INTRODUCTION
The State must respect, protect, and facilitate the actions of individuals who seek to feed themselves in a dignified manner (1). In 2010, Brazil included food as a social right, making the State responsible to the courts for the sufficient and adequate supply of food, and enteral diets are supplied using the public pharmacies (2).
Nutritional risks permeate the whole cycle of human life, from conception to senescense, assuming several epidemiological configurations within the health/disease process. Thus, policies and actions aimed at food control as a component of full human development are of fundamental importance to health users (1,2).
There are several criteria established in the public health domain for dispensing enteral diets and nutritional formulas (4). Because they are expensive, these enteral foods are provided by state pharmacies, also known as "citizen pharmacies", an innovative model that is adept at pharmaceutical care (5).
Patients with difficulty swallowing and who fail to achieve their daily nutritional needs orally rely on these enteral foods to maintain their health (6). It is necessary to participate in the administrative process of the public pharmacy, and to comply with the criteria set out in a protocol to obtain these enteral foods (3).
Regarding the inclusion criteria for nutritional therapy, the law establishes that "patients are to be included exclusively in enteral nutrition when using long-term tubes for > 30 days" (criterion I), combined with at least one of the following clinical conditions: be a carrier of neoplasm that causes gastrointestinal tract obstruction (criterion II) or severe neurological dysphagia due to certain diseases (criterion III). Thus, the ordinance requires that at least two inclusion criteria be observed for the supply of enteral food to occur, and the criterion I is mandatory (3).
The literature is sparse on the supply of enteral food by state pharmacies; therefore, the profile of patients using this type of diet is unknown. Thus, in this study we aim to evaluate the supply of enteral diets, particularly how recipients comply with the ordinance, and the nutritional and social profiles of the users.
METHODS
A quantitative, descriptive, retrospective study was carried out with users who filed an administrative petition with the State Department of Health to obtain formulas for enteral nutrition. Espírito Santo has nine (9) "citizen pharmacies", and the analysis was carried out in seven of these pharmacies, which together comprise 73 % of the total enteral food supply processes in Espirito Santo (5-7).
A total of 1009 administrative processes for users who received enteral food between July 2013 and July 2015 were verified. After this process, a sample of 204 patients was delimited based on the inclusion and exclusion criteria. The inclusion criteria to delimit this sample were as follows: the users participated during the indicated period, which represents the most significant number of active processes; the physical documents were present on the premises of the pharmacy, were not dismembered or duplicated, and had not been transferred to other sectors, and the users received treatment for at least one year (5-7) (Fig. 1).

Figure 1. Study population and sample selected for application of the form in administrative processes.
The data were collected using a structured instrument (Fig. 2) with questions concerning the social profile, indicators of nutritional status, types of diet, routes of administration, reports, and base calculations for dispensation and use, in addition to the presence of compliance with the inclusion and exclusion criteria of delivery orders.
