Introduction
Caring for a dependent person is highly demanding and often entails a significant reduction in the time the caregiver spends doing activities they enjoy. Between 66.0% and 80.2% of caregivers report having problems related to their free time. Specifically, as a result of their caregiver responsibilities, 61.8% of caregivers have seen their leisure time reduced, between 17.4% and 55.0% spend less time with family and friends, between 38.0% and 49.0% have given up vacations, hobbies, and social activities, and 30.0% have reduced their physical activity (Alzheimer's Association & National Alliance for Caregiving, 2004; Instituto de Mayores y Servicios Sociales, 2005).
The reduction in these activities could be relevant to caregivers’ psychological well-being (Losada et al., 2010). In fact, caregivers have a high prevalence of depression, with 8.9% having experienced an episode of major depression (Torres et al., 2015). In addition, between 30% and 80% exhibit clinically significant symptoms of depression (i.e., subclinical depression; Schoenmakers, Buntinx, & Delepeleire, 2010). Though not a major depressive episode, subclinical depression is not a minor issue, as it causes discomfort and significant functional deterioration (Backenstrass et al., 2006) and increases the probability of developing a major depressive episode (Cuijpers & Smit, 2004).
Moreover, both phenomena-the reduction of pleasurable activities and depression in caregivers-could be related. A low rate of environmental response-contingent positive reinforcement (RCPR), determined by the number of reinforcing events, their availability in the context, and the individual's ability to achieve this reward, is considered a critical predictor of depression (Lewinsohn, 1974), giving rise to the two most important psychopathological phenomena for this disorder: depressed mood and extinction of non-depressive (i.e., healthy) behaviors that have been positively reinforced by the social environment. According to this approach (Hopko, Lejuez, Ruggiero, & Eifert, 2003; Lewinsohn, 1975), the appearance of a depression would require the presence of three conditions: (a) absence of reinforcers in the environment, (b) lack of social skills to obtain the reward, and (c) subject’s inability to perceive or enjoy rewards, even if they exist in the environment, due to the presence of high levels of social anxiety that interfere with the utilization of social skills and achievement of social rewards. Likewise, the activity restriction model (Williamson & Shaffer, 2000) proposes that the restriction of normal or pleasurable activities after a negative life event plays an important role in the appearance of depression, acting as a mediator between the negative life event (e.g., becoming a non-professional caregiver) and depressive symptoms (Mausbach, Patterson, & Grant, 2008).
In fact, previous research on caregivers has found evidence of the relationship between reduced participation in activities and depression in caregivers (Mausbach, Roepke, Depp, Patterson, & Grant, 2009; Mausbach et al., 2011; Nieboer et al., 1998; Romero-Moreno, Losada, Márquez-González, & Mausbach, 2014). Despite this relationship, to date, no study has analyzed environmental RCPR as a predictor of different levels of depression (i.e., no depression, subclinical depression, and major depressive episodes) in the caregiver population. In addition, the previous studies have some limitations. They were focused almost exclusively on caregivers for people with dementia, using the activity restriction model, and assessed the level of reward using lists of pleasurable activities to analyze the frequency of participation in pleasurable events, or else activity restriction scales that evaluate the degree to which they have been restricted by the obligations of care. However, they did not necessarily evaluate the environmental reward at the functional level. In addition, they evaluated depressive symptoms using quantitative scores from self-report scales, thus they cannot elucidate the relationship between the reward and the presence of subclinical depression or a major depressive episode as identified using standardized diagnostic criteria (e.g., the Diagnostic and Statistical Manual (DSM) or the International Classification of Diseases (ICD)). Therefore, the main objective of this study was to analyze RCPR, evaluated at the functional level, as a predictor of depression level (i.e., no depression, subclinical depression, major depressive episode) in non-professional caregivers.
Method
Participants
A cross-sectional study was conducted between January 2014 and December 2015. The sample was extracted using simple random sampling among the 18,410 recognized caregivers in the official registry of the Ministry of Labor and Welfare of the Autonomous Community of Galicia (Spain).
