Introduction
The prevalence of obesity has risen in the past three decades, becoming a worldwide epidemic(1). In 2016, according to the World Health Organization (WHO), over 650 million adults (18 years and older) had obesity(2). Data from the National Health and Nutrition Survey (NHANES) reported a prevalence of obesity among United States (U.S.) adults of 39.8% in 2015-2016(3). Since the 1970s, obesity trends have been increasing in the U.S. regardless of ethnicity, race, age, or gender(4).
Numerous interventions and treatments have been developed to halt the progression of obesity. Metabolic and bariatric surgery (MBS) has become one of the most commonly performed and approved therapies for severe obesity(5,6). Substantial weight loss, remission or improvement of related comorbidities have been widely demonstrated(7-12). Recent research has proven a superior and persistent effect of MBS than medical treatment in medium and long-term periods(13). However, despite the outcomes regarding shortand medium-term weight loss after MBS, treatment failures (≤50% excess weight loss)(14,15) can reach up to 5-20% in gastric bypass and gastric sleeve(16,17), and 14-63% in gastric band(18).
Several non-surgical factors have been identified to be associated with poor weight loss outcomes, weight regain, and weight loss maintenance over time. Associated factors include a variety of demographic, patient-related diseases, and behavioral characteristics, from which older age, greater preoperative weight, obesity-related diseases, physical inactivity, poor followup after surgery, self-efficacy, psychosocial and behavioral patterns have been demonstrated to play an important role(19-22). Maladaptive eating behaviors (MEB) are highly prevalent among bariatric surgery patients and have been reported to be much higher compared to the general population(23). The most common MEB reported in the literature are binge eating, emotional eating, uncontrolled eating, eating in absence of hunger, recurrent episodes of nocturnal eating, and continuous snaking or grazing patterns(24). These problematic eating patterns have been demonstrated to be significant predictors of poor weight outcomes(25). MEB are associated with an increased caloric intake, which causes less weight loss, weight regain, and attenuated longterm weight loss can ultimately cause treatment failure(24,26-28). The association between preoperative MEB and weight loss outcomes after surgery have yielded inconsistent results, while there is consistent evidence of postoperative MEB negatively affect weight loss results(29). However, in the last years, research has been increasing evaluating the impact that have preoperative MEB, specially binge eating, on postoperative outcomes. A recent study reported that patients that presented higher levels of pre-operative emotional eating and food addiction symptoms had poorer weight loss 1 year after follow-up(30). In addition, other psychological factors (depression, anxiety and drug abuse) are also associated with weight loss outcomes and adherence to surgical protocols(31).
Behavioral interventions including psychotherapy have been implemented in bariatric surgery patients before and/or after surgical treatment to improve MEB, better compliance to dietary guidelines, weight maintenance, and to optimize weight loss after surgery. Psychological interventions are characterized by a large variety of therapies, ranging from individual and group therapy to support groups(32). Previous systematic reviews which evaluated behavioral management including psychotherapeutic interventions and support groups in bariatric surgery patients have demonstrated a positive effect on weight loss outcomes(32-34). Most of the psychological treatment approaches developed for improvement of MEB implement or are based on principles of cognitive behavioral therapy (CBT), acceptance-commitment therapy, mindfulness, adapted motivational interviewing, and psychoeducational groups. These therapeutic strategies provide skills to regulate eating patterns, stimulate self-control, create assertiveness/problem-solving skills, increase self-esteem and motivation to change(35,36).
The aim of this systematic review is to evaluate the effectiveness of preor postoperative psychological treatment approaches on MEB in bariatric surgery patients.
Methods
Protocol and Registration
The protocol of the present study was registered at the international database of prospectively registered systematic reviews in health and social care (PROSPERO), the registration number is CRD42018108443.
