INTRODUCTION
Swallowing is a complex process that depends on the integrity of various physical structures and aims to transport food from the oral cavity to the stomach without penetration into the airways (1). Any change that hinders swallowing safety and efficiency is classified as dysphagia, recognized by the World Health Organization within the symptoms related to the digestive system (1 2-3). In the general population, the prevalence of neurogenic oropharyngeal dysphagia (NOD) varies from 2% to 16%, with values above 40% in hospitalized patients (2 3-4). Although it may occur at any age, the highest prevalence of oropharyngeal dysphagia is found in the elderly, where it may be permanent or transient (4). Risk factors include use of medications, tracheostomy, previous orotracheal intubation, head and neck surgery, and neurological disorders such as Parkinson’s disease, Alzheimer’s disease, neurodegenerative diseases, and stroke (5,6). Dysphagia, regardless of etiology, leads to severe consequences such as malnutrition, significant weight loss, aspirative pneumonia, and mortality (6,7).
Speech therapy aims to minimize the complications of OD and includes the definition of a safe feeding path (8), as well as the modification of food characteristics such as texture and consistency (9,10). Liquids are associated with laryngeal penetration (11), and to promote safe and efficient swallowing homogeneous and thick diets are recommended (9). Thickened beverages compensate deficits and reduce aspiration risk (2,3,12 13 14 15-16). However, increased viscosity renders oral and pharyngeal transit longer (2,9), increases the risk for food residues (2,10,15), and demands greater tongue pressure when swallowing (2,10,17). Liquids must be thickened to a specific viscosity to improve swallowing safety for each patient, since very thin liquids can be as detrimental as excessively thickened ones (18) and a correct selection depends on evaluation findings (19).
Currently, it is understood that a standardization of terminology to identify consistencies is relevant to guarantee the efficiency of treatment (3,20 21-22). Internationally, several standardized terminologies are used (23 24 25-26), most commonly the National Dysphagia Diet (NDD) (27) and International Dysphagia Diet Standardization Initiative (IDDSI) (28). The NDD was published in 2002 by the American Dietetic Association in order to establish a standard terminology and the practical applications of dietary texture modification for dysphagia; it includes 4 levels for liquid foods (27). The IDDSI was proposed in 2016 with the aim of developing a globally standardized terminology to describe food consistencies as used for individuals with dysphagia. It includes 8 consistency levels and proposes simple methods of measuring consistency using a syringe, fork and spoon (28).
Lack of standardization in consistency nomenclature generates risks to the patient (3,20,29). The viscosity of thickened liquids is often judged subjectively and described using terms such as syrup and honey (29). Prescriptions involving viscosity and texture should allow efficient communication between professionals (3,20,29).
Speech therapists ought to know and use a standard viscosity nomenclature, otherwise their practice may generate risks to their patients. Accordingly, the present study aims to assess the ability of speech therapists to identify, sort, and name the different consistencies used in NOD management, and to compare the results with the terms proposed by the Dysphagia Diet Standardization Initiative (IDDSI).
METHOD
This was a cross-sectional, descriptive and analytical study. It was approved by the institution’s Ethics Committee (2.490.627). The sample consisted of speech therapists who work with neurogenic oropharyngeal dysphagia (NOD) patients. These professionals were contacted by e-mail, by phone and in person. A total of 114 participants were contacted and invited, and 65 accepted to take part. As inclusion criteria for this study, the participants had to work with NOD patients. Participants who would not fill out the questionnaire or who later stated that they did not exactly work with NOD patients were excluded.
Data were collected at their workplace. The participants were informed of the study’s aims and provided a signed consent to participate. The questionnaire assessed sample characteristics such as age, gender, work with NOD patients or otherwise, timing of professional activity with dysphagia, workplace, and population served.
The sorting and naming tasks were initially explained to each participant, and the 5 foods presented simultaneously in small portions arranged in colored disposable cups, but not in increasing or decreasing order of consistency. The participants were instructed to sort these foods from thinnest to thickest viscosity, and to write in blank spaces the terms they would use to describe the consistencies presented. The materials available to participants were watercolor pens (green, blue, purple, grey, and pink), a 10 mL syringe without needle or plunger, a stopwatch, spoons and forks. Participants were allowed to manipulate the samples if they wanted to. Five levels were considered, from 0 to 4. To ensure consistent presentation of same viscosities, only industrial products were used. These were: mate tea (Chá Mate Leão®) for level 0; mango juice (Summer Fruit®) for level 1; strawberry-flavored yogurt (Itambé®) for level 2; chocolate syrup (Ice Cream®) for level 3; and strawberry-flavored yogurt (Danoninho®) for level 4. Each beverage was previously assigned a level using the IDDSI method with a syringe and stopwatch (30). After completing the questionnaire participants received an IDDSI primer in order to encourage the use of IDDSI standardization in clinical practice.
