INTRODUCTION
Vestibular schwannoma (VS), also known as acoustic neurinoma, is a benign tumor that grows from Schwann cells [1] and affects the eighth cranial nerve [2, 3]. It has an incidence of 1-2 cases per 100,000 people/year, and it affects both genders equally. It occurs most frequently in middle-aged people (between 30 and 50 years) [4, 5].
Given its location, the most characteristic symptoms are progressive or sudden hearing loss, tinnitus, instability, or balance disorders [6]. If the SV continues growing, it may affect other cranial nerves and may cause symptoms of raised intracranial pressure [7].
The cause and risk factors of VS are unknown, but when they are located on both sides, the cause may be a hereditary disease (neurofibromatosis type 2) [6, 8].
Clinical suspicion appears with anamnesis, physical examination, audiologic evaluation, and vestibular tests. However, magnetic resonance imaging (MRI) is required for a precise diagnosis and to plan the subsequent treatment [9].
The treatment of VS depends on the symptoms it produces, its size, its growth rate, and the age of the patient. In case of large VS, and/or when there are symptoms that have an impact on the quality of life, a surgical removal of the tumor may be necessary. The main objectives in this case are the complete resection of the tumor and reaching a postoperative mortality and morbidity close to zero [10-13].
According to the literature, the incidence and duration of the symptoms are not related to the size of the tumor, and the most common symptoms are due to the involvement of the acoustic pathway of the eighth cranial nerve [14]. The most common reason for consultation is progressive hearing loss (related or unrelated to tinnitus), which is also the symptom which is most frequently found [15, 16].
The main objective of this study is analyzing the hearing loss in patients with VS and determining the extent to which the tumor grade and the hearing loss are related.
Our secondary objectives are establishing the clinical characteristics of patients with VS, determining the most common clinical symptoms, and comparing the degree of hearing loss based on the symptom that was reported as a reason for consultation.
MATERIAL AND METHODS
Study population
An observational retrospective study was conducted with a sample of 291 patients diagnosed with VS between 1995 and 2017 in the Department of Otorhinolaryngology and Head and Neck Surgery of the Tertiary Care Primary Center of Salamanca.
The symptoms reported by the patient as the reason for consultation were registered, that is, those symptoms that were present at diagnosis, and the following categories were established: progressive unilateral hearing loss (related or unrelated to tinnitus), sudden unilateral hearing loss (related or unrelated to tinnitus), instability, vertigo, paresthesia, pain, facial nerve paralysis and other symptoms (unspecified alterations, muscle weakness, visual alterations). Those symptoms are grouped into the following: progressive unilateral hearing loss, sudden unilateral hearing loss, tinnitus, instability, vertigo, and others.
The symptoms presented by the patients during the follow-up were also registered and classified in the categories mentioned above.
About the risk factors, they are grouped into the following: minor cardiovascular factors (arterial hypertension (AHT), diabetes mellitus (DM), hyperlipidemia (HL) and tobacco consumption [17, 18]), major cardiovascular factors (heart rhythm disorders, thrombosis, ischemia), exposure to noises (job-related), other risks (stress, thyroid disease) and neurological factors.
The age of the patients was grouped into the following categories: under 25, 25-50, 50-75 and over 75 years old.
Functional tests and physical examination
All the patients underwent the same clinical tests, including a complete neurological exam, audiometry and logoaudiometry, electrical facial nerve test, magnetic resonance (MRI) and videonystagmography (VNG). From 2012 onwards, the video head impulse test (VHIT) was also conducted. The audiometry calculates the pure tone average (PTA) and classifies it as normal (<20dB), or with hearing loss that may be mild (20-40 dB), moderate (40-70 dB), severe (70-90 dB) and profound (>90 dB). The logoaudiometry was performed and the ipsilateral and contralateral reflex of both ears were also registered.
Imaging test
Both the size and the composition of the tumor were determined by magnetic resonance imaging (MRI) and grouped according to the Koos grading scale (I: intracanalicular; II: protrusion into the cerebellopontine angle (CPA); III: the tumor reaches the brainstem; IV: there is brainstem displacement) [19]. In all cases, the size of the tumor was registered considering its largest diameter in millimeters. The composition was analyzed and divided into heterogeneous or homogeneous.
Study analysis and design
The hearing loss of the patient was analyzed as the dependent variable by measuring the PTA prior to surgery.
A statistical analysis was conducted with IBM SPSS Statistics (version 21.0), starting with a descriptive study of the symptoms and the hearing level of all the patients and those who presented hearing loss. Then, a discriminant analysis was carried out with two-way contingency tables for qualitative variables and a chi-squared test through a paired study of the PTA (dependent variable, classified as normal, mild, moderate, severe, or profound) and the size of the tumor (grouped in grades I-IV) for the patients who reported hearing loss as a reason for consultation.
