Introduction
In 2020, together with the new disease denominated COVID-19 some social norms were implemented to avoid the transmissibility of the virus SARS-CoV-2. Nevertheless these new routines were accompanied with an increase in the co-occurrence of mental health disturbances mainly by either the subjects what had direct contact with the disease (Sun et al., 2021). Recent studies associate the intensity and prevalence of these mental disturbances generated by the COVID-19 with variables such as socio-demographic features, cultural models, geographical conditions, the media as well as the public policies implemented in each region for its containment, among others, notwithstanding little is to known about the prevalence and impact in serious patients infected by the virus (Canet-Juric et al., 2020; Erman & Medeiros, 2021; Zheng et al., 2020). In the case of Mexico, a country with single cultural and socio-demographic features, the first contagious by COVID-19 was confirmed in February 2020 and some days after the Mexico government declared a national health emergency implementing actions and suggestions for avoiding the spread of virus in focused on the social distancing, sanitation and hygiene as well as an active social communication. Since the early phase of COVID-19 spread different social and individual phenomena such as panic, uncertainty, changes in the routine and social isolation were observed contributing to alter the mental health of Mexican population similar as it happening in other regions in the world (Varma et al., 2021) which could be explained by an increase in the demand for mental health services and whose recurrence is related to the temporal evolution of the COVID-19 pandemic (Jacobson et al., 2020; Titov et al., 2020). Several studies describe the mental health degree in specific sectors however there is little information about the emotional and mental state of the individuals affected directly by the pandemic including to the infected and their families. COVID-19 is a highly contagious disease that encompasses a wide spectrum of clinical manifestations (Chen et al., 2020; Delsante et al., 2020; Dorrell et al., 2020; Gandhi et al., 2020; Gottlieb & Long, 2020; Josephson & Kamel, 2020; Kunutsor & Laukkanen, 2020; Rahman et al., 2021) but in particular is associated with the acute respiratory syndrome that evolves to severe cases and that require hospitalization which additionally is a traumatic and exhausting process for individuals involved. It is well known that admission patients with dyspnea and hypoxemia to urgency are classified as suspected cases of COVID-19 (Du et al., 2020) so they are treated by specialized personnel with personal protection equipment, who record the clinical history of the patient and request for complementary studies such as radiography, high-resolution tomography and laboratory analysis to confirm the diagnosis or severity of the health condition (Abbasi-Oshaghi et al., 2020). According to the World Health Organization (WHO), a severe case of COVID-19 is who presents at least one of the following conditions: (1) respiratory rate ≥ 30 breaths / min, (2) oxygen saturation ≤ 93% at resting position and (3) an oxygenation index (PaO2 / FiO2) ≤ 300 mmHg. The hospitalization process in the COVID area involves the full isolation of the patient, without access to familiar visits, being the last moment in which the family member maintains visual and direct communication with the patient. Based on this scenario, it is possible to anticipate that the visual impact promotes an altered emotional state. During this pandemic, people directly affected as patients hospitalized by COVID-19 and family members are more susceptible to developing disorders in their emotional state compared to other sectors of the population that have not gone through this experience. The emotional impact has been assess through psychological instruments such as structured interviews which allow translating their responses into numerical and categorical values allowing relate it with another variables and some examples are the surveys based on DASS-21 Scale (Depression, Anxiety and Stress Scale) or PSQI Scale (Pittsburgh Sleep Quality Index) (Bhat et al., 2020). Recent studies, has reported that it scale has already been used to analyze the impact on the emotional health of specific sectors of the population during this pandemic (Bhat et al., 2020), for example, students (Odriozola-González et al., 2020), teachers (Vulić-Prtorić et al., 2020), children (Orgilés et al., 2020), etc. (Al Zubayer et al., 2020; Bautista et al., 2012; Medina-Mora, 2020) including the bulk of Mexican population (Cortés-Álvarez et al., 2020). However, to date it has not been applied to patients hospitalized by COVID-19 due to the physical difficulties to establish communication with these patients, so there are only few reports that indicate its prevalence and severity degree. Some of these studies point to a substantial increase in levels of depression and anxiety in patients with COVID-19 (Seyahi et. al 2020). For another hand, the evaluation of the mental health of patients is relevant because depression, anxiety or stress are associated with a higher risk of post-traumatic stress days after the hospitalization event (Matalon et al., 2021). On the other hand, Mexico has a particular socio-cultural composition from those of the rest of the world, so that the exploration of these variables could show new insights to support local public health strategies aimed at mitigating the psychological effects of the COVID-19 pandemic. In this research, we explore the mental health of two groups of subjects directly involved with the disease and highlight the impact in the Mexican population of the most relevant health public emergences in our times to this assess the prevalence of depression, anxiety and stress among patients or relatives of infected individuals during the pandemic of COVID-19 in Mexico City.
