INTRODUCTION
Low back pain is an important public health problem that often affects the adult population in industrialized society. Its incidence is only surpassed by headaches on the scale of painful disorders affecting people, being a frequent cause [1, 2, 3].
The etiology of low back pain is difficult to identify because it manifests itself under various conditions. Studies show that the main individual and psychosocial risk factors for low back pain are sex, age, body mass index (BMI), genetics, stress, anxiety, and depression [4].
Some symptoms such as anxiety, depression, and kinesiophobia can be considered a tool that predicts the patient's psychological profile, thus contributing to the prognosis and treatment, providing a better therapeutic approach [5, 6].
In a systematic review to seek the best method of physical intervention and rehabilitation for low back pain, comparing several physical therapy interventions, the authors concluded that therapeutic exercises promote a reduction in the intensity of pain and disability for a long period [7].
Considering the high prevalence of low back pain, several treatment techniques have been applied to minimize the damage from these dysfunctions, among which is neural mobilization.
Neural mobilization (NM) is a manual therapy technique that aims to restore the movement and elasticity of the nervous system, generating a consequent better functioning of the musculoskeletal regions. Its execution takes place through oscillating or sustained movements, always in the direction of the peripheral nerves that present limitation in sliding. As a result, signs of neural tension appeared during region-specific neural tests [8].
NM has an influence on the axonal transport process and a consequent increase in the flexibility of rigid nerves and adjacent joint structures. Thus, it leads to greater muscle stregth, increased flexibility of the entire nerve, decreased mechanosensitivity of the nervous system, which is turn increases the confomirty of nervous tissues [9].
The purpose of this review is to assess the consensus of the available evidence about the benefits of neural mobilization in the treatment of patients with chronic low back pain.
MATERIAL AND METHODS
This study is a systematic review of the literature, characterized as an exploratory research. This type of research allows greater flexibility in planning, which makes it possible to make more diverse considerations of the research theme [10, 11].
Regarding the type of intervention, all studies should include NM as an intervention, which may or may not be associated with other physiotherapeutic interventions, provided that the main objective of the study was NM as a form of treatment. The participants had chronic low back pain and were treated with the NM technique, selected according to the criteria of each author of the included articles (individuals diagnosed with chronic low back pain, not submitted to lumbar spine surgery, without systemic pathologies, cognitive alterations, and absolute contraindications for the proposed technique).