Literature search strategy
The present study was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) recommendations(37). A comprehensive literature review was performed in the databases MEDLINE (PubMed), ScienceDirect, Cochrane Library, and Web of Science. Additionally, we performed a manual review of the reference list of retrieved articles for any other related study not included in our database search. Literature search was limited to include studies between January 1st 1990 and October 18th 2019. The following combinations of search terms were used: “psychotherapy” OR “psychotherapeutic” OR “psychological” OR “psychosocial” OR “behavioral” OR “behavioral interventions” OR “behavioral therapy” OR “cognitive” OR “cognitive intervention” OR “mindfulness” OR mindfulness interventions” AND “bariatric surgery” OR “weight loss surgery” OR “bypass” OR “gastric sleeve” OR “gastric band”. The literature search was conducted by two reviewers (PRC and CIFG). The last search was conducted on October 18th, 2019.
Study selection and inclusion criteria
Randomized controlled trials (RCT) and pretest-posttest studies were included based on the following inclusion criteria:
Aged ≥18 years with a minimum follow-up period equal or greater than four weeks.
Bariatric surgery patients (patients who underwent bariatric surgery or bariatric surgery candidates or subjects in a bariatric surgery program).
Studies that performed preor postoperative psychological treatment approaches aimed to improve MEB.
Studies that reported preand post-intervention outcomes on MEB or problematic eating patterns, including binge eating, emotional eating, uncontrolled eating, eating in absence of hunger, night-eating, grazing, snacking, picking patterns, etc.
Data extraction and quality assessment
All data extraction was performed by the first author and double-checked by two other authors (CIFG and MBG). Discrepancies were solved though consultation and consensus. Data was collected from the full-text articles and was pooled. Data regarding the study design, sample size, participant's characteristics (mean age and gender), follow-up period, retention rate, type of intervention, and outcomes measured were obtained (Table 1). Data was organized according to the study design (i.e. RCT and pretest-posttest studies) and by the period of intervention (preor postoperative intervention). Primary outcomes analyzed were MEB and secondary outcomes were weight loss, anxiety and depression symptoms. When there was more than one publication of the same study population, the articles where combined and information was collected from the article that reported the primary outcomes and that had the longest follow-up. Effect size of the primary outcomes (MEB) was extracted from the studies when available, when not reported and data was available, Cohen d effect size was calculated.
Table 1. Study characteristics.
| Author | Country | Type of study | Sample size | Mean age ± SD | Follow-up, mo ± SD | Retention rate (%) | Type of psychological treatment approach | Outcomes measured | Effect size of MEB | Group differences (p) |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention after surgery | ||||||||||
| Wild et al. 2017, 2015 | Germany | RCT | 74 (female 68.9%) | 41.4 ± 8.8; 41.3 ± 9.8 | 37.9 ± 8.2 | 63.2 | Videoconferencing-based psychoeducational group | Eating disorder | - | 0.65 |