Methods
Study design and research population
This study was cross-sectional conducted from April 1st, 2020, to September 30th, 2020, in the Hospital Juárez de México, located in Mexico City. Participants were divided in two groups: (I) constituted by hospitalized patients with COVID-19 and (II) constituted by relatives with hospitalized patients with COVID-19. Selection criteria by groups were: Group I: Participants were chosen based on following two eligibility criteria: a) COVID-19 hospitalized patients with clinical confirmation using the current gold standard method (PCR-RT for SARS-CoV-2) (Abbasi-Oshaghi et al., 2020) and who have a medical history characterized by fever, cough, sore throat, malaise, myalgia, anorexia, nausea, diarrhea, anosmia and ageusia and patients who volunteered could participate and with ability for responding to the questionnaire. As exclusion criteria: patients with respiratory impairment or patients with non-invasive mechanical ventilation and patients or those patients who refused to answer the survey. Group II: Relatives that had with COVID-19 patients ( ≥ 18 years). The familiar relationship between groups were avoided. All participants provided informed consent when they entered the hospital and at research meet.
Sample size and data collection
Forty-five Mexican hospitalized patients diagnosed with COVID-19 from Hospital Juárez de México in Mexico City were selected and in the same temporal frame fifty-five relatives of COVID-19 hospitalized patients. A convenience sampling technique was carried out to recruit patients and relatives not related between them, according to their availability and accessibility in the Hospital. First, a team of physicians applied the survey and psychological instruments face-to-face with each patient after to sign in the informed consent and on the other hand, the psychologist team recruited the relatives for application of survey and instruments. This study was reviewed and approved by Committee of Hospital Juárez de México, CDMX (Register Number: HJM 0796 / 20-I) and conducted in compliance with the Declaration of Helsinki and Mexican Official Norm NOM-012-SSA3-2012.
Survey and psychological assessment
A survey was structured by three sections: the first one recollected socio-demographic data such as age, gender, comorbidities, hospital outcome. Additionally, respondents were interviewed about three open questions about their mood and recorded the first adjective that described their situation. Questions were: (1) What is the mood that describes how do you feel? (2) What is the hardest situation that you are going on right now? and (3) What or who is your main motivation? Later, in the second section, the socioeconomic status was calculated according to the Mexican Association of Market Research (AMAI) based on the Survey conducted by the National Household Income and Expenditure Survey (ENIGH) (INEGI, 2018) and used this information to generate six levels associated with the quality of life and well-being of the participants. We applied a new segmentation to reduce the number of levels we classified in (1) “predominantly high” constituted by AMAI A/B, C+ who are characterized with lifestyles where they spend a higher percentage of their income to transport and education and a lower proportion for feeding expenses compared to the other socioeconomic levels; (2) “predominantly middle” constituted by AMAI C and D+ which is characterized for a lifestyle that reflects optimal sanitary conditions, basic internet access and mobility either in public or private transport and with consumption habits where they dedicate almost a third of their income in feeding and (3) “predominantly low” constituted by AMAI D and E who are characterized by allocating about half of their income to food, with a low level of schooling by parents, with limited internet access and mobility mainly by public transport. Finally, in the third section, DASS-21 is a self-report instrument (Depression Anxiety Stress Scale), it consists of a self-report instrument comprising 21 items, completion takes 10 to 20 minutes and have an adequate and demonstrated internal consistency (Cronbach´s α: .761 to .906) and that evaluate three psychological domains: depression, anxiety and stress (Oei et al., 2013). DASS-21 instrument scored as follows: normal (0-4), mild (5-6), moderate (7-10), severe (11-13), and very severe (14) for depression subscale; normal (0-3), mild (4-5), moderate (6-7), severe (8-9), and very severe (10) for anxiety subscale and finally, normal (0-7), mild (8-9), moderate (10-12), severe (13-16) and very severe (17) for stress subscale.
