorável para a realização de programas de exercícios.
Palavras-chave: Exercícios aquáticos. Metabolismo da glicose. Metabolismo lipídico.
Introduction
Exercise training is widely prescribed as a means of reducing metabolic complications and improving cardiorespiratory capacity, muscle strength and functional capacity; in general, a combination of strength and aerobic exercise is recommended. However, overweight and obese individuals - and, consequently, individuals with a high metabolic risk - can experiment difficulties to execute traditional exercises on dry land due to the necessity of supporting their own body mass. Therefore, exercise modes in which there is no necessity of supporting one's body mass represent an interesting alternative for these populations and have been reported in the literature.1 In this regard, aquatic exercise training is being increasingly recommended for such individuals, since it contributes to the improvement of different aspects of fitness, including aerobic capacity, strength, flexibility and body composition.2
Besides swimming, for which specific and refined motor skills are required, the aquatic environment has been used for several different exercise types executed in an upright position, such as water aerobics, deep water running, water cycling, shallow water walking or aquatic treadmill walking. One advantage of these exercise types over those executed on dry land is the reduction of ground reaction forces, and, consequently, of the load imposed to the musculoskeletal system.3 This facilitates the application and progression of different exercise training models on populations such as the elderly, pregnant women and patients with muscle diseases, osteoarthritis or other degenerative disorders. As a consequence, aquatic exercise is gaining more and more popularity in the fitness field, with its benefits are already reported in the literature.4
In the past decades, aquatic exercise training executed in an upright position was recognized as an important physical activity mode used in prevention of disease, being considered as an alternative for reaching fitness, therapeutic and rehabilitation aims. The effect of this type of exercise training on health parameters has been subject of research involving different populations,5 and primarily by the lower risk of joint injuries, this has been considered ideal for populations, as obese patients, the elderly, and patients with arthritis.1
Given the spread of aquatic exercise as a form of regular physical activity, there is an increasing interest in better understanding the functioning of the human organism during immersion in water. For adequately prescribing aquatic exercise training, the physical properties of water have to be considered, since they differ considerably from those of air, which is reflected in the differences in physiological responses to exposure to these environments. The main physical properties related to the physiological alterations during immersion in water are the increased heat exchange between the organism and the environment; the buoyancy, which operates against the force of gravity; and the hydrostatic pressure that affects cardiovascular parameters during rest and exercise.6 One important point to be considered is that the magnitude of the physiological alterations in response to immersion in water depends on the depth of immersion.
The most studied physiological alterations during aquatic exercise are those affecting the cardiovascular system. A possible cause for this is the direct influence of the physical properties of water, specially the hydrostatic pressure, on the circulatory system. Immersion in water induces a hydrostatic pressure gradient that affects all vascular columns of the organism, exerting pressure in the whole immersed body surface. This increases the venous return, augmenting the blood volume in the heart and intrathoracic vasculature.7 The increased blood flow from the lower limbs to the central regions, which can reach 700 ml/min-1, leads to augmented pressures in the thorax, central veins, lungs and right atrium.8 This blood flow shift also increases the final diastolic volume and, consequently, the systolic volume. Although a decrease in heart rate occurs, which can be understood as a compensatory mechanism, an increase in cardiac output is also apparent. A considerable extent of this increase (32-62%) in cardiac output is explained by the dominance of the augmented systolic volume over the decreased heart rate. At the same time, mean arterial blood pressure remains stable, indicating a reduction in total peripheral resistance. Concerning the systemic oxygen consumption, it remains unaltered in thermoneutral temperatures. In contrast to what occurs on dry land, however, it is not regulated by the metabolic demands of peripheral tissues, since blood flow regulation is affected by water immersion. As a result, oxygen delivery to tissues rises and frequently exceeds tissue demands.8