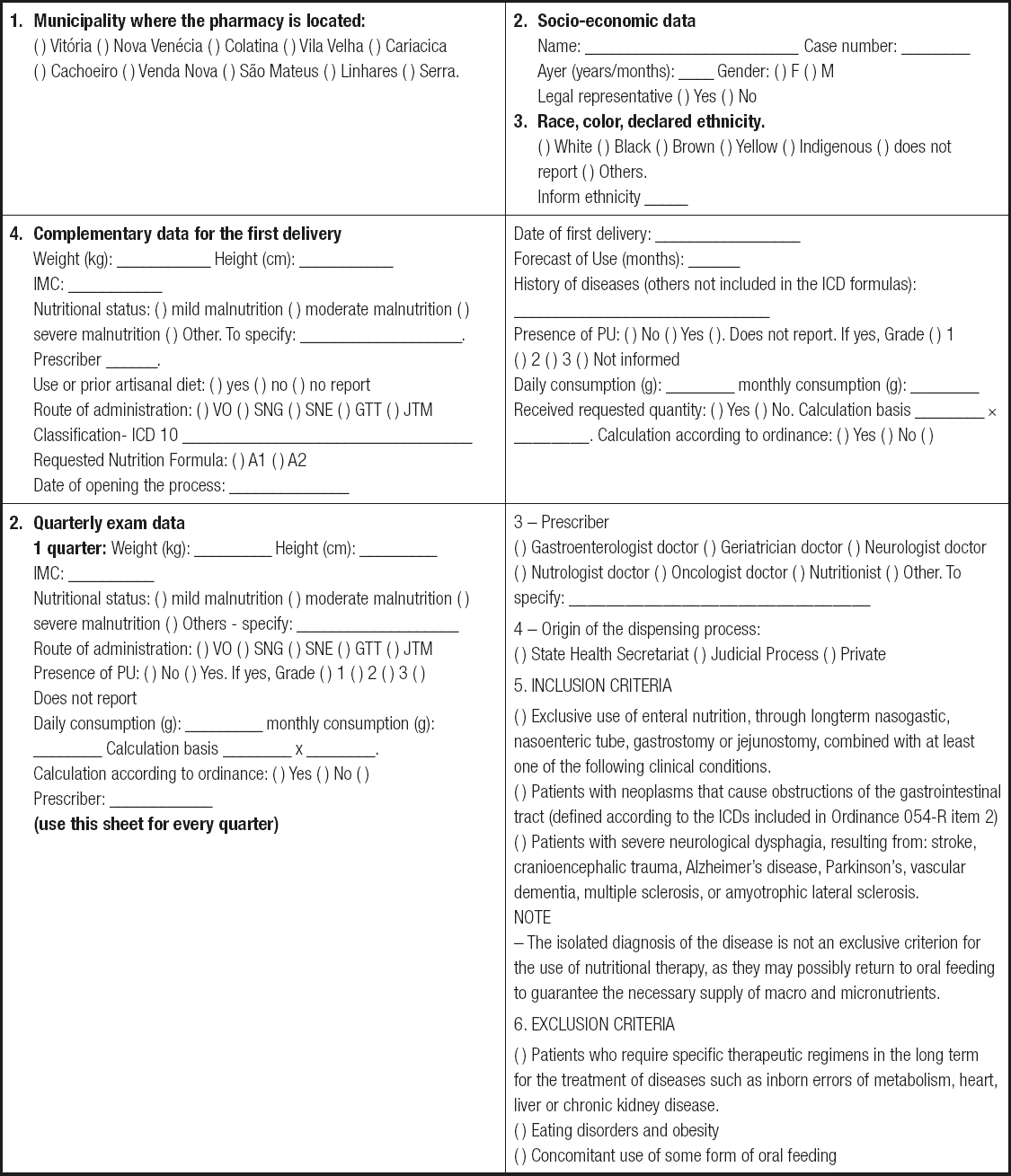
Figure 2. Analysis of the users' profile for the use of nutritional formulas: adolescents and adults.
By researching documentation we identified the required forms as well as the periodicity of requests, the delivery of nutrition, and the information contained therein. We used the same instrument just described for data collection. The data for each quarter were recorded and compared.
As the "base of calculation" parameter for the request is a prerequisite for acquisition, a survey was made of the processes that considered the anthropometric values and body mass index values that were indicative of nutritional status, and that were available in the documents collected.
The data were compiled through the EPiInfo™ program and later added to a spreadsheet in Microsoft Excel. A descriptive statistical analysis was performed, and the mean, standard deviation, and percentage parameters were determined.
This study was submitted to and approved by the Research Ethics Committee at Universidade Vila Velha (CAAEE number 45623815.8.0000.5064).
RESULTS
The profile of the population surveyed was composed of a balanced sample of women (51 %) and men (49 %), who were legally represented (91 %), with an average of 73.5 years (11-109 years), and with a mean weight and height of 56.72 kilograms and 1.60 meters (Table I). The predominance of women using healthcare facilities has been noted to be higher by several authors because women generally show more concern for health care, which may justify the higher frequency of women reported in this study (5).