Statistical analyses
Descriptive statistics was used for report proportions and percentages for categorical variables and means and standard deviations for continuous variables. Sociodemographic characteristics and severity of mental health in patients and relatives were reported as proportions and chi-square test were used for identifying statistical association with a confidential level at 95%. Univariate generalized linear model with a main effects model (linear regression) was used to measure the associations between socio-demographic characteristics with regard the DASS-21 subscales scores. Associations were presented using beta coefficients, confidence intervals and p-values. Logistic regression analysis was carried out to find the association of socio-demographic data and mental health evaluations. Results were reported as odds ratios (ORs) with 95% confidence intervals. P-values tailed less than .05 were considered statistically significant. Our data were analyzed using SPSS V. 27.0 and GraphPrism V. 17.0.
Results
Sociodemographic and socioeconomic characteristics
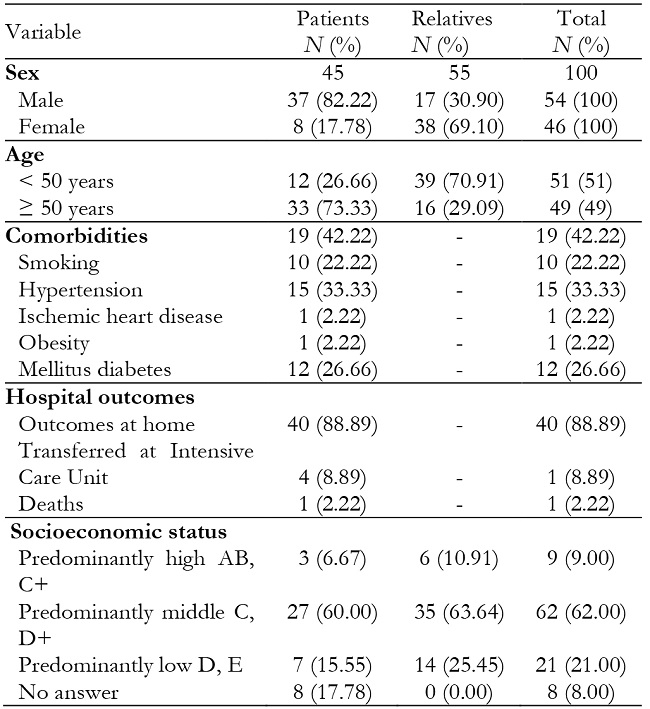
A total of 100 participants were divided in two independent groups identified as hospitalized patients with COVID-19 and relatives. Sociodemographic features of both groups were presented in Table 1. The majority of patients were male (82.22%) with mean age of 54.4 ± 9.6 years, while the relatives were 38 females (69.10%) with mean of 43.2 ± 11.8 years. Regarding the comorbidities in patients with COVID-19 they showed that 33% have arterial hypertension, 27% have diabetes mellitus and 22% are smokers. Other comorbidities such as ischemic heart disease and obesity were identified in less than 2% for patients. None of the patients and relatives had any psychiatric illness and none used psychotropic drugs (Table 1). The socioeconomic analysis showed that the majority of the population was allocated in the predominantly middle level in patients group (60%) and in relatives group (64%) which is characterized for a lifestyle that reflects optimal sanitary conditions, basic internet access, mobility either in public or private transport and with consumption habits where they dedicate almost a third of their income in feeding (Table 1).