Haemodynamic variables are not the only parameters affected by the mentioned blood flow redistribution and the resultant central hypervolemia. Indeed, the augmented atrial pressure stimulates low-pressure cardiopulmonary receptors, inhibiting the sympathetic nervous activity, which, in turn, controls systemic circulation and kidney function. Consequently, plasma renin activity (PRA) and plasma adrenocorticotropic hormone (ACTH) activity are suppressed, since their release is mainly controlled by sympathetic nervous activity.9 Furthermore, the activation of heart mechanoreceptors resulting from water immersion also causes neural and hormonal adjustments.10 These adjustments include the diminished release of vasopressin and aldosterone, an inhibition of the sympathetic nervous activity in the kidneys, and increased release of prostaglandin in the kidneys and atrial natriuretic peptide, causing diuresis, natriuresis and kaliuresis. It is important to bear in mind, however, that these parameters are also affected by salt intake, hydration status and physical activity.10
Physiological alterations such as the renin-angiotensin-aldosterone system (RAAS) suppression are of high clinical relevance, since the activation of this system is associated with the development of chronic diseases including obesity and type-2 diabetes mellitus (DM-2), being decisive for the occurrence of cardiovascular disease. Thus, suppressing RAAS activity can contribute to the prevention of diseases such as DM-2 through enhanced insulin release and sensitivity.11 The effects of insulin can be down-regulated by angiotensin II, since this hormone is able to stimulate phosphorylation of tyrosine in the insulin receptors (IRS-1 and IRS-2), as well as their associations with PI-3 kinase, inhibiting this enzyme.12 This phenomenon can be prevented by the use of angiotensin II receptor (AT1) blockers.13
Due to the negative effect of angiotensin II on insulin signalling, the RAAS is suggested to contribute to insulin resistance and development of DM-2.14 Importantly, insulin resistance in skeletal muscle, which often affects sedentary individuals, can also lead to disturbances is lipids profile and metabolism.15 Since the RAAS regulates vascular tone, angiotensin II release can lead to reductions in skeletal-muscle blood flow, impairing glucose consumption by muscle. Accordingly, Mitsuishi et al.16 demonstrated that blocking the RAAS can partially revert decreases in mitochondrial content, improving fatty acid oxidation, intramuscular content of triacylglycerol and glucose tolerance. Furthermore, there is evidence that angiotensin II release inversely correlates to expression and activity of lipoprotein lipase in adipose tissue.17 In a recent review, Goossens11 cited a decrease in adipose-tissue lipolysis after exposure of this tissue to angiotensin II.
The presented associations reflect the role played by the alterations caused by water immersion, and especially by the inhibition of RAAS, in different biochemical outcomes. Analysis of blood parameters is used for assessing health status and diagnosing disease or pre-disease conditions. These parameters are frequently used to assess health disturbances in middle-aged and elderly individuals. Examples of such measures are glycaemic, lipids and lipoprotein levels; these variables are also frequently investigated in exercise science, since exercise can improve them. Nevertheless, studies showing the response of these biochemical variables to different aquatic exercise training models are still scarce. This field of study is particularly interesting due to the physiological alterations associated to water immersion and the increasing engagement of overweight, obesity and elderly individuals, as well as of individuals affected by endocrine-metabolic diseases, in aquatic exercise training programmes. Accordingly, this review addresses the responses of glycaemia and lipids profile to the physiological alterations caused by water immersion. In addition, the acute and chronic effects of aquatic exercise training on these responses are discussed.
Method
Study design
This study is a systematic review in which relevant clinical trials were identified, selected and evaluated, providing practical and theoretical support to the classification and analysis of the literature review. The methods used for the systematic review follow below.
Literature search
In January 2013, computer searches for articles were performed in Scopus (www.scopus.com) and PubMed (www.pubmed.gov) databases, while master and doctoral theses were performed in LUME (on-line database of the Federal University of Rio Grande do Sul, Brazil, containing master and doctoral theses). Publication year was unlimited and the following key words were used: "physical activity", "exercise", "training", "aquatic", "water-based", "hydrotherapy", "hydrogymnastics", "deep water running", "deep water walking" and "head-out aquatic", brought them together by means of the boolean operator "OR". Besides this, references provided in the documents identified by these searches were screened with the purpose of finding additional studies.
Due to the higher availability and ease for searching and reading, only documents written in English, Portuguese and Spanish were used in this study.
Inclusion criteria
Criteria for inclusion of studies in the present review were as follows:
(1) Intervention studies (acute and chronic treatment).
(2) Use of aquatic exercises and/or aquatic exercise training executed in an upright position (with the head out of the water).
(3) Use of human subjects.
(4) Assessment of lipids or glycaemic profile variables.
Regarding the exercise and training aims, protocols aiming at strength, aerobic or combined (strength and aerobic) improvements were included in the review, without restriction of training frequency and intensity, as well as duration of training sessions.
