Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Osteoporosis y Metabolismo Mineral
versión On-line ISSN 2173-2345versión impresa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.10 no.1 Madrid ene./mar. 2018 Epub 03-Abr-2023
https://dx.doi.org/10.4321/s1889-836x2018000100007
Review
Osteoporosis and spinal surgery: strategies for medical and surgical treatment
1 Servicio de Neurocirugía - Complejo Hospitalario Universitario Insular-Materno Infantil de Las Palmas de Gran Canaria - Las Palmas de Gran Canaria (España)
2 Servicio de Neurocirugía - Hospital Universitario Central de Asturias - Oviedo (España)
The prevalence of osteoporosis in patients undergoing spinal surgery is estimated at 50% in women over 50 years, a higher figure than in the general population adjusted for age. Consequently, many authors recommend the systematic assessment and timely treatment of osteoporosis in most patients who are going to undergo arthrodesis.
The decrease in bone mineral density (BMD) is the main factor in independent risk related to the failure of the instrumentation in spinal fusion surgeries.
Complications arising from spinal fusion are more frequent in osteoporotic patients over 65. The most frequent early complications are pullout or tearing pedicular screws, pedicular fracture and fracture by compression in the adjacent vertebral segment. After 3 months, the most frequent complications are pseudoarthrosis, fracture or mobilization of the bars, subsidence of vertebral intersomatic boxes and the kyphosis of the proximal joint.
There are some clinical trials of spinal arthrodesis surgery with perioperative treatment with alendronate, zoledronic acid, or teriparatide that have been shown to be effective in clinical improvement and increase in fusion rates.
Several modifications in the surgical arsenal may improve fusion rates and decrease surgical complications. Arthrodesis has been highlighted with cemented and expandable pedicle screws.
Finally, randomized clinical trials have shown that vertebral reinforcement treatments in osteoporotic vertebral fractures are beneficial in the short and long term.
Bone metabolism and spinal disorder
Spinal fusion surgeries with or without instrumentation have become well-established surgical procedures in the therapeutic arsenal of spinal disease, either degenerative, deformity (scoliosis and degenerative kyphosis), vertebral instability (degenerative spondylolisthesis and isthmus) and in stenosis of the lumbar spinal canal (central or foraminal).
The gradual aging of the population has led to an increase in spinal fusion surgeries in elderly patients. From 2001 to 2007, spinal fusion procedures in those insured by Medicare in the USA increased 15 fold 1. A significant percentage of patients who require lumbar or cervical vertebral arthrodesis are older than 50 years, many of whom suffer from osteoporosis without being correctly diagnosed.
In Spain, approximately 2 million women suffer from osteoporosis, according to the densitometric criteria proposed by the World Health Organization (WHO). Díaz-Curiel et al. estimated that the prevalence of osteoporosis in Spain is around 26% (1 in 4) of women over 50 years of age 2.
In a recent study in patients over 50 years who underwent spinal surgery, 41.4% of women were reported to have osteopenia and 51.3% had osteoporosis. On the other hand, in men, 46.1% presented osteopenia and 14.5% osteoporosis 3,4. Thus, the prevalence of osteoporosis in women undergoing spinal surgery is higher than that of the general population adjusted for age. Consequently, many authors recommend the systematic evaluation and timely treatment of osteoporosis, especially in women over 50 3.
Patients with osteoporosis present a lower bone mineral density (BMD) and lower osteoblastic activity, which negatively influence osteoconductive, osteoinductive and osteogenic capacity. Therefore, patients with osteoporosis have increased bone remodeling and negative final bone balance, which results in poor bone fusion, and a reduction in the force of extraction or pullout of the pedicle screws 4.
Reduced BMD is the main independent risk factor related to instrumentation failure in lumbar fusion surgeries4 and a moderate risk factor for the development of pseudoarthrosis. BMD is significantly higher in patients who achieve higher fusion rates compared to those who suffered from a lack of fusion after vertebral column arthrodesis, according to some reports 5. Although the development of pseudoarthrosis is multifactorial, a significant proportion could be explained by low BMD levels 6.
Complications in spinal surgery associated with osteoporosis
Arthrodesis with long instrumentation assemblies are increasingly common in the treatment of spinal deformity (scoliosis and degenerative kyphosis). Scoliotic deformities are present in 36-48% of osteoporotic women and patients with large deformities in the spine usually have a low BMD 7. Complications derived from spinal fusion surgery tend to be more frequent in patients over 65 and osteoporotic.
Early complications occur within the first 3 months of surgery. The most frequent are the pullout or removal of the pedicle screws, epidural hematoma, pedicular fracture and fracture of the adjacent vertebral segment by compression mechanism 7 8 9-10.
Late complications, after 3 months include pseudoarthrosis, fracture or mobilization of the bars, fracture by compression mechanism of the adjacent vertebral segment, pain in the iliac area (specifically in the area of insertion of the iliac screws), disc herniation (mostly cephalic), subsidence of vertebral intersomatic boxes and proximal junction kyphosis (PJK) (Figure 1).