To participate in this study, participants had to: (a) be a family caregiver for a person whose dependence was officially recognized; (b) live with the care-recipient; and (c) provide informed consent. The study excluded those who (a) presented conditions that could interfere with the evaluation (e.g., intellectual disability); (b) took care of a relative with a terminal prognosis of one year or less; or (c) who had received psychological or pharmacological treatment in the last two months.
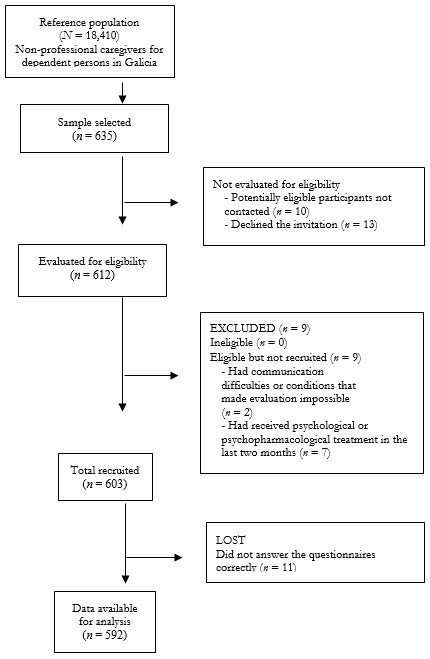
The sample size was estimated on the basis of the prevalence of significant depressive symptomatology (Rodríguez et al., 2002) and major depressive episodes (Torres et al., 2015) in Spain’s caregiver population. Utilizing an alpha risk of .05, for an estimated prevalence of subclinical depression and major depressive episode of ≈ 32%, and an error of 4%, a total of 508 participants were required for the current study. The sample size was increased to 635 caregivers to account for a 20% attrition rate. The response rate was 95.0%: Of the 603 people who met the eligibility criteria and participated, 11 did not properly fill out the self-administered instruments and therefore were eliminated from the analyses. The final sample consisted of 592 caregivers (see Figure 1). No significant differences were identified in caregiver/care-recipient sociodemographic variables and the care situation between those who did and did not complete the evaluation correctly.
Participation was voluntary and no financial or other incentives were provided. All participants provided their informed consent. The study respected the principles of the Declaration of Helsinki and was approved by the Bioethics Committee of the University of Santiago de Compostela.
Measures
Sociodemographic variables of the caregiver, care-recipient, and the care situation. An ad hoc questionnaire designed for this study was used to collect information on the caregiver’s sex, age, marital status, social class, educational level, and relationship with the care-recipient; the care-recipient’s sex, age and diagnosis; and the duration of care and daily hours devoted to care.
Environmental Reward Observation Scale (EROS; Armento & Hopko, 2007; Spanish version by Barraca & Pérez-Álvarez, 2010). This is a 10-item self-reported scale that provides information on the degree of response-contingent environmental positive reinforcements earned by the participant in recent weeks. The items were constructed considering the three criteria established by Lewinsohn (1974) to define this construct. Each item is evaluated on a 4-point Likert scale (1= completely disagree; 4 = completely agree). Items 2, 5, 6, 7, and 9 are reverse scored. Scores range from 10 to 40, with a higher score indicating a greater degree of positive environmental reward. The internal consistency of the Spanish version was .86 and it presents evidence of criterial validity. It is highly correlated with instruments used to evaluate depressive symptomatology, behavioral activation, anxiety, and experiential avoidance.
Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977; Spanish version by Vázquez, Blanco, & López, 2007). This is a 20-item self-reported scale that evaluates the level of depressive symptomatology. The person evaluates each item according to the frequency with which they have experienced the symptom in the last week, using a scale from 0 (rarely or never) to 3 (most of the time). For all items, except for four inverse response items (4, 8, 12, and 16), a higher score indicates greater deterioration. The scale ranges from 0 to 60, with a higher score corresponding to greater depressive symptomatology. A score of 16 or higher is considered indicative of a risk of depression. The internal consistency for the Spanish version was .89.