PEDro scale
The PEDro (Physiotherapy Evidence Database) scale18 was used for rating the documents included in the analysis. This scale was developed by the Centre for Evidence-Based Physiotherapy with the purpose of objectively evaluating the internal validity of studies. Each document was assessed through several criteria previously established, that overall, aim to evaluate four fundamental methodological aspects of a study such as the random process, the blinding technique, group comparison, and the data analysis process, being attributed a maximal value of 10 points. These 10 points were distributed among the seven criteria scale of possible control in intervention studies with physical training. Thus, studies were considered of excellent quality those who completed at least six criteria (8.57 points), not being associated with excellence the criterion on intention-to-treat analysis, which although very important clinically, it is still very unusual in studies aiming to analyse responses to physical training. Two raters evaluated the documents independently using the scale; in case of differences between the values attributed by them, the evaluation was discussed until a consensus was reached.
Results
From the 64 articles identified, 53 were excluded after analysis of titles and abstracts. Were included 11 articles as potential studies, a study being excluded for not having sufficient information about exercise intervention. Therefore, 10 studies were included in this review. The process of identification and selection of studies is shown in Fig. 1.
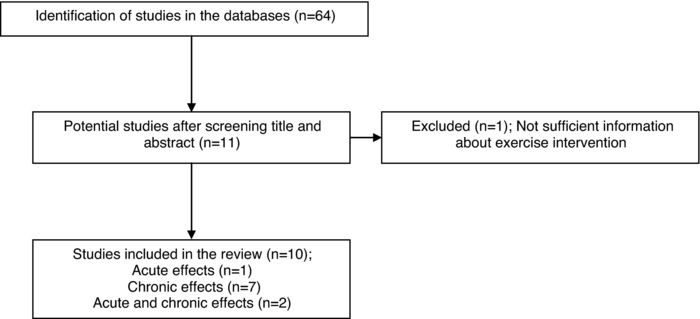
Figure 1. Acute effects of aquatic exercise training on glycaemia and lipids profile.
Acute effects of aquatic exercise training on glycaemia and lipids profile
The average (± standard deviation) score of the analysed articles on the PEDro scale was 8.10 ± 0.83 points; only three studies were found and no study reached the highest score. The selected studies presented the specified eligibility criteria and the random distribution of treatments, but since they involved physical training, the scale criteria 3, 5 and 6, related to blinded interventions, were not considered, as it would not be possible to blind subjects and/or researchers in such interventions. By exclusion these three criteria of scale, the 10 points considered for assessment of methodological quality are the result of a redistribution of the total score of the seven criteria PEDro scale (2, 4, 7, 8, 9, 10 and 11), being assigned 1.42 for each criterion.
Table 1 shows the acute effects of aquatic training on lipids profile and glycaemia found in the three studies analysed, together with a summary of the development of the studies, including intervention duration, type, volume and intensity of training sessions, sample, main outcomes, percentage of improvement and score in the PEDro scale.
The three analysed studies19-21 involved aerobic aquatic exercise, and the interventions were effective in improving lipids profile in two20,21 of them. This effect was independent on the training status of the participants.
Although all training sessions of these studies were focused on aerobic exercise, they were executed through different manners (underwater cycle ergometer,19 underwater treadmill20 and water aerobics,21 emphasizing the different types of exercise that can be used for aerobic training in the aquatic environment.
In spite of the benefits in lipids profile described by two these studies,20,21 methodological differences between them, such as population and characteristics of exercise session impairs the formulation of definitive conclusions and practical applications regarding this subject.
Chronic effects of aquatic exercise training on glycaemia and lipids profile
The number of studies evaluating chronic outcomes (n = 9) was slightly higher than for the acute effects studies. Average (± standard deviation) score obtained by these studies in the PEDro scale was 8.58 ± 1.65 points, with three22-24 studies obtaining the maximal score. Only one study22 did not specify its eligibility criteria. Concerning random distribution of interventions, only one study23 did not meet this criterion; nevertheless, this was not due to low methodological quality, but to the study design, since the authors analysed the effect of one aquatic exercise training protocol on two different populations. In this case, the score was redistributed within the other scale criteria. As in the studies about acute effects, scale criteria 3, 5 and 6 were not considered for the same reason.
Table 2 shows the chronic effects of aquatic exercise training on lipids profile and glycaemia in the nine studies analysed, as well as research development, intervention duration, type, volume and intensity of the training protocol, environment, sample, main results, percentage of improvement and score in the PEDro scale.