Table I. Characteristics of the 204 subjects whose administrative processes were included in the research

The processes initiated by the Unified Health System (SUS) requesting the continuous use of enteral food treatment amounted to 53.5 %. The average daily intake was 367.05 g of enteral diet, corresponding to approximately 28 cans per month. In only 6 % of cases, attempts at artisanal feeding were recorded (9,10). The State of Espirito Santo made available seven standardized nutritional formulas, two for adults and five for infants and children (Table II).
Table II. Standardized nutritional formulas made available by the State of Espirito Santo, Brazil, and their dilutions

A1: nutritionally complete enteral diet, normocaloric, normoproteic, polymeric, lactose- and gluten-free, source of powdered caseinate protein for reconstitution; A2: nutritionally complete enteral diet, normocaloric, normoproteic, polymeric, lactose-free, gluten and sucrose, source of soy-based protein powder for reconstitution; F2: formula for semi-elementary infant feeding, based on protein hydrolyzate, whey, free of sucrose and gluten, suitable for children aged 0 to 12 months; F3: formula for elementary infant feeding, based on free amino acids, free of sucrose and gluten, suitable for children aged 0 to 12 months; P1: nutritionally complete diet, normocaloric, normoprotein, free from lactose, sucrose and gluten, suitable for children from 1 to 10 years old; P8: nutritionally complete diet, normocaloric, normoproteic, semi-elementary, free of lactose and gluten, based on peptides, suitable for children aged 1 to 10 years; P7: nutritionally complete diet, normocaloric, normoprotein, elementary, lactose-free, based on free amino acids, suitable for children aged 1 to 10 years.
In 100 % of the processes involved, the patient had some associated clinical conditions. The main diagnosis for the acquisition of diets was gastrostomy (55.2 %), followed by severe malnutrition and cerebrovascular accidents. Of these, 116 individuals (57.29 %) had at least three comorbidities, including hypertension, Alzheimer's disease, neoplasia, Parkinson's disease, diabetes mellitus, and chronic obstructive pulmonary disease. It was verified that 30 % of the respondents used a nasogastric tube for enteral feeding.
The use of gastrostomy, which was the predominant criterion (criterion I, Table III) for the request of nutritional therapy, was expected because the diseases and comorbidities reported were mostly chronic-degenerative, and required continuous, unlimited treatment (10). Therefore, these patients receiving prolonged treatment will use nutritional therapy (10). Although one of the criteria for inclusion in this study was one year of continuous treatment (4), 30 % of the patients used short-term feeding via a nasogastric tube.
Table III. Distribution of inclusion criteria among the patients assisted

*: patients are to be included exclusively in enteral nutrition using long-term tubes; †: carriers of neoplasia that causes gastrointestinal tract obstruction; ‡: severe neurological dysphagia due to certain diseases (criterion III).
The home care booklet provided by the Ministry of Health (15) notes that it is necessary to use gastrostomy when there is a need for long-term feeding, ranging from 3 to 6 months of enteral treatment. According to the inclusion criteria for this study (4), for at least one year of treatment, it was necessary to use a gastrostomy for diet infusion. In addition, the use of a long-stay tube was a criterion for supply. This aspect of the ordinance should be reviewed.
In their reports, few prescribers reported previous attempts at an artisanal diet. Nutritional formulas with enteral food (artisanal diets) may be indicated for clinically and nutritionally stable individuals with chronic diseases or for palliative treatment (10).
The ordinance requires all data of administrative processes to be completed (4). However, after our analysis, it was found that only 29 % (n: 59) of the processes had all fields completed during the enteral food treatment. In 85.8 % of the cases personal patient information was omitted, such as address, full name, and age; however, other information, such as gender, occupation, weight, height, and daily ingestion, were also missing. In contrast, it was found that during the period surveyed (July 2013 to July 2015), only 25 users had all the data correctly filled in.
The rate of missing data for body mass index, for example, was 60 % (n: 122) in the first trimester, and this decreased little in subsequent quarters, reaching 57 % in the last year surveyed. Other anthropometric data, such as measures of arm circumference and skinfolds, gastrointestinal function, tube condition, signs of infection, and others whose collection was recommended by the ordinance were omitted in 94.1 % of the processes involved (4).