Structured Clinical Interview for DSM-5 - Clinician Version (SCID-5-CV; First, Williams, Karg, & Spitzer, 2015). This is a semi-structured interview that covers the most common clinical diagnoses according to the DSM-5 and must be administered by a clinician. The interview questions are formulated according to each of the corresponding DSM-5 criteria and must be classified as present or absent. This study used the items related to major depressive episode from Module A - mood episodes and persistent depressive disorder. The SCID's severity scales, including the evaluation of depressive episodes, have a high internal consistency (all Cronbach's α's > .80), test-retest reliability, and concurrent and predictive validity (Shankman et al., 2018).
Procedure
A protocol was developed detailing the objectives of the study, the design and framework, the participants (estimation of sample size, sampling, and eligibility and recruitment criteria), measures (predictors and outcome), biases (no response, recollection, selection), quality control for the procedure, data management and analysis, and ethics. Two independent psychologists were trained to conduct the evaluation using seminars and role-playing with two clinicians with more than 20 years of experience in evaluating and diagnosing mental disorders. A pilot study was conducted with 50 randomly selected caregivers to assess the adequacy of the assessment instruments, the competence of the evaluators, and the feasibility of the study.
The sociodemographic characteristics of the caregiver and care-recipient, the care situation, environmental reward, and depressive symptomatology were evaluated using self-administered instruments near the participants’ homes by evaluators who were masked to the diagnosis of major depressive episode. In addition, two expert clinicians masked to the results of EROS and CES-D established the diagnosis of major depressive episode for each caregiver using the SCID-5-CV. Each evaluation lasted approximately 45 minutes.
The selected caregivers were contacted via letter informing them of the study and asking them to return a sealed postcard if they did not wish to participate. Those who did not return the postcard were contacted, informed of the nature of the investigation. and invited to participate. One of the clinical experts supervised the evaluators each week, providing feedback.
The strategies recommended by Hulley, Cummings, & Newman (2013) were followed to minimize the loss of participants, such as providing reminders of the interview date, eliminating invasive procedures for data collection, and presenting the study in an appealing manner.
Data Analysis
The statistical package SPSS for Windows (version 22.0) was used to analyze the data. The sociodemographic characteristics of the caregiver and care recipient, the care situation, environmental reward, and depression level were analyzed using frequencies, percentages, means, and standard deviations. Caregivers were classified into three groups based on depression level: (a) no depression, consisting of caregivers with a score < 16 on the CES-D who did not meet the diagnostic criteria for a major depressive episode; (b) subclinical depression, consisting of caregivers who obtained a score ≥ 16 on the CES-D and did not meet the criteria for major depressive episode; and (c) major depressive episode, consisting of caregivers who met the diagnostic criteria for major depressive episode.
For clinical and statistical reasons, the caregiver and care-recipient sociodemographic and care situation variables are codified as follows: caregiver sex (male or female), marital status (without partner and partner), social class (lower/lower-middle and middle/upper-middle), educational level (able to read and write, primary school, and secondary/university), caregiver and care-recipient relationship (parent, child, or other) and care-recipient sex (male or female) have been presented in their original response format. Taking the statistical distribution as a reference (below and above the mean), caregiver age was recoded as ≤ 55 and > 55 years, care-recipient age as ≤ 63 and > 63 years, and care duration as ≤ 13 years and > 13 years. For statistical reasons (given that caregivers for persons with major dementia are the majority in this sample) and clinic reasons related to the contradictory results in studies that have evaluated the consequences of caring for people with dementia versus other pathologies in terms of caregiver emotional state (Vázquez, Otero, Blanco, López, & Torres, 2018), the diagnosis of the care-recipient was recoded as dementia and not dementia. Finally, to differentiate among those who performed care tasks during the day from those who provided a greater number of care hours, the variable daily hours devoted to care was dichotomized into ≤ 12 hours and > 12 hours (similar to Torres et al., 2015).
To analyze the differences in reward according to the sociodemographic characteristics of the caregiver, care-recipient, care situation, and depression level, Student t-tests for independent samples and analysis of variance (ANOVA) were used. Post-hoc analyses were performed using the Bonferroni test.
A multinomial logistic regression analysis was performed to analyze the relationship between reward and depression level (with depression level as a dependent variable). The odds ratios (ORs) were analyzed without adjustment and adjusted by caregiver sociodemographics (sex, age, marital status, social class, educational level), care-recipient sociodemographics (kinship, sex, age, and diagnosis) and care situation (care duration and daily hours of care provided).