RESULTS
Sixty-five questionnaires were analyzed to characterize the sample. A total of 5 participants were excluded because they did not work with neurogenic oropharyngeal dysphagia. The sample, therefore, was composed of 60 participants. From this total, 33 (55%) participants reported they worked with NOD patients, and 27 (45%) mentioned they worked with both NOD and mechanic oropharyngeal dysphagia patients. Ages varied from 21 to 54 years, with an average of 33.8 years. They were mostly female therapists – 56 (93.3%), whereas 4 (6.6%) were male. The duration of their practicing with NOD patients varied from 1 month to 20 years, with an average of 5 years and 4 months. A higher concentration of participants was observed between 3 and 4 years of practice (31.66%). Most of them (48.33%) worked only in one workplace, 45.07% in two workplaces, and 6.60% in three workplaces.
Home care was the main workplace described (61.66%), followed by hospitals (48.33%). The population served varied, but the greatest demand was in the care of elderly individuals (73.33%).
There were no difficulties in identifying the viscosity for level 0. Most speech therapists (76.66%) identified and sorted the consistencies from 0 to 4, from thinnest to thickest, correctly.
Table I shows the viscosity sorting data, from thinnest to thickest. Most participants (49, 81.66%) properly sorted levels 1 and 2. Levels 3 and 4 were sorted properly by 57 (95%). It is important to notice that the number of incorrect sortings decreased as consistency level increased.
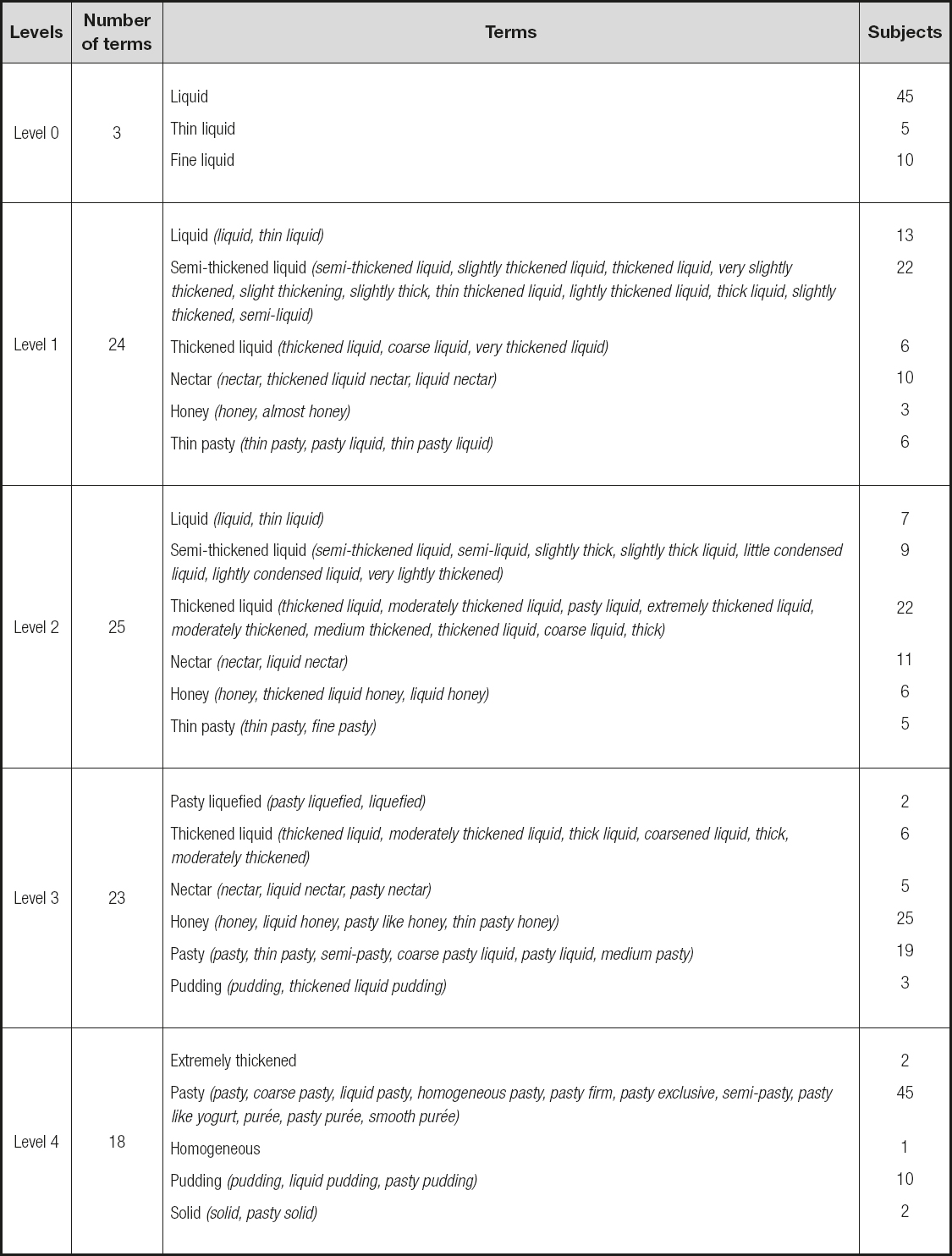
Table II lists the terminologies used to describe food viscosity. Concerning the terminology used by speech therapists, there was agreement between 45 participants (75%) on the terminology used to designate level 0. For level 1, 24 different terms were presented; for level 2 there were 25 terms; for level 3 there were 23 terms; and for level 4 the participants used 18 terms. In the analysis, the terminologies used were grouped together based on similarity, as shown intable II. The findings show that different terminologies are used to describe the same viscosity.