The divergence of values for classifying nutritional status in the elderly results from a lack of a clear definition of the limits of body mass index for this stage of life (10), and the fact that body mass index may not adequately reflect the extent and distribution of adiposity. In this way, these missing data may reflect the difficulty that prescribers face when using this parameter to portray the nutritional reality of their patients. Therefore, it is necessary to update this aspect of the protocol.
It was verified that 80 % (n: 167) of the users presented with at least two inclusion criteria, as indicated in the diet reception order. However, 27 users received enteral feeding incorrectly because they presented with a single isolated criterion for feeding (I, or II or III) (4).
It should be noted that in 11 analyzed cases no inclusion criteria were present, and 21 additional individuals presented with exclusion criteria (Table III). The predominant exclusion criterion was concomitant use of some form of oral feeding, followed by eating disorders and obesity (4).
Regarding the protocol's inclusion and exclusion criteria that were not applied to 59 users, this finding was already expected because a previous study (9) indicated a low compliance with the protocol's inclusion criteria, which corroborates the data presented.
It was observed that in 51 % (n: 104) of the administrative processes evaluated there was a change in the height of the users according to the measurements performed in the quarterly evaluations. Of these, 45 patients exhibited greater heights than those at the first evaluation; since 9 were under 24 years old, the increase in height was to be expected. Surprisingly, in 16 patients, the height difference was greater than 10 cm, with only one of these subjects being under 24 years. Another 18 users had heights that decreased by 10 cm, with three of such patients under 24 years of age. These data indicate inconsistency in the recording of this parameter, which indicates that the calculations performed for verification of nutritional status may also be inconsistent (4). The impossibility of an individual to stand up in order to have height measured could be one of the reasons for these inconsistencies (11).
There were changes in patient follow-up data, as verified in the quarterly reports. According to our findings, more than half of the recipients had an increase in height, and 34 had increases or decreases by 10 centimeters. The incorrect estimation of weight and height leads to erroneous estimations of body mass index, which would have a direct influence on a patient's nutritional status; this factor would corroborate the absence of body mass index recordings in the patient information form (10). In all, 80 % of medical and nutritional records were correctly displayed in the investigated processes. However, despite the changes in weight and height just reported the enteral food treatment remained unchanged in half (51 %) of the processes over follow-up.
The changes in weight and nutritional status whose increase and consistency were verified indicate that the use of enteral diets may contribute to the maintenance of the nutritional status of patients and improve their quality of life; these improvements could occur without evidence of weight gain because the main International Classification of Diseases conditions that require diet requests are chronic-degenerative diseases associated with other comorbidities (10).
It was verified that the weights of 17 % (n: 35) of the subjects did not change over one year of treatment. However, there was a decrease in the weights of 34 % (n: 69) of those investigated in the first trimester of treatment. Weight gain was verified in 20 % of the patients in the first trimester of enteral food treatment. Nutritional status remained constant during one year of treatment in 63 % (n: 129) of the subjects.
Although there was no correlation among changes in the physical exams, it was verified that the quarterly follow-up visits of users were not attended to by a single professional. It was observed that 83 % of the users had more than two prescribers over three quarters (three reports and at least two different professionals). This change might not allow adequate patient follow-up.
Few studies indicate compliance with the protocol and supply of this type of enteral food in public pharmacies. Consequently, information has been obtained from studies that observed other protocols for dispensing mainly medicines. It was found that the profiles of those assisted by these public pharmacies are similar to those of previous studies involving other protocols in Espírito Santo pharmacies (6).
CONCLUSION
There were several gaps in the processes of pharmacies supplying enteral foods to citizens of Espirito Santo due to the absence of some essential data required by the ordinance. Although the inclusion criteria were complied with in almost 80 % of cases, 15 % presented with problems that would end nutritional treatment. In addition, a need for adjustments to the current protocol is noted due to the use of non-effective parameters for the follow-up of patients; a higher degree of vigilance by prescribers and pharmacists at citizen pharmacies alike is required for this therapy. Finally, putting the issue on the table already implies benefits in terms of improvement of health services.