Results
Characteristics of the sample
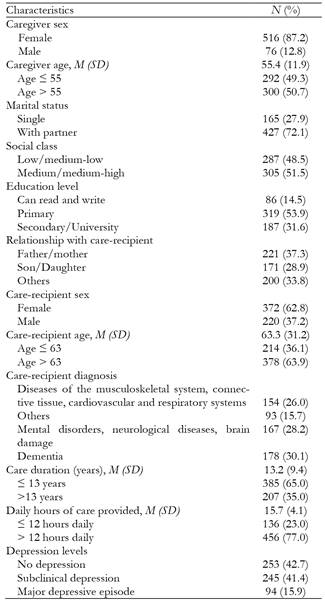
As can be seen in Table 1, 87.2% of the caregivers were women, with an average age of 55.4 years (SD = 11.9), 50.7% were older than 55 years, 72.1% had a partner, 51.5% were middle/upper-middle class, and 53.9% had only a primary school level of education. The caregivers provided care for a parent in 37.3% of cases, and 62.8% of care-recipients were female, with an average age of 63.3 years (SD = 31.2); 63.9% of cases involved a care-recipient older than 63 years. A diagnosis of dementia was present in 30.1% of the cases. Caregivers had provided care for a mean of 13.2 years (SD = 9.4); 65% of cases involved 13 or fewer years of care. Caregivers provided an average of 15.7 hours of care per day (SD = 4.1), with 77.0% of caregivers providing more than 12 hours of care a day. There was no risk of depression present in 42.7% of the caregivers, while 41.4% presented with a risk of depression and 15.9% met the criteria for a major depressive episode.
Differences in reward according to the characteristics of the caregiver, care-recipient, care situation, and depression level
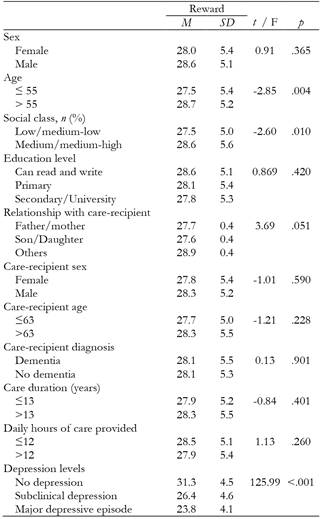
The average score for reward was 28.1 (SD = 5.3). Table 2 shows the means and standard deviations for reward according to the variables of caregiver and care-recipient socio-demographics, care situation, and the three depression levels. We found significantly lower reward scores in caregivers aged 55 years or younger, t (590) = -2.85, p = .004 and those in the lower/lower-middle class, t (588.469) = -2.60, p = .010. Likewise, according to the results of the post-hoc analyses, caregivers without depression exhibited greater reward than those with subclinical depression (p < .001) and those experiencing a major depressive episode (p < .001). Caregivers with subclinical depression exhibited greater reward than those experiencing a major depressive episode (p < .001). No relationship to differences in reward were identified for the other variables.
Relationship between reward and depression level
Table 3 shows the odds ratios (OR) for the association between reward and depression level (no depression, subclinical depression, major depressive episode), unadjusted and adjusted by the characteristics of caregiver and care-recipient sociodemographics and the care situation. Caregivers with higher reward scores had a significantly lower probability of developing subclinical depression (adjusted OR = 0.78, 95% CI 0.75-0.83) or a major depressive episode (adjusted OR = 0.67, 95% CI 0.62-0.72).
Table 3. Reward as a predictor of depression level in the caregiver population.
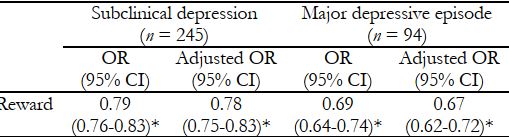
Note: Reference group = No depression (n = 253). OR = Odds Ratio. Adjusted OR = Odds ratio adjusted for variables for caregiver (sex, age, social class, educational level), care-recipient (kinship, sex, age, and diagnosis), and care situation (care duration, daily hours of care provided). 95% CI = Confidence interval at 95%.