| Quality of life | - | 0.65 | ||||||||
| Self-efficacy | Medium | 0.03 | ||||||||
| Depression severity | 0.03 | |||||||||
| Weight loss | 0.82 | |||||||||
| Chacko et al., 2016 | Israel | RCT | 18 (female 83.3%) | 53.4 ± 5.6; 54.5 ± 7.8 | 6 | 100 | Mindfulness-based | Emotional eating | N/A | 0.03 |
| Binge eating | - | 0.47 | ||||||||
| Cognitive restraint | - | 0.27 | ||||||||
| Uncontrolled eating | - | 0.98 | ||||||||
| Eating self-efficacy | - | 0.64 | ||||||||
| Quality of life | 0.30 | |||||||||
| Depression | 0.74 | |||||||||
| Perceived stress | 0.43 | |||||||||
| Weight loss | 0.28 | |||||||||
| Weineland et al., 2012 | Sweden | RCT | 39 (female 89.7%) | 43.9; 42.3 | 1.4 | 84 | Acceptance and commitment therapy | Eating disorder-general | Medium | 0.047 |
| Eating disorder-shape concerns | Large | 0.009 | ||||||||
| Eating disorder-weight concerns | Medium | 0.03 | ||||||||
| Eating disorder-restraint eating | 0.55 | |||||||||
| Eating disorder-eating concerns | - | 0.42 | ||||||||
| Binge eating | Large | 0.006 | ||||||||
| Self-perceived body dissatisfaction | Medium | 0.023 | ||||||||
| Acceptance of weight | Large | 0.006 | ||||||||
| Quality of life | 0.022 | |||||||||
| David et al., 2016 | Canada | RCT | 51 (female 87%) | 49.2 ± 9.1 | 2.8 | 90.2 | Adapted motivational interviewing | Binge eating | Medium | <0.01 |
| Self-efficacy | - | NS* | ||||||||
| Confidence to change | Small | <0.05 | ||||||||
| Papalazarou et al., 2010 | Greece | RCT | 30 (female 100%) | 32.7 ± 1.6; 33.4 ± 2.0 | 36 | 100 | Lifestyle intervention including elements of CBT | Eating behavior-restrained eating | Large | <0.001 |
| Eating behavior-emotional eating | - | 0.858 | ||||||||
| Eating behavior-eating in response to external food-related stimuli | Large | <0.001 | ||||||||
| PAL | 0.001 | |||||||||
| Weight loss | <0.001 | |||||||||
| Beaulac and Sandre, 2015 | Canada | Pre-post | 17 (female 88.2%) | 48 ± 9.5 | 3 | 100 | CBT | Emotional overeating | Medium | 0.05 |
| Anxiety and depression | 0.78 | |||||||||
| Perceived difficulties in their lives | 0.009 | |||||||||
| Feelings in relation to their weight, relationships, and activities | 0.018 | |||||||||
| Psychological distress | 0.0001 | |||||||||
| Wnuk et al., 2018 | Canada | Pre-post | 22 (female 100%) | 55.4 ± 9.4 | 4 | 77.3 | Mindfulness-based eating and awareness training | Binge eating | - | 0.16 |
| Emotional eating-anger | - | 0.16 | ||||||||
| Emotional eating-anxiety | Small | 0.07 | ||||||||
| Emotional eating-depression | - | 0.30 | ||||||||
| Depression | 0.76 | |||||||||
| Anxiety | 0.11 | |||||||||
| General emotion regulation | 0.04 | |||||||||
| Weight loss | 0.94 | |||||||||
| Bradley et al., 2016 | USA | Pre-post | 11 (female 63.6%) | 53.4 ± 8.7 | 2.3 | 72.7 | Acceptance-based behavioral | Eating disorder-general | - | NS* |
| Emotional eating-anger | - | 0.63 | ||||||||
| Emotional eating-anxiety | - | 0.30 | ||||||||
| Emotional eating-depression | - | 0.18 | ||||||||
| Food cravings | Medium | 0.04 | ||||||||
| Grazing behavior | - | 0.41 | ||||||||
| Disinhibition eating | Medium | 0.07 | ||||||||
| Restraint eating | Medium | 0.05 | ||||||||
| Acceptance of the internal experiences associated with food | Large | 0.01 | ||||||||
| Weight loss | 0.01 | |||||||||