From the nine reviewed studies, three analysed aerobic exercise,20-22 five analysed combined training (resistance and aerobic),23-27 and only one analysed isolated resistance training.28
Among the studies involving aerobic exercise, two presented interventions using water aerobics and one used walking and/or running on an underwater treadmill as exercise type. All studies demonstrated significant improvements in at least one of the lipids profile parameters, while only two studies measured glycaemia through glycated haemoglobin (HbA1c)22,27 values, finding significant effects of exercise on this variable.
The majority of the studies investigating the chronic effects of aquatic exercise training used a combination of aerobic and strength training.23-27 Of these studies, four24-27 used water aerobics as exercise type, with three24-26 of them showing positive results of exercise in lipids and lipoprotein profiles. Only one27 of these studies evaluated HbA1c values, with authors reporting decreases in these values and, therefore, efficacy of the intervention in improving glycaemic control in DM-2 patients. Additionally, the study using deep-water running23 as exercise type for healthy individuals and individuals presenting glucose intolerance also found diminished postprandial glycaemic values in the patients with glucose intolerance after the training intervention.
Only one study used strength training without combination with aerobic training.28 In this study, no significant alterations in lipids profile and glycaemia were found in response to aquatic exercise training.
Discussion
Based on the analysed studies, it is possible to identify three different modes of manipulating aquatic exercise training: aerobic training, strength training and a combination of aerobic and strength training. Protocols involving these training modes can be designed for different exercise types, including walking and/or running on underwater treadmill or deep water, underwater cycling and water aerobics, all executed in an upright position. In all protocols, subjects were exposed to the physical properties of water and, consequently, to the physiological alterations resulting from immersion in water which were already described in the present review. Overall, the lipid and glucose changes found in studies with aquatic exercise training are similar or superior to those found in studies with land exercise training.
The study designs, samples and manipulation of training variables, specially intensity and volume, together with considerations about the results reported and the remaining uncertainties in this field of study are addressed in the following topics.
Studies involving aerobic exercise/training
Two different designs were identified in studies regarding aerobic training, comparisons between exercise on dry land and in water; and comparisons between a training group and a control group. The populations examined were elderly men with history of heart ischaemic disease, dyslipidemic premenopausal women, overweight and obese subjects and patients diagnosed with DM-2; thus, responses to exercise and water immersion could be reviewed only for these populations. In the three20-22 studies examining the effects of chronic exercise training, interventions had duration of 12 weeks; it was not possible to find studies with longer periods of intervention. While in one study21 participants exercised twice a week during the intervention period, in the others studies individuals underwent three exercise sessions per week. In one study,19 the duration of the exercise sessions was 15 min, considerably lower for aerobic exercise aiming at improvements in lipids metabolism, which is between 30 and 60 min. The minimal duration recommended (30 min) was reached by the other two studies21,22; only one study20 controlled exercise duration through energy expenditure instead of time in minutes. Three different manners of controlling intensity could be identified in the studies: rate of perceived exertion (RPE), percentage of the maximal heart rate, and velocity corresponding to a given percentage of maximal oxygen consumption (VO2max). Considering the three studies20-22 with a 12-week intervention, two20,21 presented intensity progression throughout the training period, one20 with intensities varying between 60% and 85% of VO2max and the other21 with RPE values varying between 11 and 15 points using the Borg Scale (minimum of 6 and maximum of 20 points).
No studies evaluating glycaemic measures were found. However, improvements in lipids profile were found both acutely and chronically, with exception of the study by Berminghan et al.,19 in which the lack of improvements most likely results from the intensities and short duration of the training sessions. Nuttamonwarakul et al.22 controlled glycaemic values by measuring HbA1c and, despite the lack of intensity progression during the training period, considerable improvements in this parameter were found, exceeding the improvements found by previous studies involving on-land exercise in individuals with DM-2.29,30
Future studies could examine the effects of longer interventions, higher training volumes and intensity control according to the anaerobic threshold or its markers, since this parameter is considered excellent for controlling intensity during aerobic exercise training.31 Furthermore, comparing continuous and interval training, as well as analysing the mechanisms underlying the effects of immersion in water on lipids profile and glycaemic variables would be possible and highly relevant.
