INTRODUCTION
Streptococcus agalactiae .S. agalactiae), also called group B ß-hemolytic streptococcus, is a facultative anaerobic, gram-positive, oxidase, and catalase-negative cocco that forms chains of variable length. Ten serotypes based on specific capsular antigens have currently been identified [1, 2, 3].
In 1887 Edmond Nocard identified it in bovine mastitis and it was related to the decrease in the quantity and quality of milk. This is the reason why it was called agalactiae, which means "without milk." In 1938 Fry described three cases of puerperal infection by S. agalactiae, and several years later it was recognized as the causal agent in neonatal infections. Since then, it has been an agent involved in septicemia and meningitis in newborns, as well as in adverse obstetric outcomes: premature delivery, chorioamnionitis, and fetal death [1, 3, 4].
At the time it has been established that S. agalactiae is part of the normal intestinal flora of humans and other lower species. Without causing infection, it can asymptomatically colonize the male and female urogenital tracts [3]. Colonization frequencies between 4 and 40% have been indicated, depending on age, sexual practices, hygienic conditions and detection methods used, and may be transient, persistent or intermittent. Up to 30% of healthy and colonized adults can present mild or severe infectious symptoms [1, 2]. There is no precision if S. agalactiae should be considered a sexually transmitted germ. The aim is to present the clinical case of a male who consulted for presenting two genital ulcers, in which S. agalactiae was isolated.
CASE REPORT
A 55-year-old black male patient residing in a city located at sea level, with an average ambient temperature of 35ºC and relative humidity of 64%. He carried out professional activity in hot environments, with many hours a day under exposure to sunlight.
He consulted together with his spouse, when he was completing two weeks with itching and burning in the penis. He had noted redness on the glans and scant discharge staining clothing. Miconazole was applied without improvement. He denied anal sex or homosexual activity, urinary symptoms, urethral discharge. He claimed frequent relationships with different partners. In the last month, he had two intercourses with different women, without protection for sexually transmitted diseases. He had lived together with his spouse for twelve years, frequent sexual and traumatic activity for both, due to poor adherence to genital lubricants, prescribed for severe vaginal dryness. His 43-year-old spouse, diagnosed with early ovarian failure due to endometriosis, had undergone subtotal hysterectomy with bilateral oophorectomy.
The patient was found in the glans, an erythematous area of one centimeter, rounded, poorly defined edges and a clean bottom without bleeding. In addition, in the balanopreputial sulcus, another larger lesion, erythematous, raised and pale edges, a bottom with bleeding points and little yellow-green discharge, from which a sample was taken for cytology and microbiology (Figure 1).

Figure 1. Balanopreputial sulcus showing erythema, raised and pale edges, bleeding points and little yellow green discharge.
His partner was asymptomatic. No lymphadenopathy or anal or genital ulcerations. She had perineal fissures and vaginal atrophy: paleness, stiffness, petechiae, and dry walls. Normal cervix. The vaginal cavity was irrigated with sterile physiological saline and one centimeter was taken to perform smears, cultures and antibiograms.
Donovan bodies were not found in the secretion of the ulcers, Gram positive cocci and abundant polymorphonuclear cells were identified. In the culture, S. agalactiae was found, sensitive to daptomycin, levofloxacin, linezolid and vancomycin. In the study of the partner: absence of Donovan and Lactobacillus bodies, with few polymorphonuclear cells. Negative culture. In both partners: negative serologies for chlamydia, HIV and syphilis. There was no clinical information or the possibility of evaluating other sexual contacts. Male's treatment with levofloxacin 750 mg / day for 10 days. One month later, both were asymptomatic and without genital lesions.
DISCUSSION
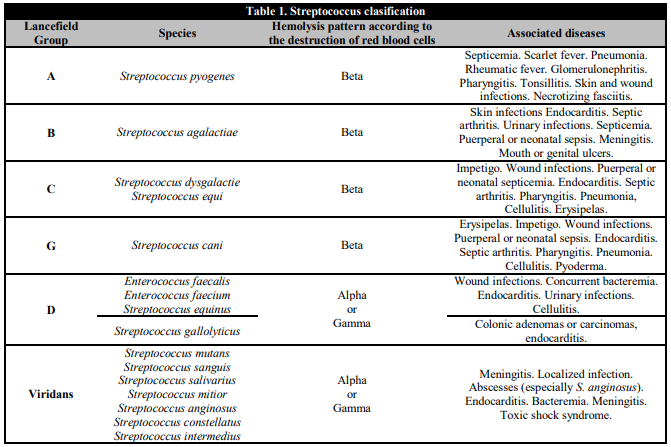
Streptococci are a diverse and heterogeneous group of bacteria. Some can cause disease in humans or animals, but many others are not pathogenic. 49 species and 8 subspecies have been identified, of which more than 30 have been linked to infections in humans. They are classified according to several systems: Lancefield groups, hemolysis patterns and more recently according to molecular or biochemical tests [1]. Table 1 presents a version of Rebeca Lancefield's classification.