Figure 1. (A) Lateral radiograph of lumbosacral spine: S1 screw rupture is observed (arrow). (B) Surgical part of ,the broken screw removed. (C) side of the lumbosacral spine where mobilization bar distally (arrow) x. (D) CT axial cut and (E) sagittal, hypodense halo is observed around the pedicle screws (arrows), characteristic of pseudoarthrosis. (F) Sagittal CT that illustrates the presence of subsidence or subsidence of the intersomatic device, note the loss of the disc height and the erosion of the vertebral plates (arrow)
Instrumentation failure may also be subdivided according to the location of the instrumentation, either anterior or posterior. The latter tends to fail due to a limited fixing force in the bone of low density, which results in the extraction or pullout and/or loosening of the pedicle screws 11,12. In contrast, anterior instrumentation is subject to a repetitive cyclic load, resulting more frequently in screw rupture or implant subsidence in patients with BMD involvement 12,13.
Osteoporosis is a major risk factor for the failure of surgery in the spine, and even more so when multiple vertebral levels are instrumented 14,15.
De Wald et al. 10 reported that the two most frequent mechanisms of complications in patients over 65 years of age, operated on at least 5 levels of instrumentation, were vertebral fracture by compression mechanism of the last superior vertebral segment of an arthrodesis and PJK to the last instrumented segment in 28% of cases. Other articles concur that PJK is the most frequent complication in multi-level instrumented columns 16 17-18. As a complication, PJK has provoked much interest in its frequency and complexity. The Scoliosis Research Society defines proximal junctional kyphosis (PJK) as the kyphotic Cobb angle equal to or greater than 20º between the last instrumented vertebra and the two vertebrae located above (Figure 2). PJK occurs in 39% of operated deformities occurring most between 6-8 postoperative weeks. The three most important risk factors are advanced age, poor bone quality and significant sagittal imbalance prior to surgery. Of all the patients who develop PJK, approximately one third are re-operated early before 5 months for surgical revision due to mechanical failure and vertebral instability 19.

Figure 2. (A) Sagittal CT at the thoracolumbar level; osteoporotic compression fracture at level D12 with segmental kyphosis is observed. (B) Arthrodesis through instrumentation with pedicle screws from D10 to L2, with significant kyphosis correction. (C) Lateral radiography: vertebral compression fracture at D10 level with kyphosis of the proximal junction and screw pullout at level D10. (D) Extension of arthrodesis, superior to levels D8 and D9 and inferior to levels L3 and L4, and correction of kyphosis
It is important to consider that a preoperative thoracic kyphosis of more than 30º is an independent risk factor for the appearance of PJK, and that the adequate resolution of the sagittal imbalance prior to surgery reduces the incidence of PJK from 45% to 19% (20).
Medical treatment strategies
Patients with osteoporosis and with uncorrected hypovitaminosis D reported present worse rates of bone fusion after vertebral arthrodesis and may also have poorer clinical results in disability scales in the perioperative period 4.
In recent decades there has been a significant advance in the knowledge of the pathophysiology of bone formation and resorption, as well as in the treatment of osteoporosis, which logically leads us to wonder about the influence of these therapies in the bone fusion process in spinal surgery 21. Currently an increasing number of studies and clinical trials evaluate the impact of various pharmacological treatments (bisphosphonates, zolendronic acid, PTH) on bone fusion in spinal surgeries. Table 1 summarizes the main studies to date.
Table 1 The prevention and timely treatment of osteoporosis is the most important principle

OP: osteoporosis; PLIF: posterior lumbar intersomatic fusion; X-ray: radiography; CT: computed tomography; 3-D: three-dimensional.
In experimental animals, 18 studies have been reported that assessed the influence of bisphosphonates on the fusion process in arthrodesis, most of them did not demonstrate significant effects on bone fusion rate probably attributed to low statistical power. Studies in animals with bisphosphonate-based therapy showed that the bone fusion mass was histologically less mature, however the impact on spinal biomechanics was not clear (22).
On the other hand, in an osteoporotic animal model alendronic acid was found to be effective in obtaining radiological, biomechanical and histological improvement of the fusion of the vertebral column 23. Alendronate increased the biomechanical strength with internal bone growth in the posterolateral fusion masses in the osteoporotic animals. This study suggests that alendronate can help achieve successful fusion of the spine in animals affected by osteoporosis.
Kim et al. 24 studied the effect of alendronate in 44 patients operated on 1-level instrumented intersomatic lumbar fusion compared to the control group without treatment. They did not find significant differences in terms of bone fusion, and instead there was a higher incidence of vertebral plate degeneration in the alendronate group.