Qualitative psychological assessment in COVID-19 patients and relatives
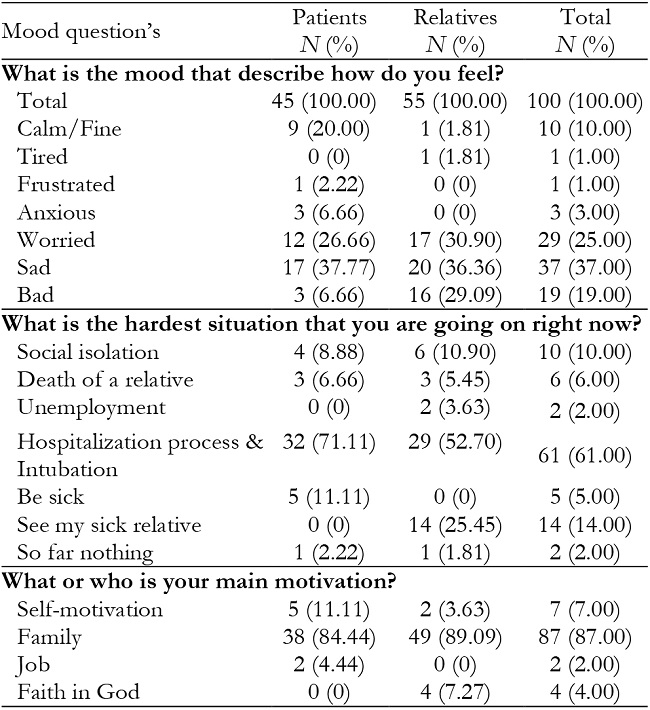
An initial introspection allowed us better communication face to face with patients breaking the sociocultural barriers that limit the expression of feelings and emotions by the male gender. About the first question, the answer most recurrent provided by patients were feeling worried (26.7%), sad (37.8%) and calm (20.0%) while that in relatives the expression of emotion was described as worried (30.9%), sad (36.4%) and bad (29.1%). About the second question, the hardest situation for the patients were “be sick” (71.1%) and in the relatives, was the hospitalization process of their relatives (52.7%). In the last question, both patients (84.4%) and relatives (89.1%) placed the family as the main motivation to overcome the situation (Table 2).
Assessment of depression, anxiety, and stress in patients with COVID-19 and relatives
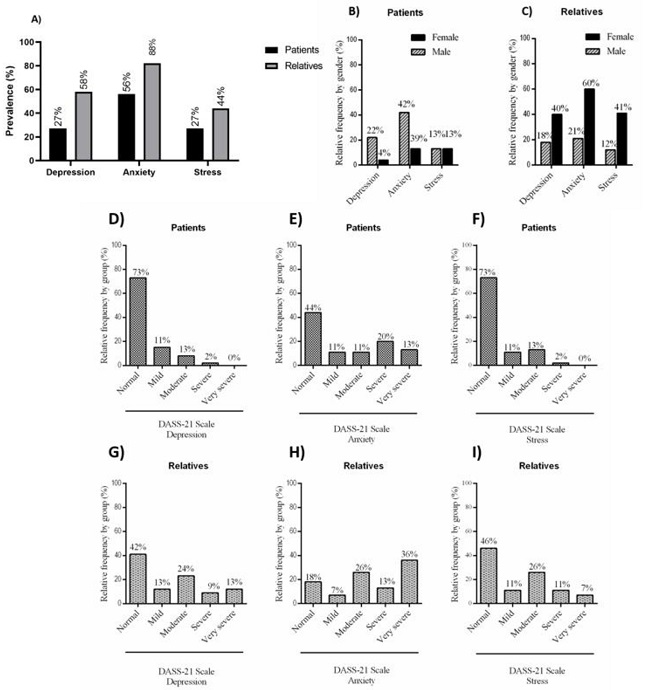
The depression, anxiety and stress assessment by COVID-19 patients and relatives was measured using the DASS-21 survey. In patient’s group was found a prevalence of 27% of depression, 56% de anxiety and 27% with stress; regarding to relatives´ group 58% has been identified with depression, 82% with anxiety and finally 44% of relatives with stress (See Figure 1A). In patient´s group, analysis by sex showed that women relatives had low levels of depression (4%) but elevated levels of anxiety (30%) and stress (13%) while men had levels high of depression (22%), anxiety (42%) and stress (13%). Regarding to relative’s group, they had levels higher of depression (40%), anxiety (60%) and stress (41%) while in men participant´s we identified traits of depression (18%), anxiety (21%) and stress (12%). (Figure 1B, 1C). DASS-21 scores in patients group: 27% presented traits of depression (mild = 11%, moderate = 13%, severe = 2%), the 56% anxiety (mild = 11%, moderate = 11%, severe = 20% and very severe = 13%) and 27% any traits of stress (mild = 11%, moderate = 13%, severe = 2% ) in contrast with as relative´s group we identified that 69% reported traits of depression (mild = 13%, moderate = 24%, severe = 9% and very severe = 13%), 82% anxiety (mild = 7%, moderate = 26%, severe = 13% and very severe = 36%) and 44% traits of stress (mild = 11%, moderate = 26%, severe = 11% and very severe = 7%) (Figure 1D-1I).
Association of depression, anxiety and stress with sex, age and socioeconomic level
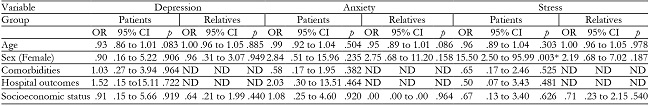