RESULTS
Clinical characteristics of the patients who present VS (N=292)
The most common reason for consultation at diagnosis was progressive unilateral hearing loss (31.6%), followed by instability (24.9%), vertigo (19.3%), sudden hearing loss (9.5%), isolated tinnitus (9.1%) and other symptoms (5.6%) (Figure 1).
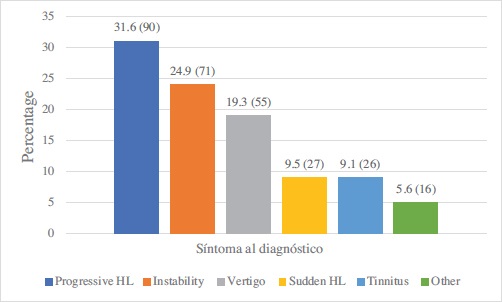
Figure 1. Descriptive study of the reasons for consultation of patients with VS. The number over each bar represents the percentage, and the number in brackets shows the frequency. (HL= Hearing Loss).
During the follow-up, most patients (54.5%) presented associated symptoms that were different from the reason for consultation. 92 patients (32.2%) developed progressive hearing loss, which they had not presented before, followed by other symptoms (5.8%), isolated tinnitus (5.6%), instability (2.8%), vertigo (2.8%) and sudden hearing loss (1.4%). In 45.5% of the cases, no additional symptoms appeared during the follow-up (Figure 2).
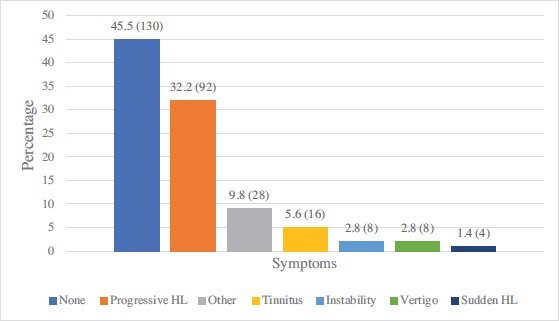
Figure 2. Descriptive study of the symptoms during the follow-up of the patients with VS. The number over each bar represents the percentage, and the number in brackets shows the frequency. (HL= Hearing Loss).
An analysis of the hearing level via PTA only among patients who reported progressive hearing loss as a reason for consultation, with or without tinnitus, revealed that the hearing loss was mild in 13.7% of the patients (n=10), moderate in 45.2% of the patients (n=33), severe in 13.7% of the patients (n=10) and profound in 20.5% of the cases (n=15). Hearing was within normal limits in 6.8% of the patients (n=5).
About the relationship between the size of the VS and hearing loss in the patients who reported progressive unilateral hearing loss as a reason for consultation, with or without tinnitus, no statistically significant association was observed (p=0.099) (Table 1). An analysis of the relationship between the VS grade and the degree of hearing loss in patients who present hearing loss at any time, both at diagnosis and during follow-up, does not reveal a statistically significant association (p=0.083) (Table 2).
Table 1. Relationship between the size of the VS and hearing loss in patients with progressive hearing loss as reason for consultation. P-value=0.099.
|
|
Grade of the SV |
Total |
||||
|---|---|---|---|---|---|---|
|
I |
II |
III |
IV |
|||
|
PTA |
Normal |
1 |
2 |
0 |
1 |
4 |
|
Mild |
3 |
3 |
3 |
1 |
10 |
|
|
Moderate |
12 |
10 |
5 |
5 |
32 |
|
|
Severe |
1 |
5 |
2 |
1 |
9 |
|
|
Profound |
2 |
1 |
3 |
8 |
14 |
|
|
Total |
19 |
21 |
13 |
16 |
69 |
|
Tabla 2. Relationship between the size of the VS and hearing loss in patients with progressive hearing loss at any time during the study. P-value=0.083.
|
|
Grade of the SV |
Total |
||||
|---|---|---|---|---|---|---|
|
I |
II |
III |
IV |
|||
|
PTA |
Normal |
2 |
3 |
0 |
2 |
7 |
|
Mild |
6 |
7 |
4 |
4 |
21 |
|
|
Moderate |
17 |
21 |
12 |
14 |
64 |
|
|
Severe |
3 |
7 |
4 |
2 |
16 |
|
|
Profound |
2 |
3 |
3 |
13 |
21 |
|
|
Total |
30 |
41 |
23 |
35 |
129 |
|
The tumor grade was transformed into a dichotomic variable by grouping grades I and II into one category and grades III and IV into another, and we observed that the relationship between the size of the tumor and hearing loss was statistically significant, both for patients who presented progressive hearing loss at diagnosis (p=0.042) and for those who presented it either at diagnosis or during the follow-up (p=0.036) (Table 3).