Data collection articles and case studies, published in Portuguese, Spanish, and English, with a score equal to or greater than 5 on the PEDro scale, which included neural NM as a form of physical therapy intervention for chronic low back pain were included. Works excluded from books, abstracts, and congress proceedings were excluded; dissertations, pilot studies, course conclusion papers (TCC), and literature reviews.
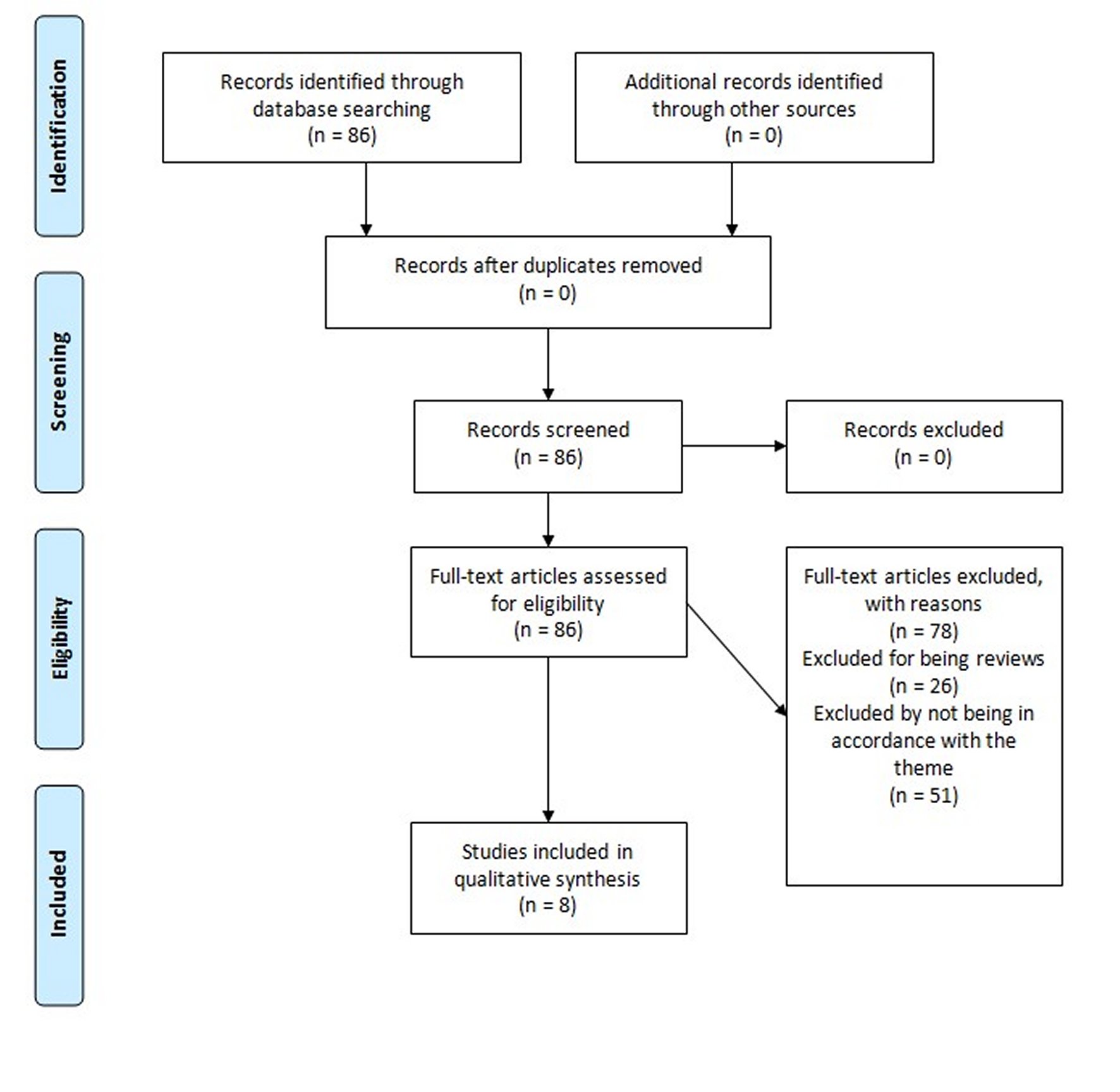
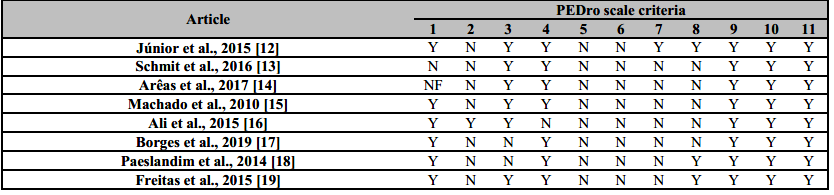
All included articles (Figure 1) were evaluated using the PEDro scale (Physiotherapy Evidence Database), described in Table 1. After analyzing the results obtained through the selected articles, all the data collected, as well as their respective results, were described in Table 2.
The search strategy was carried out in the Google Scholar, Scielo (Scientific Electronic Library Online), Medline (Medical Literature Analysis and Retrieval System Online) / PubMed databases. Searches were carried out in the last 10 years (2010-2020), considering the Portuguese, English and Spanish languages. The keywords and their translations were used: “low back pain”, “chronic low back pain”, “neural mobilization” and “physical therapy intervention”, combined in the most diverse possibilities.
Initially, the articles were analyzed through the title and the abstract and, later, in a judicious manner, the articles were evaluated through critical reading, with the objective of electing those that fit the required criteria. Therefore, the articles included in the systematic review were selected, verifying the positive and negative aspects of each treatment.
RESULTS
The nine articles included in this qualitative synthesis were evaluated based on the PEDro scale to verify their statistical suitability and methodological relevance. Studies that achieved a score greater than or equal to five on this scale were considered adequate, as described in Table 1.
According to the PEDro scale, 4 of the articles included received a score of 5, 3 received a score of 6, 1 received a score of 7 and another received a score of 8, demonstrating an elevated methodological quality of the articles included.
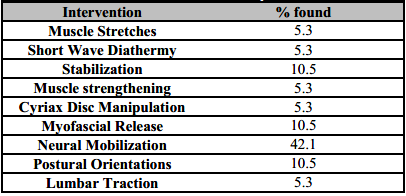
The number of participants involved in all studies totals 123 people. The data show us that the majority of participants were female (62.6%) and relatively young (average age 38.8 ± 8.4 years). Table 2 shows the main interventions carried out in the studies.