In our analysis, patients and relatives by sex only was found a significant association for male participants in both groups in anxiety subscale DASS-21 (p = .001), in other subscale were not found associations. For female participants were reported a significant association with subscale depression (p = .0001), anxiety ( p => .0001) and stress (p = .003) (Table 3). Regarding to age of participants, data shown a significant association in prevalence of DASS-21 for depression (p = .001), anxiety (p > .001) and stress (p = .004) in < 50 years between patients in comparison with relative´s participants, regarding to ≥50 years subgroup, only was found a significant association in subscale anxiety (p = .028) between patients versus relatives. Subsequently, in the analysis of association between socioeconomic status in patient´s and relative´s groups were found that predominant middle level (C, D+) was associated in patients and relatives (p = .003) in subscale depression and stress (p = .023) and predominant low level (D, E) (p = .012) were associated with higher score in anxiety subscale, related to subscales depression, anxiety and stress were not found any associations with high level (A, +) (Table 3). Finally, for comorbidities in patients, significant association was not found (Table 6).
Risk factors for depression, anxiety and stress in patients hospitalized by COVID-19 and relatives
This research identified that the relatives of COVID-19 patients show a probability four times higher to have traits of mental health disturbances (Depression OR = 3.83, CI (1.63, 8.96) p = .002; Anxiety OR = 3.60, IC (1.46, 8.88), p = .005; Stress OR = 3.30, IC (1.41, 7.70), p = .006) (Table 4). Comparing subjects by age ( < 50 versus older ≥ 50 years) we identified a probability almost three times to have traits of depression in the younger people compared with older people (OR = 2.99, (1.31, 6.80), p = .009), anxiety (OR = 2.83, (1.15, 6.93), p = .02) and finally in our analysis clustered by sex we shown that gender of participants was a risk factor to suffer anxiety (OR = 4.13, (1.57, 10.89), p = .004) and stress (OR = 5.38, (2.27, 12.8), p = .002) (Table 5). Regarding socioeconomic status, it was not found as a risk factor for participants. In subsequent analysis by sociodemographic characteristics for patients and relatives’ group, only was found a significant association in female participants (OR = 15.50, (2.50, 95.99), p = .003) with a high score in stress subscale DASS-21; about other characteristics were not found association.