Tabla 3. Relationship between the size of the VS and hearing loss in patients with progressive hearing loss at diagnosis and during follow-up. P-value=0.036.
|
Patients with progressive hearing loss at diagnosis |
Grade of the SV |
Total |
P-valor |
||
|---|---|---|---|---|---|
|
I, II |
III, IV |
||||
|
PTA |
Normal |
3 |
1 |
4 |
0.036 |
|
Mild |
6 |
4 |
10 |
||
|
Moderate |
22 |
10 |
32 |
||
|
Severe |
6 |
3 |
9 |
||
|
Profound |
3 |
11 |
14 |
||
|
Total |
40 |
29 |
69 |
||
|
Patients with progressive hearing loss during follow-up |
|
|
|
||
|
I, II |
III, IV |
||||
|
PTA |
Normal |
5 |
2 |
7 |
0.042 |
|
Mild |
13 |
8 |
21 |
||
|
Moderate |
38 |
26 |
64 |
||
|
Severe |
10 |
6 |
16 |
||
|
Profound |
5 |
16 |
21 |
||
|
Total |
71 |
58 |
129 |
||
DISCUSSION
This study analyzed the symptoms for consultation of patients who were diagnosed with VS. The most common reason for consultation was progressive unilateral hearing loss, which was also the most frequently associated symptom when it appeared. We have observed that patients who consulted with progressive hearing loss or any type of hearing loss (either progressive or sudden) as an initial symptom, already presented an average hearing loss of over 40 dB, which was moderate in most cases. We can highlight that the hearing loss presented by the patients, both at diagnosis and during the follow-up, was not significantly related with the size of the tumor. According to previous authors, the degree of hearing loss is not related to the tumor growth [20] and it is not a predictive factor for its size. For this reason, the dissociation between the tumor size and symptoms is generally mentioned as a typical feature of VS [21-23]. However, in our study, when the tumor grades were grouped into two categories, we observed that, in the case of grades III and IV, patients showed associated severe and profound hearing loss more often than patients with tumors in grades I and II, who presented, in turn, more cases of mild hearing loss or normal hearing.
Although progressive unilateral hearing loss is the most common symptom among patients with VS, the initial symptoms may be very varied, and none of them are associated with the stage of the tumor [24]. There is no typical clinical pattern for the initial symptoms in schwannomas of the eighth cranial nerve. Any audiovestibular or even facial symptom, no matter how subtle, may be the first clinical expression of a schwannoma of the eighth cranial nerve, and should be adequately examined. No symptom is exclusive of a specific stage, except for the symptoms that affect the posterior fossa [24-27].
Previous studies which analyze the hearing loss classified into different frequencies have concluded that the lowest frequencies (500 Hz) were characteristic of larger tumors [28]. Del Río et al. analyzed 81 neurinomas and observed that the most affected frequency was 8000 Hz, and that the largest drop in interaural difference occurred at 4000 Hz. As in our study, they did not find a significant association between the degree of hearing loss and the size of the tumor. They also concluded that the lack of corneal reflex and a poorer preoperative facial function were significantly related to a higher degree of hearing loss, but not to the size of the tumor. When they analyzed the volume instead of the maximum diameter, the relationship with the facial function and the preoperative hearing loss degree became more intense, but this did not change the fact that the symptoms caused by VS were independent from its size [29]. Similarly, other studies have concluded that there are neurinomas that affect more frequently the adjacent cranial nerves, but the mechanism that causes this involvement is independent from the size of the tumor, and the main aspect related to the involvement of the cranial nerves is their level of adhesion to the tumor, a factor that is not known until the surgery is performed [29-33].
CONCLUSIONS
The most common reason for consultation in VS is progressive unilateral hearing loss. However, this initial symptom may be very varied, and it is not directly related to a specific size of the tumor or a typical clinical pattern that appears at the onset of symptoms. The hearing loss caused by VS does not have a statistically significant association with any tumor grade, although severe and profound hearing loss is more commonly associated with grade III-IV neurinomas, whereas mild hearing loss or normal hearing are more likely in grade I-II tumors. We must underline here the importance of requesting an MRI for the final diagnosis of VS, because there is no typical hearing loss or clinical pattern which can provide a diagnosis by itself.