Level 0 (IDDSI - thin) was named by most participants as liquid; level 1 (IDDSI - slightly thick) was referred to as semi-thickened liquid; level 2 (IDDSI - mildly thick) was described as thickened liquid; level 3 (IDDSI - moderately thick or liquidized) was named as honey, and level 4 (IDDSI - extremely thick or puréed) was termed pasty by most subjects. A reduced number of participants used terms in accordance to IDDSI – level 0 by 5 subjects (8.33%); levels 1, 2 and 4 by 2 professionals each (3.33%); and level 3 by 1 therapist alone (1.66%). None of the subjects named all 5 IDDSI levels correctly.
DISCUSSION
Regarding the characterization of the sample, the results indicate that most speech therapists (61.66%) worked in home care. Home care was incorporated in Brazil in the 1980s, its guidelines focused on health promotion, conservation and rehabilitation in order to guarantee the health of the population (31). The inclusion of speech-language therapists in home care services is still recent, which explains the shortage of computations aimed at measuring the performance of these professionals (32).
In relation to the population served, the greatest demand for speech therapists is in the care of the elderly (73.33%). Researchers have pointed out that the older the age, the higher the incidence of dysphagia (7). Some studies conclude that it may be associated with anatomical and physiological modifications that promote the risk of disorders in the swallowing process (10). It is important also to consider the increase in this segment of the population, since the number of elderly people is about to exceed the number of people under five years of age (31). As the proportion of elderly people is increasing throughout the country, the high demand of speech therapists for health services is justified (33,34).
When analyzing the ability to sort the presented consistencies, most of the subjects performed the food progression properly, from thinnest to thickest. It was possible to infer that food visualization side by side facilitated sorting the food viscosity. A correct food viscosity identification is extremely relevant as it allows professionals to select the appropriate level to be used in each case (23).
Regarding the terminologies used by the speech therapists, the present study found a great diversity among the participants. Divergence in nomenclature could be seen at all levels, especially at level 2, which collected 25 different terms. The absence of standardization to guide both the preparation and naming of food consistencies results in a variety of nomenclatures in clinical practice (3,20,21,29), whereas a unified terminology provides patient safety and treatment efficiency (3,20,22). It is described in the literature that different consistencies result in crucial changes in the physiology of swallowing, such as reduced risk for aspiration (2,3,12-16). However, they may interfere with oral and pharyngeal transit time (2,9), and may be associated with food stasis (2,9,15) and with changes in the tongue force required for ejection of the bolus (2,10,17).
Diversity in terminology may make it difficult for other professionals, patients, or caregivers to understand and obtain the desired consistence. The extant lack of agreement in nomenclature among professionals, as evidenced by this research, may lead to different interpretations of food consistency prescriptions and to health damage for patients (3,20,29).
The modification of food characteristics such as texture and consistency (9,10) is one of the responsibilities of speech therapists in dysphagia rehabilitation, and a proper use of the available terminology is essential for professionals in this setting. Due to the diversity of terms found in this research, we supposed that most of the professionals participating in the study were unaware of IDDSI.
CONCLUSIONS
The professionals who took part in the study were assertive in sorting the progression of food from thinnest to thickest. The research evidenced the diversity of terminologies that speech therapists working with neurologic oropharyngeal dysphagia patients currently use. In clinical practice this fact represents a risk for patients, since it could lead to misunderstandings and errors in communication between professionals, patients and caregivers, to wrong or incomplete prescriptions, and to incorrect management of food consistency. Comparing the nomenclature proposed by IDDSI with those used by our professionals, there was disagreement between them. The study presented limitations due to the reduced number of participants. Therefore, it highlights the need for further research, aiming to check out the use of a unified terminology.