Nagahama 25 published a clinical trial in 40 patients with osteoporosis who underwent intersomatic lumbar fusion and treatment with bisphosphonates. There was an increase in the fusion rate at one year of follow-up in the alendronate group compared to controls (95% vs 65%, respectively), in addition to reducing the presence of subsidence of the prosthesis and the vertebral fracture of the level adjacent. Finally, the authors recommend postoperative treatment with bisphosphonates in all patients with osteoporosis, although they acknowledge that there is still no consensus regarding the use of these drugs.
Park et al. 26 in 2013 evaluated the effect of zoledronic acid in 44 patients with lumbar spinal stenosis operated on posterolateral arthrodesis with instrumentation of 1 or 2 levels, one group received a dose of zoledronic acid and another group control. At 6 months after surgery there was no significant increase in the fusion mass in the single-dose zoledronic acid group demonstrated by 3D computerized tomography. However, there was a significant improvement in the Visual Analogue Scale (VAS) and the Oswestry Functional Scale (OFS) in the zoledronic acid group.
Tu et al. 27 also studied the effect of zoledronic acid on fusion rates in patients with osteoporosis after posterior lumbar interbody fusion at 2 years of follow-up. The zoledronic acid group received an intravenous infusion at 3 and 12 months after surgery. There was a non-statistically significant difference in patients with zoledronic acid with a fusion rate of 75%, compared with 56% in the control group. In addition, there were better VAS and OFS scores, but without being statistically significant in patients receiving zoledronic acid. The rates of pedicle screw loosening were significantly lower in patients with zoledronic acid of 18% compared to 45% in the control group.
Chen et al. 28 conducted a recent randomized clinical trial on the effect of zoledronic acid on bone fusion in patients with osteoporosis after arthrodesis of the lumbar spine. They studied 79 patients with degenerative spondylolisthesis of 1 level. A greater fusion was observed at 3, 6 and 9 months in the zoledronic acid group without being significant at 12 months. Zoledronic acid prevented bone loss induced by immobilization and increased BMD. The authors concluded that zoledronic acid shortens the time to achieve a bone fusion, and prevents subsequent vertebral compression fracture. The limitations were the small sample size and the short follow-up time.
Another randomized clinical trial was conducted by Ohtori et al. 29 in 57 women with osteoporosis and degenerative spondylolisthesis undergoing a posterolateral arthrodesis procedure. One group received risedronate and another parathyroid hormone (teriparatide). The authors found a fusion rate of 82% with PTH and 68% with risedronate; the time frame for carrying out bone fusion was 8 months for PTH and 10 months with risedronate.
In a more recent study, also by Ohtori et al. 30, the effect of teriparatide and risedronate on the incidence of loosening of pedicle screws in patients operated on instrumented posterolateral fusion with local bone graft, specifically in 62 women with degenerative spondylolisthesis and osteroporosis. There was a statistically significant difference in favor of the teriparatide group in the loosening of screws (7-13%) compared with risedronate and the control group (15-26%).
Surgical strategies in the treatment of osteoporotic patients
Given the impact of osteoporosis on spinal fusion interventions, techniques have been developed that can increase the chances of successful vertebral fusion surgery.
In developing these strategies, it is essential to consider the most common forms of instrumentation failure discussed in the previous section 1. These techniques are:
1. Methods that reinforce the segmental vertebral instrumentation
Increase of fixation points. The most common method is to extend the instrumentation with pedicle screws at least 3 levels rostrally and caudally to the compromised level. In this way the stress that is transmitted to several fixation points is reduced; This is especially important in patients over 65 with deformity or osteoporosis 10.
Reports suggest that the addition of wires or sublaminar hooks to the pedicle screws, that is to say hybrid assemblies, can significantly improve the results of an arthrodesis in the osteoporotic spine 31. Although this technique is an effective option, it has not been widely used, probably due to the technical difficulties involved.
Use of cross-link connector. This has been shown that the addition of a transverse connector to the instrumentation with segmental pedicle screws increases the rigidity of the system and prevents the axial rotation of the instrumentation 32. It has also been shown that they increase the resistance to extraction or pullout of the pedicle screws. However, this effect was substantially lower in the osteoporotic column 33.
2. Technical modifications in the placement of screws
Pilot hole size. The creation of a pilot hole is the first step for the insertion of a pedicle screw. It is important to take into account the size of the pilot hole, especially in the osteoporotic bone, since large pilot holes lead to poor grip of the screws, while very small pilot holes can increase the insertion torque, with the consequent risk of pedicle fracture.
Battula et al. 34 attempted to characterize the optimal size of the pilot orifice in the osteoporotic bone. Based on their results, the authors recommend the creation of a pilot hole no larger than 71.5% of the outer diameter for maximum resistance to pullout and minimize iatrogenic fracture of the pedicle, for which a more precise technique is required through high-speed milling, or the use of a punch instead of a gouge.