In several studies, NM has been associated with some other type of intervention, such as myofascial maneuvers, Cyriax disc manipulation, muscle strengthening, lumbar traction, short wave diathermy, stretching, and postural orientations. In these cases, the results were more expressive concerning the benefit for patients.
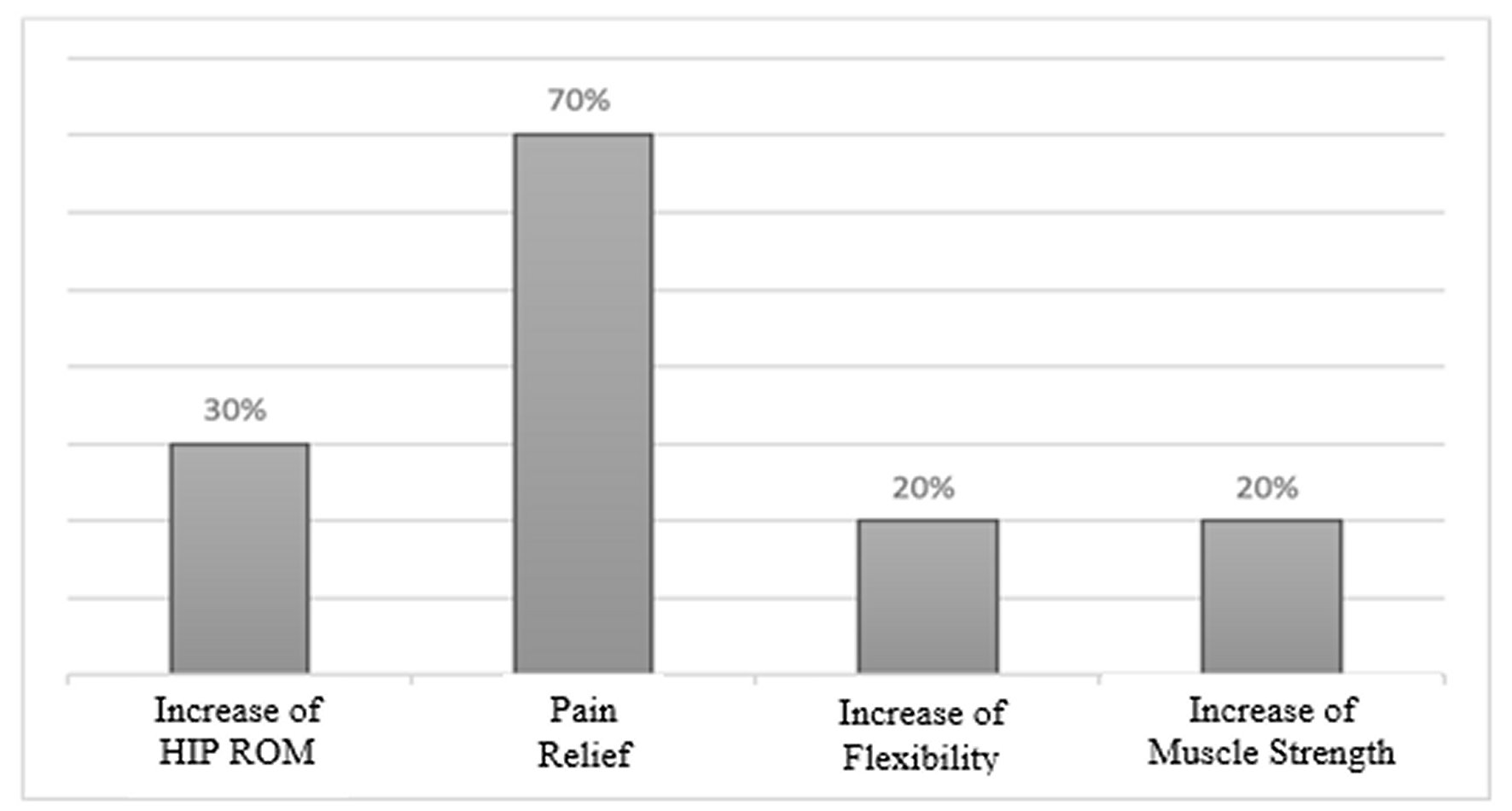
Figure 2 shows the main results observed with the neural mobilization technique in patients with chronic low back pain, pointing out the decrease in pain as being the most relevant (70% of the studies).