* p <.001
Discussion
The aim of this study was to analyze environmental reward as a predictor of depression level (no depression, subclinical depression, and major depressive episode) in non-professional caregivers.
The average reward score obtained by the caregivers (28.1) was slightly lower than that found in the non-clinical Spanish population (Barraca & Pérez-Álvarez, 2010). These results are consistent with previous findings that caregivers reduce their participation in pleasurable activities (Alzheimer's Association & National Alliance for Caregiving, 2004; Instituto de Mayores y Servicios Sociales, 2005) and participate in fewer social activities than non-caregivers matched for age and sex (Clark & Bond, 2000).
Reward was significantly lower in caregivers who were 55 or younger. One possible explanation is that younger caregivers may have less time for pleasurable activities because they have to combine care tasks with other life tasks such as work and caring for minor children. This finding is consistent with Romero-Moreno et al. (2014), where older caregivers had a higher frequency of leisure activities and high satisfaction with these activities. Likewise, reward was lower in caregivers from the lower-middle/lower class compared to those of middle/upper-middle class. A tentative hypothesis from this finding is that caregivers from the lower classes might have fewer resources to handle the demands of care, which limits their ability to get help and therefore reduces their available time. No other variable showed a relationship to differences in reward.
In addition, the average score for reward was significantly higher in caregivers with no depression compared to those who had subclinical depression or a major depressive episode, and in caregivers with subclinical depression compared to those with a major depressive episode. One possible explanation is that caregivers without depression are more active in the search for environmental rewards and have more ability to obtain them than those with subclinical depression, and the latter, in turn, are more capable of doing so than those who experience a major depressive episode-a finding that is consistent with Lewinsohn (1974). Once depressive symptoms begin to be present, the symptomatology itself could make it difficult to seek out and achieve environmental rewards and instead favor avoidant behaviors to guard against potentially aversive stimuli (Trew, 2011), constituting a risk factor for a major depressive episode (Joling et al., 2015).
Finally, caregivers with greater positive environmental reinforcement were less likely to present with subclinical depression or major depressive episodes (even after controlling for sociodemographic and care variables), which suggests that reward acts as a protective factor against both levels of depression and especially against major depression. These results provide support for behavioral models of depression (Lewinsohn, 1974; Williamson & Shaffer, 2000), indicating that caregivers who obtain positive rewards in a low-reinforcement environment (e.g., without leaving home) will be more protected against a major depressive episode.
This study has important implications for research and clinical practice. It suggests that an increase in positive rewards may be an appropriate strategy for mood regulation. Behavioral therapies focused on increasing environmental reward, such as behavioral activation, for caregivers with various levels of depression might be protective against the development of subclinical and major depression. This treatment modality for depression has well-established efficacy in other populations (Cuijpers, van Straten, & Warmerdam, 2007) and is recognized as an evidence-based intervention by the National Institute for Health and Clinical Excellence (NICE; National Collaborating Centre for Mental Health, 2010). It is especially recommended for younger caregivers and those with subclinical depression. In fact, randomized controlled trials aimed at caregivers with subclinical depression have demonstrated prevention of depression using problem-solving and cognitive-behavioral interventions (e.g., Vázquez et al., 2013, 2016). In addition, some studies using behavioral activation (Read, Mazzucchelli, & Kane, 2016; Vázquez et al., 2017; Vázquez et al., 2018) and cognitive-behavioral interventions (Vázquez et al., 2014) have shown promising results. The parsimony of behavioral activation compared to other psychological interventions makes it ideal for training professionals and application to this population with limited time availability.
This study also has limitations. The transversal design does not allow us to establish causal relationships between reward and depression. In addition, only the role of reward has been analyzed; however, its weight is unknown in relation to other potential risk factors for depression in caregivers (e.g., deficits in problem-solving skills or irrational thoughts). Future research should evaluate the contribution of reward versus other potential variables involved in the development and maintenance of depressive pathology of caregivers. Despite these limitations, this is the first study that has analyzed the role of environmental reward as a predictor of depression levels in caregivers using a diagnosis of major depressive episode by expert clinicians in a randomly selected sample of caregivers for persons with a variety of pathologies, which points to a greater generalizability of its results.











 texto em
texto em