Preparation of the screw path. Under normal conditions, tapping improves the insertion path of the pedicle screws; however, the tapping influences the grip strength of the pedicle screws in the osteoporotic column.
Halvorson et al. 35 found that the lack of tapping or tapping with diameters below 1 mm of the final diameter of the screw, led to a greater grip strength of the pedicle screw.
Carmouche et al. 36 observed similar results in a study performed on corpses with osteoporotic bone: the tapping with the same diameter of the inserted screw led to a decrease in the pull resistance of the lumbar pedicle screw. On the other hand, the non-tapping or tapping with a lower diameter showed a greater force required for the extraction of the lumbar pedicle screws, although these differences were not replicated with the thoracic pedicle screws.
Bi-cortical fixation of pedicle screws. As it is known, the cortex of the vertebral body is significantly stronger compared to cancellous bone, so that the bi-cortical attachment or hook is stronger than the insertion in the spongy and uni-cortical. However, the bi-cortical fixation technique leads to an additional risk of injury to neurological structures, including the lumbar roots and the sacral sympathetic trunk; in vascular structures, such as the aorta and the vena cava; and in the colon 37.
Fixation with bi-cortical screws is usually carried out ventrally or cranially to the superior plate of S1, where the risk of damaging neurovascular structures is lower. It has been demonstrated that the latter technique significantly increases the torsional force and the extraction of the screw after a cyclic load compared with traditional anteromedially directed fixation 38.
The screws in S1 can also be inserted in what is known as a tricortical trajectory pointing towards the apex of the sacral promontory, so that the screw is inserted or meshed in the posterior cortex and anterosuperior of the superior plate of S1.
Hubbing involves inserting the screw to the head that is embedded or abutted with the dorsal cortical bone of the vertebra, theoretically avoids the windshield-wiper effect of the instrumentation system. However, in a cadaveric biomechanical study of this technique, Paik et al. 39 observed that hubbing led to a reduction of more than 40% in the screw’s extraction force, regardless of BMD, so it was not recommended.
The cortical bone screw is an alternative trajectory of the pedicle screw. The insertion of the pedicle screws with the traditional trajectory from dorsolateral to ventromedial usually implies that the screw thread is located in the cancellous bone of the vertebral body, which in osteoporotic patients may cause poor anchoring. An alternative trajectory introduced in 2009 is the placement of the screw with a dorsomedial to ventrolateral trajectory, in order to couple the screw with more cortical bone of the pars interarticular and of the pedicle (40).
Although the trajectory of the screws placed with the cortical bone tends to be smaller in diameter and shorter in length compared to traditional techniques, it has a reportedly greater insertion torque and a greater extraction force of the screws 41.
Currently, there is only one randomized clinical trial that compared screws in cortical bone with the standard technique 42. At 12 months, the fusion rates evaluated by computerized tomography were similar between the 2 groups (89.5%, n=39, in the conventional pedicle screw group and 92.1%, n=38, in the group of cortical screw), with no differences in pain relief in the leg or scores in the Oswestry disability index. However, subjects subjected to a cortical screw trajectory showed less blood loss, shorter surgical time, and a shorter incision length compared to their counterparts of conventional pedicle screws, probably due to the lack of need to expose beyond the facet joint at the screw insertion points.
3. Modification in pedicle screw design
Increase in the size of the screws. One of the fundamental techniques is the selection of longer instrumentation screws with a larger diameter. It is believed that the larger diameter screws "fill" more the pedicle and allow a better contact of the screw thread with cortical pedicle. In addition to providing a greater surface area of bone in contact with the screw thread and obtain an additional improvement in fixation, particularly in the sacrum. There are several studies that have confirmed that increasing the diameter and length of the screw improve the retention force of the screws 43,44.
Tapered pedicle screws. Changes in the design of the screws have also been considered in terms of morphology and screw threading. The use of conical screws, both with the conical thread and with the center or conical core, are common. If the outside diameter is constant, then the conical core allows a greater contact surface with the thread of the screw in the spongy vertebral body, where the osteoporotic bone has little retention power 45. Screws with a cylindrical outer diameter and conical internal diameter demonstrate a better extraction force compared to other designs.
Cemented screws. One technique that has received considerable attention in recent years is the reinforcement of the pedicle screws through a cement layer or mantle around the screw at the level of the vertebral body. This apparently distributes the tension of the adjacent trabecular bone so that the screws are less prone to loosening or pullout 46 (Figure 3).
