My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 n.1 Madrid Jan. 2010
LETTERS TO THE EDITOR
Lymphoepithelial cyst of the pancreas mimicking a cystic neoplasm
Quiste linfoepitelial de páncreas. Un simulador de neoplasia quística
Key words: Lymphoepithelial cyst. Pancreatic true cyst. Benign pancreatic cyst.
Palabras clave: Quiste linfoepitelial. Quiste pancreático verdadero. Quiste pancreático benigno.
Dear Editor,
Cystic lesions of the pancreas are rare. They can be classified into pseudopancreatic cysts (80%) and true pancreatic cysts (20%). Lymphoepithelial cysts of the pancreas (LECP) are true pancreatic cysts, benign and extremely rare that can mimic cystic neoplasms making difficult its differential diagnosis preoperatively.
Case report
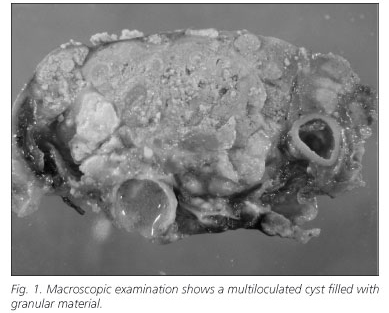
A 73-year-old male patient was found to have a pancreatic cystic lesion after undergoing an abdominal computed tomography (CT). Physical examination and blood tests were normal except for elevated CA 19-9 and CEA levels. Abdominal CT and magnetic resonance imaging (MRI) showed a multiloculated lesion of 5.2 cm in diameter in the body tail of the pancreas. Both CT and MRI features of the mass favored a mucinous cystic neoplasm so we made the decision to operate the patient. A distal splenopancreatectomy involving the cystic lesion was carried out with a rim of normal pancreatic tissue. Pa-thologic examination (Fig. 1) revealed: yellowish multiloculated cyst, well circumscribed, filled with abundant amorphous and granular material. Microscopically presented a wall lined by stratified keratinized squamous epithelium surrounded by lymphoid tissue with germinal centers. The cyst was filled with anucleated squamous cells, proteinaceus material and cholesterol crystals. These findings were diagnostic of a benign LEC of the pancreas.
Discussion
Lymphoepithelial cysts of the pancreas were first described in 1985. About one hundred cases have been previously described (1). This is the first reported case in Spain. LECPs occur more commonly in the middle-age man, often asymptomatic, and may appear either intrapancreatic or peripancreatic.
The etiopathogenesis as well as histogenesis of LECPs remain unclear. They have been described in other locations in which frequently are associated with autoimmune diseases and states of immunological depression (2).
Diagnosis of LECPs preoperatively is difficult because they can mimic other cystic pancreatic lesions. Differential diagnosis of LECPs may include pseudocyst, mucinous cystic neoplasm and intraductal papillary mucinous neoplasm.
Chemical analysis of pancreatic LECPs fluid have shown a high level of tumor markers CEA and CA 19-9 as well as variable levels of amylase (3).
Abdominal US can see LECPs as solid masses to cystic lesions. The CT scan usually shows features of a low-attenuation mass or multilocular lesions (60%) with a thin enhancing rim. Magnetic resonance imaging (MRI) on the basis of the lipid cystic component perceives a lesion with a high signal in T1 and a low signal in T2.
Nowadays, the fine-needle aspiration cytology (FNA) has become the definitive diagnostic method. Cyst aspirates reveal yellowish creamy features. Cytologically, the aspiration material from a LECP typically contains abundant proteinaceus material, anucleated squamous cells, cholesterol crystals, squamous cells without nuclear atypia and polymorphous lymphoid population. Unfortunately often cytological findings are unclear, leading to misdiagnosis or uncertain diagnosis.
Histologically, the differential diagnosis should include all cystic lesions that may be found in the pancreas, essentially the dermoid cyst. It has epidermal appendages and absence of lymphoid tissue typical of LECP.
In the present case preoperative EUS-FNA was not performed for the high radiological malignancy suspicion and due to the delay in the definitive surgical treatment that would have involved the absence of this diagnostic procedure in our hospital.
Several treatment options are suggested in the literature. Some authors recommend surgical excision (distal pancreatectomy with or without splenectomy) since these lesions are very rare and can easily mimic cystic neoplasms of the pancreas (4). But recently the tendency is to adopt a conservative management. If the patient is asymptomatic and EUS-FNA firmly establishes the diagnosis of LECP based on cytological examination of the cyst fluid, surgery can be avoided and then patient may be followed with serial cross-sectional imaging of the upper abdomen. To our knowledge, 26 patients with LECPs have been reported diagnosed by CT- or EUS-guided FNA (2,3,5). Of these, 11 patients have been followed and no clinical and radiological changes have been found in the characteristics or size of the lesion. The last eight cases are concentrated in the last year reflecting the increasing use of imaging tests and FNA and better knowledge of this entity. In patients who are symptomatic or when there is a doubt in the cytological diagnosis, minimal resection of the cyst should be performed including enucleation of the cyst with a rim of normal pancreatic tissue (6). After local resection, the prognosis is excellent with no incidence of recurrence to date.
M. J. Alcaide-Quirós1, M. Castellote-Caixal1, F. Feliu-Villaró1, A. Raventós-Estelle2, A. Caro-Tarragó1 and V. Vicente-Guillén1
Departments of 1General Surgery and Digestive Diseases, and 2Pathology. University Hospital Joan XXIII. Tarragona, Spain
References
1. Frezza EE, Wachtel MS. Lymphoepithelial cyst of the pancreas tail. Case report and review of the literature. JOP. J Pancreas (Online) 2008; 9(1): 46-9. [ Links ]
2. Jian B, Kimbrell HZ, Sepulveda A, Yu G. Lymphoepithelial cysts of the pancreas: endosonography-guided fine needle aspiration. Diagn Cytopathol 2008; 36(9): 662-5. [ Links ]
3. Ahlawat SK. Lymphoepithelial Cyst of pancreas. Role of endoscopic ultrasound guided fine needle aspiration. JOP. J Pancreas (Online) 2008; 9(2): 230-4. [ Links ]
4. Bolis GB, Farabi R, Liberati F, Macciò T. Lymphoepithelial cyst of the pancreas. Report of a case diagnosed by fine needle aspiration biopsy. Acta Cytol 1998; 42(2): 384-6. [ Links ]
5. Nasr J, Sanders M, Fasanella K, Khalid A, McGrath K. Lymphoepithelial cysts of the pancreas: an EUS case series. Gastrointest Endosc 2008; 68(1): 170-3. [ Links ]
6. Madura JA, Yum MN, Lehman GA, Sherman S, Schmidt CM. Mucin secreting cystic lesions of the pancreas: treatment by enucleation. Am Surg 2004; 70(2): 106-12. [ Links ]











 text in
text in