Studies involving strength exercise/training
Among the studies analysed, only one28 investigated the effects of aquatic strength training, comparing them to those of strength training executed with elastic bands on dry land. In this study, postmenopausal women underwent a 12-week intervention, with training frequency increasing from two to three sessions per week during the training period. Additionally, over the training period, volume increased from one set to two supersets and intensity increased from 5 to 7 points of the OMNI scale (RPE). No significant differences were found in fasting glycaemia and lipids profile in response to this training mode, which appears not to be the more adequate for populations in which these alterations are important aims. It is also important to consider that the magnitude of intensity progression was not very high; this could have been a reason for the lack of improvements in biochemical parameters found, since high-intensity strength training on dry land can enhance glycaemia and lipids profile in DM-2 patients.32 Currently, research has been demonstrating increased strength in different populations when aquatic strength training is executed at maximal velocities.33,34 The impact of this strategy on biochemical variables is, though, still unclear.
Definitive conclusions about the effects of this type of training on the parameters focused in this review are prevented by lack of studies with a higher level of evidence, such as randomized controlled trials. In addition, the only study involving aquatic strength training presented in its prescription moderate intensities, which are not characteristic of training programmes aiming at strength gains.
Studies involving combined strength and aerobic exercise/training
Studies analysing responses of lipids profile and glycaemia to combined training can be divided into three groups according to their methods: (a) comparisons between exercise in water and on dry land (one study26); (b) comparisons between training and control groups (two studies24,27); and (c) comparison of pre- and post-training values of one group (two studies23,25). The populations examined were healthy premenopausal and elderly women, middle-aged overweight women (both glucose tolerant and intolerant), middle-aged men with coronary artery disease, and men and women with DM-2 and/or cardiac insufficiency. Intervention duration of the studies ranged between eight and 20 weeks, with an average training frequency of three sessions per week.
The study26 with the highest training frequency - four sessions per week - presented the only protocol in which aerobic and strength-training sessions were separately executed in different days. This can be an interesting strategy when planning exercise training programmes, since it leads participants to engage in physical activity four days per week and diminishes the monotony of the sessions.
On average, total session duration of the analysed studies was approximately 60 min. In almost all studies, aerobic training sessions had a duration of about 30-40 min, with no changes along the training period. Control of session duration through energy expenditure was not used in any of these studies. In turn, strength-training volume varied between one and six sets per exercise and duration of sets was controlled through different manners, such as maximal repetition number or percentages of it, execution time or fixed number of repetitions at maximal velocity. As a consequence of the considerable differences in training volume between the studies, it remains difficult to explore and associate the results with training prescription.
With respect to aerobic training intensity, three23,25,26 studies controlled this parameter during aerobic training through percentages of maximal heart rate, which ranged between 50% and 85%. Other manners of prescribing exercise intensity found were the use of heart rate reserve measures and the identification of heart rate values at the anaerobic threshold. None of the analysed studies presented intensity progression throughout the training period, which is a possible limiting factor for several physiological adjustments.
Regarding intensity prescription of strength training, exercise execution at maximal velocity was used in two studies. Another form of controlling this variable when exercising at submaximal intensities is the use of percentages of the maximal number of repetitions; this method, however, presents the disadvantage of requiring the execution of repetition maximum series in the water - in these cases, fatigue can lead to a diminution in velocity of execution, which in turn decreases the water resistance to the movement, altering the exercise load. Thus, it is possible to control intensity by determining a given number of repetitions to be executed within a determined time; however, it has to be considered that this measure is not related to repetition maximum values. The other methods used for controlling intensity were not sufficiently described in the studies, preventing their discussion. Only one study25 explored an interesting intensity progression throughout the strength-training period, starting with two sets of 30 s, progressing until six sets of 10 s at maximal velocity.
Only two studies23,27 examined glycaemic variables and four studies23-27 assessed lipids profile. In all studies, combining aerobic and strength training elicited significant improvements in at least one of these variables when compared to the control group or pre-training values. The only study comparing aquatic exercise training to training on dry land demonstrated a lack of differences between these two exercise types. This emphasizes the advantages of aquatic exercise training, since this type of training could elicit the same biochemical improvements resulting from training on dry land, with the additional benefit of increased buoyancy and diminished load imposed to the musculoskeletal system.3
Suggestions for further studies include the comparison between biochemical responses elicited by exercise training in water and on dry land. Another important point would be to prescribe exercise based on maximal and/or submaximal tests executed in the training environment. Prescribing aquatic exercise training based on results reached during tests on dry land can lead to considerable errors and imprecisions, since the physiological peculiarities of water immersion, discussed in this review, are neglected in such situations.
The reduced number of database searched is a limitation in our literature search. However, the broad reach of the searched databases (PubMed and Scopus), we believe that our findings reflect the current literature on the topic of study.