Given the analyzed articles, it is possible to observe that in most interventions aimed at chronic low back pain where NM was used, there were significant results. In all cases, this type of treatment reduced the intensity of pain, in addition to improving the flexibility of neural tissue. Pereira Junior et al., 2015, used only the NM technique as a form of treatment for patients with chronic low back pain. Both showed that the NM increased the range of motion of trunk flexion, which was confirmed by the goniometry tests and the Wells bench. Regarding pain, Pereira Junior et al., 2015, concluded that NM had limited effects [12]. Arêas et al., 2017, also evaluated the effects of NM in isolation and concluded that the mobilization promoted an increase in knee flexor muscle strength, increased flexibility in knee flexion and extension movements. However, they did not evaluate the effects of the technique on pain pictures [16].
Of the articles included in this review, six brought NM associated with other physical therapy techniques, such as strengthening, stabilization, stretching, and pompage, among other techniques used in clinical practice in the treatment of chronic low back pain. Ali et al., 2015, and Borges et al., 2019, associated mobilization with segmental stabilization and concluded that these techniques performed in the association were effective in controlling pain and improving functional capacity, but did not know whether these techniques performed in isolation would have the same results [15, 17].
The stretching technique associated with NM has shown satisfactory results, with increased flexibility of the posterior chain and reduced pain, but it is also unknown whether these techniques performed in isolation would bring the same benefits [15].
Paeslandim et al., 2014, and Schimit et al., 2016, associated NM with more than one physiotherapeutic technique and were able to assess the level of pain and degree of muscle strength. Regarding the pain, both showed a reduction in pain levels but presented different results about the increase in the strength pattern [13, 18].
The decrease in pain, which was the main objective of the interventions in the selected articles, was reported in 70% of the studies. This percentage is in line with the results obtained in the studies by Kurt, Aras, and Buker, 2020, and Neto et al., 2017 [19, 20]. The Visual Analog Pain Scale (EVAD) was the most used assessment, characterized by a validated method that quantitatively appreciates the presence and intensity of the individual's pain. Recently, Ramos et al., 2020, demonstrated that individuals treated with NM had an average 70% reduction in pain after the treatment, which was assessed by EVAD, in addition to increasing lumbar mobility. This shows that NM relieves pain and accelerates the functional recovery process, in addition to optimizing the return of participants to activities of daily living [21].
Regarding the frequency of intervention, the authors used it 2 to 3 times a week, for a period of 4 to 8 weeks. In 2012, Monerrat et al., demonstrated that the use of 4 weeks of treatment in different disorders with variations in the number of sessions was sufficient to obtain satisfactory results. In contrast, Machado and Bigolin, 2010, used 20 sessions, held twice a week, and obtained results that are even more significant when it was compared to other studies [22].
The age range of the samples from the studies included in the present review ranged between 30 and 70 years. Regarding gender, the majority were female. This fact is supported by what is already being shown in some studies, which show that the overload of occupational and domestic tasks and the accumulation of roles making women more likely to develop musculoskeletal pathologies, such as low back pain [23].
In addition, it is worth mentioning that a biopsychosocial perspective of chronic pain suggests the existence of a dynamic relationship between biological changes, psychological status, and social context, emphasizing that these factors have different roles in chronic pain, disability, and emotional maladjustment, which makes individuals even more susceptible to chronification[24].
Although the articles included in this review have shown satisfactory results of NM as a treatment for chronic low back pain, either in isolation or in association with other techniques, these studies had limitations in the composition of their samples, as they are small and quite heterogeneous samples. Therefore, it is essential to reinforce that the objective of the sample calculation is to determine the elements that are necessary to compose the sample, obtaining valid results. Besides, the methodology must be carried out properly so that the sample results can be generalized to the population. It is necessary to ensure that the sample is representative, that is, it must present general characteristics of the population.
Regarding the number of articles, the quantity on the topic is still quite limited in the scientific literature, making it necessary to conduct further research to prove its effectiveness, as in randomized clinical trials. Thus, the importance of further studies to perceive NM as a form of treatment for chronic low back pain is perceived, since this technique has shown satisfactory results, in addition to presenting low cost, being easy to apply, and without side effects.
CONCLUSIONS
Considering the quality of the articles and their results presented, it is concluded that neural mobilization is an effective technique in reducing pain intensity and stiffness, in addition to increasing ROM, improving tissue extensibility in the treatment of patients with chronic low back pain.