| Bradley et al., 2017 | USA | Pre-post | 11 (female 72.7%) | 50.7 ± 13.7 | 3 | 70 | Acceptance-based behavioral | Emotional eating-general | - | 0.09 |
| Emotional eating-anger | - | 0.25 | ||||||||
| Emotional eating-depression | - | 0.08 | ||||||||
| Emotional eating-anxiety | Medium | 0.02 | ||||||||
| Food cravings | - | 0.13 | ||||||||
| Disinhibition eating | Medium | 0.02 | ||||||||
| Restraint eating | Large | 0.01 | ||||||||
| Acceptance of the internal experiences associated with food | Large | <0.01 | ||||||||
| Physical activity | 0.05 | |||||||||
| Weight loss | 0.01 | |||||||||
| Himes et al., 2015 | USA | Pre-post | 28 (female 93%) | 53 ± 9 | 1.4 (6 weeks) | 67.9 | CBT and DBT | Binge eating | Medium | 0.03 |
| Grazing behavior-snacks per day | Medium | 0.01 | ||||||||
| Grazing behavior-eating episodes per day | Medium | 0.01 | ||||||||
| Depression symptoms | 0.01 | |||||||||
| Weight loss | <0.01 | |||||||||
| Sockalingam et al., 2017 | Canada | Pre-post | 19 (female 86%) | 46.2 ± 9.0 | 1.6 (7 weeks) | 73.7 | Telephone-based CBT | Binge eating | Large | <0.001 |
| Emotional eating-general | Large | 0.02 | ||||||||
| Emotional eating-anxiety | Large | 0.04 | ||||||||
| Emotional eating-depression | - | 0.08 | ||||||||
| Emotional eating-anger | Large | 0.01 | ||||||||
| Anxiety | <0.01 | |||||||||
| Depression | 0.01 | |||||||||
| Weight loss | 0.28 | |||||||||
| Intervention before surgery | ||||||||||
| Ashton et al., 2009 | Norway | Pre-post | 243 (female 82.3%) | 47 ± 11.6 | 1 | 100 | CBT | Binge eating | N/A | <0.001 |
| Group differences | ||||||||||
| (p) | ||||||||||
| Hjelmesaeth et al., 2019 | Norway | RCT | 61 (female 70%) | 42.4 ± 10.1 | 48 | 66 | CBT | Emotional eating | - | 0.22 |
| Uncontrolled eating | - | 0.47 | ||||||||
| Cognitive restraint | - | 0.19 | ||||||||
| Anxiety | 0.16 | |||||||||
| Depression | 0.02 | |||||||||
| Weight loss | 0.76 | |||||||||
| Cassin et al., 2016 | Canada | RCT | 47 (female 83%) | 45.5 ± 8.9 | 1.6 (7 weeks) | 74.5 | Telephone-based CBT | Binge eating | Large | <0.01 |
| Emotional eating-anger | Large | <0.001 | ||||||||
| Emotional eating-anxiety | Large | <0.01 | ||||||||
| Emotional eating-depression | Large | <0.001 | ||||||||
| Psychosocial functioning | <0.001 | |||||||||
| Anxiety | <0.001 | |||||||||
| Gade et al., 2014, 2015 | Norway | RCT | 80 (female 68.8%) | 40 ± 10 | 12 | 100 | CBT | Emotional eating | - | NS* |
| Uncontrolled eating | - | NS* | ||||||||
| Cognitive restraint of eating | - | NS* | ||||||||
| Anxiety and depression | NS* | |||||||||
| Weight loss | 0.81 | |||||||||
RCT = randomized control trial; SD = standard deviation; CBT = cognitive-behavioral therapy; DBT = dialectical behavior therapy; BMI = body mass index; PAL = physical activity level; NS* = authors did not report p number, but they reported that p was no significant.; N/A = Not available; - = Not included since it is not significant.
Quality of evidence was rated based on the Grading of Recommendations Assessment, Development and Evaluation system, that classifies the evidence as high, moderate, low or very low quality(38). Evidence was divided into primary outcomes (MEB) and secondary outcomes (weight loss, anxiety and depression symptoms). Quality of the evidence was rated based on the study design, risk of bias, inconsistency and imprecision of results.