Conclusion
Methodological differences between the few studies analysing the responses of glycaemia, lipoproteins and lipids profile to aquatic exercise impedes definitive conclusion about this subject. However, studies regarding responses to chronic aquatic exercise training indicate that aerobic and combined training are interesting interventions when aiming at improvements in these variables. The same has not been proven for resistance training, because the only study involving aquatic strength training found showed training characteristics incompatible with the proposal to strength gain.
In a considerable number of studies, metabolic benefits in response to aquatic exercise training could be found despite methodological flaws. This points out to the possible existence of not only an effect of exercise training in these studies, but also an effect of the physiological alterations due to immersion in water. However, these physiological alterations are still not adequately or sufficiently employed in the fields of physical activity and physical training for health.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
1. Meredith-Jones K, Waters D, Legge M, Jones L. Upright water-based exercise to improve cardiovascular and metabolic health: a qualitative review. Complement Ther Med. 2011;19:93-103. [ Links ]
2. Alberton CL, Kruel LFM. Influêcia da Imersão nas Respostas Cardiorrespiratórias em Repouso. Rev Bras Med Esporte. 2009;15:228-32. [ Links ]
3. Silva EM, Kruel LFM. Caminhada em Ambiente Aquático e Terrestre: Revisão de Literatura Sobre a Comparação das Respostas Neuromusculares e Cardiorrespiratórias. Rev Bras Med Esporte. 2008;14:500-4. [ Links ]
4. Barbosa TM, Garrido MF, Bragada J. Physiological adaptations to head-out aquatic exercises with different levels of body immersion. J Strength Cond Res. 2007;21:1255-9. [ Links ]
5. Barbosa TM, Marinho DM, Reis VM, Silva AJ, Bragada JA. Physiological assessment of head-out aquatic exercises in healthy subjects: a qualitative review. J Sports Sci Med. 2009;8:179-89. [ Links ]
6. Arborelius M Jr, Ballidin UI, Lilja B, Lundgren CE. Hemodynamic changes in man during immersion with the head above water. Aerosp Med. 1972;43:592-8. [ Links ]
7. Epstein M. Cardiovascular and renal effects of head-out water immersion in man: application of the model in the assessment of volume homeostasis. Circ Res. 1976;39:619-28. [ Links ]
8. Pendergast R, Lundgren CEG. The underwater environment: cardiopulmonary, thermal, and energetic demands. J Appl Physiol. 2009;106:276-83. [ Links ]
9. Corruzi P, Novarini A, Rossi E, Borghetti A. Effects of "central hypervolemia" by water immersion on renin-aldosterone system and ACTH-cortisol axis in hemodialyzed patients. Nephron. 1984;36:238-41. [ Links ]
10. Rim H, Yun YM, Lee KM, Kwak JT, Ahn DW, Choi JK, et al. Effect of physical exer-cise on renal response to head-out water immersion. Appl Hum Sci. 1997;16: 35-43. [ Links ]
11. Goossens GH. The renin-angiotensin system in the pathophysiology of type 2 diabetes. Obes Facts. 2012;5:611-24. [ Links ]
12. Saad MJA, Velloso LA, Carvalho CR. Angiotensin II induces tyrosine phosphorylation of insulin receptor substrate 1 and its association with phosphatidylinositol 3-kinase in rat heart. Biochem J. 1995; 310:741-4. [ Links ]
13. Carvalho-Filho MA, Carvalheira JB, Velloso LA, Saad MJ. Cross-talk das vias de sinalização de insulina e angiotensina II: implicações com a associação entre diabetes mellitus e hipertensão arterial e doença cardiovascular. Arq Bras Endocrinol Metab. 2007;51:195-203. [ Links ]
14. Kasper S, Castle S, Daley B, Enderson B, Karlsta M. Blockade of the renin- angiotensin system improves insulin sensitivity in thermal injury. Shock. 2006;5:485-8. [ Links ]
15. Duvivier BM, Schaper NC, Bremers MA, van Crombrugge G, Menheere PP, Kars M, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLOS ONE. 2013;8:1-8. [ Links ]
16. Mitsuishi M, Miyashita K, Muraki A, Itoh H. Angiotensin II reduces mito-chondrial content in skeletal muscle and affects glycemic control. Diabetes. 2009;58:710-7. [ Links ]