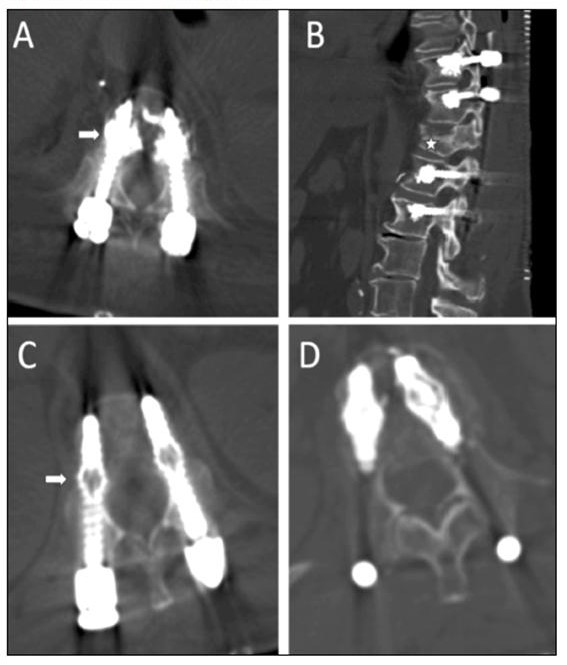
Figure 3. (A) CT axial cut and (B) sagittal pedicular screws are observed with the technique of vertebral reinforcement with cement. (C) and (D) Axial axial CT shows the technique with expandable screws, with part of the expanded screw at the level of the vertebral body (arrow)
This effect was demonstrated more thoroughly with the use of polymethyl methacrylate (PMMA) 47: there is an increase of between 2 to 5 times the force of screw extraction in the osteoporotic vertebrae, a repeated finding in many studies. In the same way, other bioactive cements constituted by calcium sulphate or calcium phosphate have been used with good results 48.
There is a growing experience in the cementation techniques of pedicular screws, and studies on its safety and efficacy have recently been reported and summarized in table 2.
Table 2 Studies that assess the effect of different surgical techniques in patients with osteoporosis

OP: osteoporosis; PMMA: polymethylmethacrylate; X-ray: radiography; CT: computed tomography; 2-, 3-D: bi-tridemensional.
On the other hand, this technique involves risks derived from the use of cement. The main ones are cement extravasation at the venous level, with the consequent possibility of embolism, and extravasation in the spinal canal, with risk of neurological injury. Fortunately, the vast majority of complications are infrequent or asymptomatic 49.
Expandable pedicular screws. Various modifications have been tested in the design of screws for osteoporotic spinal fixation; These include expandable screws and hydroxyapatite-coated screws. The expandable screws have a mechanism that allows the expansion of a part of the screw that is inside the vertebral body, keeping the part of the pedicle intact (Figure 3). The screw compresses the cancellous bone in the vertebral body as it expands, increasing the density of the bone around the screw. It has been possible to improve the pedicle fixation with a 50% increase in the resistance to the extraction of the screw in the osteoporotic bone 50. This effect was magnified when the expandable screw was reinforced with bone cement 51,52. One drawback of this technique is the difficulty involved in revision surgeries that require removing expandable screws.
4. Strategies for the prevention of "proximal joint kyphosis" (PJK)
Regarding PJK prevention strategies, there is no clearly effective solution. Pre-operative assessment of bone mass density is essential and timely correction is possible. Other strategies related to the surgical technique are: the adequate curving of the terminal bar in kyphosis, the placement of hooks in the transverse processes of the superior vertebra of the instrumentation, and the avoidance of finishing the instrumentation in a kyphotic vertebral segment. Minor correction of kyphosis is important but also maintaining an adequate sagittal and coronal balance.
Most authors advocate vertebroplasty at one or two levels higher than the instrumentation to avoid fracture or vertebral collapse in this susceptible segment. Table 3 summarizes the main surgical strategies in the osteoporotic column.
Spinal reinforcement techniques
Vertebroplasty and kyphoplasty are therapeutic procedures that can be included within the so-called "spinal reinforcement techniques" and that are carried out by interventional radiologists, by traumatologists or by neurosurgeons, percutaneously, usually with transpedicular approach. Percutaneous vertebroplasty involves introducing a bone cement, such as polymethylmethacrylate (PMMA), in a fractured vertebral body, to relieve pain by reinforcing and stabilizing the vertebral fracture (Figure 4). Similar to vertebroplasty, in percutaneous kyphoplasty, prior to the administration of cement at the level of the fractured vertebra, a balloon is inserted that is inflated to restore the height of the vertebral body and reduce kyphotic deformity. When the balloon is removed, a cavity or nest remains inside the vertebral body, allowing the cement to be introduced at a lower pressure and with a higher viscosity, which reduces the risk of extravasation. Some authors prefer to call kyphoplasty "balloon vertebroplasty" 53.

Figure 4 MRI sequence T2 (A) and (B) T1: vertebral fracture is observed by acute compression at level D7 ,with vertebral body edema. (C) Lateral X-ray of the dorsal spine shows vertebral wedging at level D7 with discrete segmental kyphosis. (D) Vertebroplasty of the fractured level with improvement of segmental kyphosis. (E) Lateral X-ray of follow-up, refracture with vertebral collapse of D7 and a significant segmental kyphosis is observed. (F) Rescue surgery by arthrodesis with cemented pedicle screws from D5 to D9, with correction of kyphosis
As has been amply demonstrated in the literature and as it has been assured by different scientific societies, the use of vertebroplasty or kyphoplasty is a safe, effective and lasting procedure in selected patients with symptomatic osteoporotic and neoplastic fractures, as long as it is carried out according to published standards. These procedures must be offered when non-surgical medical treatment has not provided adequate pain relief and this is significantly altering the quality of life of the patient 54.