Results
Literature search
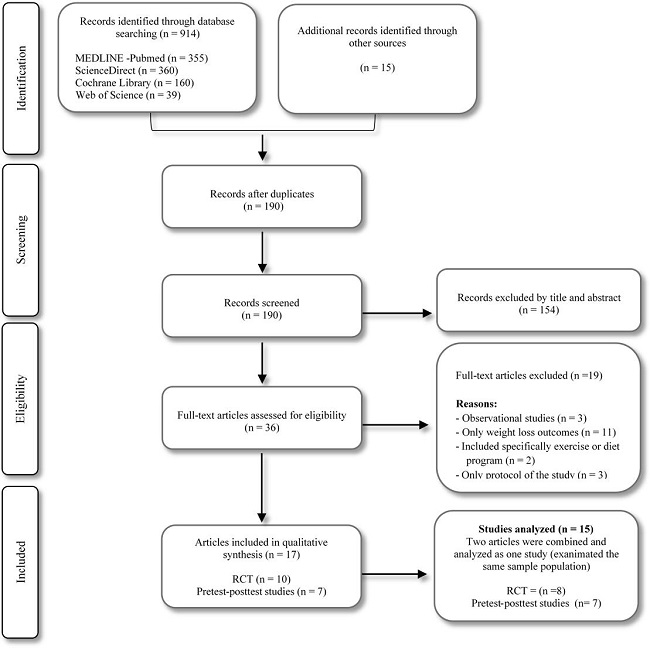
The preliminary search throughout the databases and manual search provided a total of 929 citations. The selection process of the studies is illustrated in a flow diagram (Figure 1).
Study and participant's characteristics
A total of 15 studies were analyzed in this systematic review. Seventeen articles were included, of which two of these assessed the same sample population in different follow-up periods. These articles were combined and analyzed as one study. We included eight randomized controlled trials(39-48) and seven pretest-posttest studies(31,49-54). Retention rate among the studies ranged from 63% to 100%. A total of 752 participants were identified from all the studies and sample size ranged from 7 to 243 participants. Gender distribution was primarily female (80.3%) and the average participant's age was 46.1 years (SD ± 6.6). Follow-up period after intervention ranged from 6 weeks to 48 months. Data collected from each study is summarized in Table 1.
Psychological treatment approaches
Of the four studies that assessed the efficacy of preoperative interventions, three were RCT(39,42-44) and one was pretest-posttest study(49). Of the eleven studies that assessed postoperative interventions, five were RCT(40,41,45-48) and six were pretest-posttest studies (31,50-54). The psychological interventions performed among the studies included were as follows: cognitive-behavioral therapy (CBT), acceptance-based and acceptance and commitment therapy, mindfulness-based therapy, psychoeducational group, and adapted motivational interviewing.
Eight studies included principles of CBT(31,39,42-45,49,50,53), and two of these were performed through phone calls(39,53). Two studies included an acceptance-based behavioral therapy(51,52), and one study an acceptance and commitment therapy(46). Mindfulness-based therapy was performed in two studies(40,56). One study performed a videoconferencing-based psychoeducational group(47,48), and another study performed adapted motivational interviewing(41).
Primary outcome: Maladaptive eating behaviors
All studies reported the examination questionnaires used or applied to measure MEB in their participants. MEB evaluated among the studies included: eating disorders symptoms (general, restraint, related to shape, weight and eating concerns), emotional eating (related to anger, anxiety and depression), binge eating, emotional overeating or uncontrolled eating, disinhibition eating, food cravings, grazing behaviors, and eating self-efficacy. Other behaviors or issues related with MEB were evaluated, such as self-perceived body dissatisfaction, acceptance of weight, confidence of change, and acceptance of the internal experiences associated with food. The most frequent MEB recorded among the studies was emotional eating (11 out of 15) followed by binge eating (8 out of 15).
Overall, all the studies reported an improvement of MEB. However, some of the studies did not report a significant effect compared with the control group (RCT) or after the intervention (pretest-posttest studies). Five out of eight RCT (1 preoperative intervention; 4 postoperative intervention) reported a significant effect (P <0.05) and four had a medium to large effect size between the groups receiving psychological intervention and the control group. Six out of seven pretest-posttest studies (5 postoperative intervention; 1 preoperative intervention) reported significant difference (P <0.05) and had a small to large effect size after receiving psychological intervention.
The study conducted by Hjelmesaeth et al.(44), reported a significant improvement after psychological intervention compared with the control group of emotional eating (P= 0.031), uncontrolled eating (P <0.001), and cognitive restraint (P <0.001). However, these results were reported after a follow-up of 4 months and after psychological intervention (4 weeks before surgery) and these effects disappeared after a follow-up of 1 year and 4 years after surgery.