17. Saiki A, Koide N, Watanabe F, Murano T, Miyashita Y, Shirai K. Suppression of lipoprotein lipase expression in 3T3-L1 cells by inhibition of adipogenic dif-ferentiation through activation of the renin-angiotensin system. Metabolism. 2008;57:1093-100. [ Links ]
18. PEDro Scale. The Physiotherapy Evidence Database (PEDro). http://www.pedro.org.au/; Updated June 21, 1999 (accessed 10.09.12). [ Links ]
19. Bermingham MA, Mahajan D, Neaverson MA. Blood lipids of cardiac patients after acute exercise on land and in water. Arch Phys Med Rehabil. 2004; 85:509-11. [ Links ]
20. Greene NP, Martin SE, Crouse SF. Acute exercise and training alter blood lipid and lipoprotein profiles differently in overweight and obese men and women. Obesity (Silver Spring). 2012;20:1618-27. [ Links ]
21. Costa RR (Dissertasao de Mestrado) Efeitos agudos e crônicos do treinamento em hidroginástica no perfil lipídico e na enzima lipase lipoprotéica de mulheres pré-menopáusicas dislipidêmicas. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2011. [ Links ]
22. Nuttamonwarakul A, Amatyakul S, Suksom D. Twelve weeks of aqua-aerobic exercise improve physiological adaptations and glycemic control in elderly patients with type 2 diabetes. J Exerc Physiol Online. 2012;2:64-70. [ Links ]
23. Jones LM, Meredith-Jones K, Legge M. The effect of water-based exercise on glucose and insulin response in overweight women: a pilot study. J Womens Health (Larchmt). 2009;8:1653-9. [ Links ]
24. Takeshima N, Rogers ME, Watanabe E, Brechue WF, Okada A, Yamada T, et al. Water-based exercise improves health-related aspects of fitness in older women. Med Sci Sports Exerc. 2002;34:544-51. [ Links ]
25. Tormen MLS (Dissertasao de Mestrado) Efeitos do treinamento e destreinamento de hidroginástica no perfil lipídico e na remodelação óssea em mulheres pré-menopáusicas. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2007. [ Links ]
26. Volaklis KA, Spassis AT, Tokmakidis SP. Land versus water exercise in patients with coronary artery disease: effects on body composition, blood lipids, and physical fitness. Am Heart J. 2007;154:e1-6. [ Links ]
27. Asa C, Schaufelberger M, Katharina SS, Bert A. Aquatic exercise is effective in improving exercise performance in patients with heart failure and type 2 diabetes mellitus. Evid Based Complement Altern Med. 2012:1-8. [ Links ]
28. Colado JC, Triplett NT, Tella V, Saucedo P, Abellán J. Effects of aquatic resistance training on health and fitness in postmenopausal women. Eur J Appl Physiol. 2009;106:113-22. [ Links ]
29. Cauza E, Hanusch-Enserer U, Strasser B, Ludvik B, Metz-Schimmerl S, Pacini G, et al. The relative benefits of endurance and strength training on the metabolic factors and muscle function of people with type 2 diabetes mellitus. Arch Phys Med Rehabil. 2005;86:1527-33. [ Links ]
30. Karstoft K, Winding K, Knudsen SH, Nielsen JS, Thomsen C, Pedersen BK, et al. The effects of free-living interval-walking training on glycemic control, body composition, and physical fitness in type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2013;36:228-36. [ Links ]
31. Azevedo M, Garcia A, Duarte P, Rissato M, Carrara P, Marson A. Anaerobic thresh-old and bioenergetics: a didactic approach. Maringá. 2009;20:453-64. [ Links ]
32. Brooks N, Layne JE, Gordon PL, Roubenoff R, Nelson ME, Castaneda-Sceppa C. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int J Med Sci. 2006;4:19-27. [ Links ]
33. Souza AS, Rodrigues BM, Hirschmmann B, Graef FI, Tiggemann CL, Kruel LFM. Treinamento de força no meio aquático em mulheres jovens. Motriz. 2010;16:649-57. [ Links ]
34. Butelli ACK (Dissertasao de Mestrado) Efeitos de um treinamento de força no meio aquático com diferentes volumes em homens jovens. Porto Alegre: Uni-versidade Federal do Rio Grande do Sul; 2011. [ Links ]
![]() Correspondence:
Correspondence:
E-mail address: rsdrodrigo@hotmail.com
(R. Delevatti).
Received 16 January 2014
Accepted 29 August 2014