Multiple case series, retrospective and nonrandomized prospective studies and, more recently, randomized controlled trials, have shown how these techniques achieve statistically significant improvements in pain and function, particularly in ambulation, with respect to medical treatment 54.
There are currently a total of six randomized controlled trials, including a total of 842 patients, in which the vertebral reinforcement treatment, vertebroplasty or kyphoplasty, is compared with medical or simulated non-surgical treatment in osteoporotic vertebral fractures 54 (Table 4).
Table 4 Randomized controlled trials comparing vertebral reinforcement treatment, vertebroplasty or kyphoplasty, with medical or simulated non-surgical treatment, in osteoporotic

RPCS: randomized and prospective controlled studies; VAS: Visual Analog Scale; VFC: vertebral fracture-compression; FREE: Fracture Reduction Evaluation Trial; INVEST:
Investigational Vertebroplasty Safety and Efficacy Trial; MRI: magnetic resonance.
The two randomized controlled trials with the largest number of patients studied have shown benefits for vertebroplasty and kyphoplasty that last up to 1 year after the intervention 55,56. Supporting these results, another study showed significant benefits for vertebroplasty that persisted up to 3 years after treatment 57. On the other hand, other investigations have reported benefits of vertebroplasty up to 1 month after intervention, but not beyond this point 58,61. The INVEST clinical trial showed a very significant trend towards clinical improvement in relation to pain for the group treated by vertebroplasty at the first month of treatment, despite the fact that no statistically significant differences were achieved 59. On the other hand, only one study failed to demonstrate that vertebroplasty treatment was beneficial after the first month after surgery 60. Therefore, based on these studies, we may conclude that vertebral reinforcement treatments in osteoporotic vertebral fractures are clearly beneficial in the short term and probably also in the long term 54 (Table 4).
Conclusions
The progressive aging of the population has significantly increased the procedures of spinal fusion. The prevalence of osteoporosis in patients who undergo surgery ranges to around 50% in women over 50 years of age. A significant proportion of these patients are not adequately diagnosed with osteoporosis or vitamin D deficiency and, therefore, receive no timely treatment. There is evidence that patients with osteoporosis and with uncorrected hypovitaminosis D have worse results in cervical and lumbar disability scales. Patients with osteoporosis, having a poor bone mineral density, suffer from worse rates of bone fusion in spine arthrodesis.
Surgical complications are more frequent in patients with osteoporosis, especially in those who do not receive timely treatment and the relevant surgical technique modifications are not made.
Currently, a variety of pharmacological and surgical medical treatment strategies are available that can improve clinical outcomes and fusion rates of patients undergoing spinal fusion.
Bibliografía
1. Goldstein CL, Brodke DS, Choma T J. Surgical management of spinal conditions in the elderly osteoporotic spine. Neurosurgery. 2015;77:S98-107. [ Links ]
2. Díaz Curiel M, García JJ, Carrasco JL, Honorato J, Cano R, Rapado A, Sanz C. Prevalencia de osteoporosis determinada por densitometría en la población femenina española. Med Clín (Barc). 2001;116(3):86-8. [ Links ]
3. Chin DK, Park JY, Yoon YS, Kuh SU, Jin BH, Kim KS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int. 2007;18(9):1219-24. [ Links ]
4. Lubelski D, Choma TJ, Steinmetz MP, Harrop JS, Mroz TE. Perioperative medical management of spine surgery patients with osteoporosis. Neurosurgery. 2015;7:S92-7. [ Links ]
5. Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR. Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J. 2009;9(7):537-44. [ Links ]
6. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Influence of bone mineral density on pedicle screw fixation: a study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001;1(6):402-7. [ Links ]
7. Vanderpool DW, James JIP, Wynne-Davies R. Scoliosis in the elderly. J Bone Joint Surg. 1969;51:446-55. [ Links ]
8. Dennison E, Cooper C. Epidemiology of osteoporotic fractures. Horm Res. 2000;54(suppl 1):58-63. [ Links ]
9. Grubb SA, Lipscomb HJ, Coonrad RW. Degenerative adult onset scoliosis. Spine (Phila Pa 1976). 1988;13:241-5. [ Links ]