Secondary outcomes: weight loss, anxiety and depression symptoms
Ten out of 15 studies (four RCT and five pretest-posttest studies) assessed weight loss. Only one (postoperative intervention) of the four RCT reported significant (P <0.05) weight loss after psychological intervention compared with the control group. Three (two postoperative intervention and one preoperative intervention) out of five pretest-posttest studies reported significant weight loss difference (P <0.05) after receiving psychological intervention.
Four pretest-posttest studies (postoperative intervention), and three RCT (preoperative intervention) assessed anxiety and depression symptoms. Four studies (three pretest-posttest studies and one RCT) reported significant improvement in depression symptoms, and two studies (one pretest-posttest studies and one RCT) reported significant improvement in anxiety symptoms.
Quality of the evidence
Based on the GRADE system, the quality of the evidence of the primary outcomes rated from low to moderate. Seven out of 15 studies included were not randomized controlled trials, and 66% of the studies presented a follow-up period of less than six months. Four out of seven RCT had a medium to large effect size. Only four studies assessed MEB for participant's recruitment.
Discussion
To our knowledge, this is the first systematic review aimed to assess psychological intervention approaches for MEB in bariatric surgery patients. The main finding of this study is that psychological interventions (regardless of type of therapy performed) have a positive effect on MEB in bariatric surgery patients at short-term periods. However, the quality of the evidence rated from low to moderate and the effect was not sustained after 12 months of follow-up.
Better results were observed in the studies with a shorter follow-up period. Four studies presented a follow-up period greater than 12 months and only one showed significant improvement on MEB. Therefore, the medium and long-term effect of psychological treatment remain uncertain. The study with the longest follow-up (four years) reported no clinical effects on MEB at the end of the follow-up period(44). The immediate effect showed after 10-weeks of psychological treatment disappeared at the first and fourth year of follow-up. On the other hand, another study with a follow-up of three years(45), reported significant effects on MEB after the end of the follow-up. However, this study conducted several sessions during the three years of follow-up, which suggests that a continuous intervention might result in a sustained positive effect on MEB.
Two systematic reviews and meta-analysis have been published, which evaluated the effect of psychotherapeutic interventions and support groups on weight loss in bariatric surgery patients(32,33), but they do not include specific assessment of MEB. These studies showed that those patients attending psychotherapy or support groups, combined with the surgical treatment, appear to experience greater weight loss than patients treated with bariatric surgery alone.
The major strengths of this study are that more than half of the studies were RCTs (eight out of 15), and almost all of the studies (12 out of 15) presented a relatively high retention rate (>70 %).
Limitations for this review are the lack of high-quality studies, the lack of statistical power of the studies included, the combination of studies with short and medium-term followups, and the inclusion of a wide variety of psychological treatments. Additionally, the inconsistency of the results between the studies with similar follow-up periods might be associated with differences on the assessment of MEB. Another limitation is that only four studies performed a basal or initial evaluation of the recruitment of the participants' sample(31,47,49,50).
The improvement of MEB among bariatric surgery subjects receiving psychological treatment is small. Metabolic and bariatric surgery might have a beneficial impact on eating behaviors; however, this effect does not remain at 12 or more months(42,55). One study with a follow up of three years shows a positive effect of psychological treatment when these continue over time, which suggest that long term interventions are warranted and should be assessed(45).
Conclusion and recommendations
In the present systematic review positive effects on MEB were shown after psychological treatment at short-term follow-up. However, the quality of the evidence rated from low to moderate, and outcomes at ≥12 months of follow-up showed no effect on MEB. Continuous and close monitoring, identification of MEB before and after surgery, and recurrent supportive preand postoperative interventions including psychotherapy are important to maximize surgical outcomes. Further high-quality studies are warranted to assess the effect of psychological treatment for MEB at long-term.