An increase in the incidence of S. agalactiae disease in adults has been reported in the United States, from 3.6 x 100,000 in 1990 to 7.3 x 100,000 in 2007 [1], Including from skin or soft tissue infection to bacteremia. In the former, cellulitis, abscesses, ulcers, necrotizing fasciitis or pyomyositis occur. The latter can lead to heart valve lesions, endocarditis, pneumonia, osteomyelitis, and meningitis [1, 2].
S. agalactiae has been found in ulcers in the oral cavity or on the genitals [5, 6]. It has also been found in urethral discharge and is estimated to be present in 1.5% of non-gonococcal urethritis cases [6]. It is usually isolated in 2.0% and 3.4% of urine cultures of men and women, respectively [7]. Urinary infection due to S. agalactiae is associated with chronic prostatitis, vulvovaginitis, and cervicitis. In pregnant women, it is a risk factor for neonatal infection [1]. Generally, vaginal colonization with S. agalactiae is asymptomatic; however there is a greater presence of these bacteria in women with excessive or purulent vaginal discharge [1, 8].
Information on genital ulcers and S. agalactiae is scarce, being limited to few clinical cases. James [9] in 1984 described a very wet and moderately painful bright red circumferential ulceration on the penis of a twenty-year-old. Studies with tests and culture broths used in those times indicated group B ß-hemolytic streptococcus. The patient admitted trauma but did not specify its nature. The authors noted that the ulceration could have been caused by S. agalactiae, although secondary infection at the trauma site was also likely, by agents that asymptomatically colonized the vagina of the sexual partner. The case presented may be a similar situation. The severe vaginal atrophy of the partner and the absence in the regular use of genital lubricant, could favor recurrent genital trauma and the occurrence of lesions on the penis, which secondarily become infected by S. agalactiae that has colonized without symptoms, the vagina of any of the sexual partners. In this regard, Lucks [10] raised the possibility of acquiring S. agalactiae, through a traumatic abrasion during sexual intercourse, with subsequent balanitis.
On the other hand, Frey et al. [5] reported S. agalactiae in painful ulcers on the penis and in the oral cavity of an adolescent, five days after vaginal intercourse and oral sex, with an unknown partner and without the use of a condom. Because S. agalactiae is isolated from the rectum, perineum, vaginal discharge, cervix, and urethra from sexually active people with multiple partners, transmission through sexual contact has been suggested [1]. However, the information available is insufficient to ensure that genital ulcers, caused by or with the presence of S. agalactiae, should be considered a sexually transmitted disease. There is no information on the need for treatment of the sexual partner. In the case presented, no similar lesions were observed, nor were the germ found in the partner. It was limiting not to have been able to obtain information about the other sexual contacts.
Armistead et al. [3] point out that S. agalactiae has the ability to have dual biological behavior: one, as an asymptomatic colonizer and the other, as a powerful pathogen. Most people colonized with S. agalactiae will not experience invasive disease, but entry of the germ into niches outside the gastrointestinal tract or vaginal mucosa can result in infectious events. Although they were not evaluated in the case presented, the virulence of the germ, the immune fragility of the individual, diabetes, liver disease, cancer, neurological disorders and heart or kidney failure, can create conditions that facilitate the transition of S. agalactiae from asymptomatic colonizer to invasive pathogen [1, 2, 3, 5].
There are still knowledge gaps in the understanding of the dual behavior of S. agalactiae. However, the following are involved: host response, signal transduction systems and bacterial adhesins, especially: fibrinogen-binding proteins, hypervirulent adhesin, C5a peptidase, plasminogen-binding surface protein, fibronectin and immunogenic bacterial adhesin, among others [3].
There is no specific antibiotic for genital S. agalactiae infection. Penicillin, ampicillin, cephalosporin, carbapenics, macrolides, and quinolones have been used with good results [5, 6, 7]. Our conclusion: In a promiscuous, heterosexual adult with genital ulcers, S. agalactiae was found. A traumatic event with secondary infection could be the mechanism involved.
AUTHORS' CONTRIBUTION
AM-C performed the clinical evaluation of the couple, performed the diagnosis, treatment and clinical follow-up. The three authors equally (AM-C, AR-B and AM-B) participated in the bibliographic search, document structuring, writing , correction, review of drafts and approval of the final document.
ACKNOWLEDGEMENTS
To Marta Barbosa Basto, graphic designer and member of the Women's Health Research Group, who was in charge of the photographic material. To the University of Cartagena, which, through the Plan for the Support and Strengthening of Categorized Groups of Minciencias, Colombia, supports research training activities for the members of the Women's Health Research Group. Resolution: 01430-2019. Minutes 064-2019.