10. DeWald CJ, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976). 2006;31(Suppl 19):S144-51. [ Links ]
11. Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976). 1990;15(9):902-7. [ Links ]
12. Hitchon PW, Brenton MD, Coppes JK, From AM, Torner JC. Factors affecting the pullout strength of self-drilling and self-tapping anterior cervical screws. Spine (Phila Pa 1976). 2003;28(1):9-13. [ Links ]
13. Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, et al. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine (Phila Pa 1976). 2001;26(8):951-6. [ Links ]
14. Healy JH, Lane JM. Structural scoliosis in osteoporotic women. Clin Orthop. 1985;195:216-23. [ Links ]
15. Chesnut CH III, Silverman S, Andriano K, Genant H, Gimona A, Harris S, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the prevent recurrence of osteoporotic fractures study. Am J Med. 2000;109:267-76. [ Links ]
16. Cook SD, Salkeld S, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw. Fixation in severely osteoporotic bone. Spine J. 2004;4:402-8. [ Links ]
17. Hu SS. Internal fixation of the osteoporotic spine. Spine (Phila Pa 1976). 1997;22(Suppl 24):S43-8. [ Links ]
18. Brodke DS, Bachus KN, Mohr RA, Nquyen BKl. Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs: a biomechanical analysis. Spine J. 2001;1:373-9. [ Links ]
19. Yagi M, Akilah KB, Boachie-Adjei. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36(1):E60-8. [ Links ]
20. Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 2013;38(23):E1469-76. [ Links ]
21. Slimack NP, Bae HW. Commentary: Therapies for osteoporosis: are they good for spinal fusion. Spine J. 2013;13(2):200-1. [ Links ]
22. Hirsch, BP, Unnanuntana A, Cunningham ME, Lane JM. The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J. 2013;13(2):190-9. [ Links ]
23. Nakao S, Minamide A, Kawakami M, Boden SD, Yoshida M. The influence of alendronate on spine fusion in an osteoporotic animal model. Spine (Phila Pa 1976). 2011;36:1446-52. [ Links ]
24. Kim TH, Yoon JY, Lee BH, Jung HS, Park MS, Park JO, et al. Changes in vitamin D status after surgery in female patients with lumbar spinal stenosis and its clinical significance. Spine (Phila Pa 1976). 2012;37(21):E1326-30. [ Links ]
25. Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A. Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial: Clinical article. J Neurosurg Spine. 2011;14(4):500-7. [ Links ]
26. Park YS, Kim HS, Baek SW, Kong DY, Ryu JA. The effect of zoledronic acid on the volume of the fusion-mass in lumbar spinal fusion. Clin Orthop Surg. 2013;5(4):292-7. [ Links ]
27. Tu CW, Huang KF, Hsu HT, Li HY, Yang SS, Chen YC. Zoledronic acid infusion for lumbar interbody fusion in osteoporosis. J Surg Res. 2014;192(1):112-6. [ Links ]
28. Chen F, Dai Z, Kang Y, Lv G, Keller ET, Jiang Y. Effects of zoledronic acid on bone fusion in osteoporotic patients after lumbar fusion. Osteoporos Int. 2016;27(4):1469-76. [ Links ]
29. Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine (Phila Pa 1976). 2012;37(23):E1464-8. [ Links ]
30. Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine (Phila Pa 1976). 2013;38(8):E487-92. [ Links ]
31. Tan JS, Kwon BK, Dvorak MF, Fisher CG, Oxland TR. Pedicle screw mo-tion in the osteoporotic spine after augmentation with laminar hooks, sublaminar wires, or calcium phosphate cement: a comparative analysis. Spine (Phila Pa 1976). 2004;29(16):1723-30. [ Links ]
32. Brodke DS, Bachus KN, Mohr RA, Nguyen BK. Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs. a biomechanical analysis. Spine J. 2001;1(5):373-9. [ Links ]
33. Suzuki T, Abe E, Okuyama K, Sato K. Improving the pullout strength of pedicle screws by screw coupling. J Spinal Disord. 2001;14(5):399-403. [ Links ]
34. Battula S, Schoenfeld AJ, Sahai V, Vrabec GA, Tank J, Njus GO. The effect of pilot hole size on the insertion torque and pullout strength of self-tapping cortical bone screws in steoporotic bone. J Trauma. 2008;64(4):990-5. [ Links ]
35. Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS III, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415-20. [ Links ]
36. Carmouche JJ, Molinari RW, Gerlinger T, Devine J, Patience T. Effects of pilot hole reparation technique on pedicle screw fixation in different regions of the osteoporotic thoracic and lumbar spine. J Neurosurg Spine. 2005;3(5):364-70. [ Links ]
37. Ponnusamy KE, Iyer S, Gupta G, Khanna AJ. Instrumentation of the osteoporotic spine: biomechanical and clinical considerations. Spine J. 2011;11(1):54-63. [ Links ]
38. Luk KD, Chen L, Lu WW. A stronger bicortical sacral pedicle screw fixation through the s1 endplate: an in vitro cyclic loading and pull-out force evaluation. Spine (Phila Pa 1976). 2005;30(5):525-9. [ Links ]
39. Paik H, Dmitriev AE, Lehman RA Jr, Gaume RE, Ambati DV, Kang DG, et al. The biomechanical effect of pedicle screw hubbing on pullout resistance in the thoracic spine. Spine J. 2012;12(5):417-24. [ Links ]
40. Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366-73. [ Links ]
41. Inceoglu S, Montgomery WH Jr, St Clair S, McLain RF. Pedicle screw in-sertion angle and pullout strength: comparison of 2 proposed strategies. J Neurosurg Spine. 2011;14(5):670-6. [ Links ]
42. Lee GW, Son JH, Ahn MW, Kim HJ, Yeom JS. The comparison of pedicle screw and cortical screw in posterior lumbar interbody fusion: a prospective randomized noninferiority trial. Spine J. 2015;15(7):1519-26. [ Links ]
43. Brantley AG, Mayfield JK, Koeneman JB, Clark KR. The effects of pedicle screw fit. An in vitro study. Spine (Phila Pa 1976). 1994;19(15):1752-8. [ Links ]
44. Bianco RJ, Arnoux PJ, Wagnac E, Mac-Thiong JM, Aubin CE. Minimizing pedicle screw pullout risks: a detailed biomechanical analysis of screw design and placement. Clin Spine Surg. 2017;30(3):E226-32. [ Links ]
45. Kim YY, Choi WS, Rhyu KW. Assessment of pedicle screw pullout strength based on various screw designs and bone densities-an ex vivo biomechanical study. Spine J. 2012;12(2):164-8. [ Links ]
46. Pfeifer BA, Krag MH, Johnson C. Repair of failed transpedicle screw fixation. A biomechanical study comparing polymethylmethacrylate, milled bone, and matchstick bone reconstruction. Spine (Phila Pa 1976). 1994;19(3):350-3. [ Links ]
47. Aydogan M, Ozturk C, Karatoprak O, Tezer M, Aksu N, Hamzaoglu A. The pedicle screw fixation with vertebroplasty augmentation in the surgical treatment of the severe osteoporotic spines. J Spinal Disord Tech. 2009;22(6):444-7. [ Links ]
48. Choma TJ, Frevert WF, Carson WL, Waters NP, Pfeiffer FM. Biomechanical analysis of pedicle screws in osteoporotic bone with bioactive cement augmentation using simulated in vivo multicomponent loading. Spine (Phila Pa 1976). 2011;36(6):454-62. [ Links ]
49. Kerry G, Ruedinger C, Steiner HH. Cement embolism into the venous system after pedicle screw fixation: case report, literature review, and prevention tips. Orthop Rev (Pavia). 2013;5(3):E24. [ Links ]
50. Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4(4):402-8. [ Links ]
51. Cook SD, Salkeld SL, Whitecloud TS III, Barbera J. Biomechanical evaluation and preliminary clinical experience with an expansive pedicle screw design. J Spinal Disord. 2000;13(3):230-6. [ Links ]
52. Gao M, Lei W, Wu Z, Liu D, Shi L. Biomechanical evaluation of fixation strength of conventional and expansive pedicle screws with or without calcium based cement augmentation. Clin Biomech (Bristol, Avon). 2011;26(3):238-44. [ Links ]
53. Martínez-Quiñones JV, Aso-Escario J, Arregui-Calvo R. Refuerzo vertebral percutáneo: vertebroplastia y cifoplastia. Procedimiento técnico. Neurocirugía. 2005;16:427. [ Links ]
54. Barr JD, Jensen ME, Hirsch JA, McGraw JK, Barr RM, Brook AL, et al. Position statement on percutaneous vertebral augmentation: a consensus statement developed by the Society of Interventional Radiology (SIR), American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS), American College of Radiology (ACR), American Society of Neuroradiology (ASNR), American Society of Spine Radiology (ASSR), Canadian Interventional Radiology Association (CIRA), and the Society of NeuroInterventional Surgery (SNIS). J Vasc Interv Radiol. 2014;25:171-81. [ Links ]
55. Wardlaw D, Cummings SR, Van Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373:1016-24. [ Links ]
56. Klazen CAH, Lohle PNM, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (VERTOS II): an open-label randomised trial. Lancet. 2010;376:1085-92. [ Links ]
57. Farrokhi MR, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine. 2011;14:561-9. [ Links ]
58. Rousing R, Hansen KL, Andersen MO, Jespersen SM, Thomsen K, Lauritsen JM. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine (Phila Pa 1976). 2010;35:478-82. [ Links ]
59. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-79. [ Links ]
60. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-68. [ Links ]
61. Rousing R, Andersen MO, Jespersen SM, Thomsen K, Lauritsen J. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-month follow-up in a clinical randomized study. Spine (Phila Pa 1976). 2009;34:1349-54. [ Links ]











 texto en
texto en 