Table 3: Association of depression, anxiety and stress scales DASS-21 with sociodemographic characteristics in both groups.
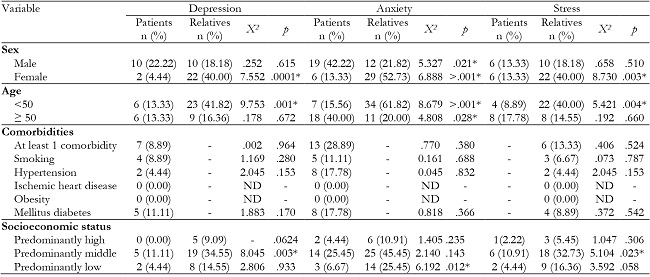
Data are expressed as mean and standard deviation. p-value < .05 show significance statistics (*). ND = Not determinated.
Table 4: Associations between sociodemographic variables and DASS-21 in patients and relatives.
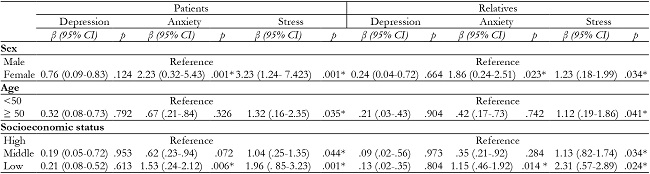
Beta value (β) and significance level of Logistic Regression Analysis. Data are expressed as mean and standard deviation. p-value < .05 show signifi-cance statistics (*).
Table 5: Logistic regression analysis to evaluate quantitatively the influence of age, gender and sub-groups in the emotional state of individuals questioned. p-value < .05 show significance statistics (*).
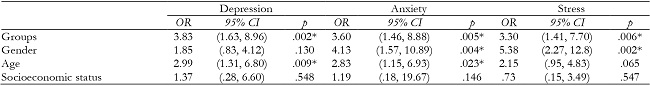
Reference group: relatives / patients; gender: women / men; age: younger < 50years / older ≥ 50 years; socioeconomic status: middle / total. N=100, p-value < .05 show significance statistics (*).
Discussion
The aim of the present report was to determine the prevalence of stress, anxiety and depression within patients hospitalized by COVID-19 as well as their likely association with the emotional impact received by relatives with hospitalized patients by COVID-19 through a transversal and observational study during the second wave of COVID-19 in Mexico City. Our data shown a high prevalence of depression, anxiety and stress in both group with high values compared with other groups under study such as students, teachers and children including to the bulk of the Mexican population. Moreover, some reports based on DASS-21 survey for other regions revealed equivalent results in hospitalized patients by COVID-19. For instance, a validated version of DASS-21 applied in a number of individuals similar to this report but in Persian subjects showed a high prevalence with severe and very severe cases of anxiety and stress in hospitalized patients by COVID-19 in Alborz, Iran (Zandifar & Badrfam, 2020). However, DASS-21 is a flexible instrument with a good internal consistency, it could has a divergent validity for different racial groups including Hispanic and Latin subjects (Norton, 2007). Despite this, currently different translated version of DASS-21 has been applied in several population including Mexican subjects with sample size since hundreds to thousands of subjects being in all cases comparable with another validated surveys (Daza et al., 2002; Bados et al., 2005; Dosil-Santamaria et al., 2022; Kumar et al., 2018; Raza et al., 2020). In this sense, prevalence of depression, anxiety and stress also are comparable with values reported by the frontline medical staff after attendance continuously to patients with COVID-19 (Guo et al., 2021; Robles et al., 2020). We suggest that the hospitalization process trigger an emotional mechanism when the individuals have a direct interaction with the disease into hospitals similar to another traumatic medical experiences (Agarwal et al., 2020). Probably, because the hospitalization by COVID-19 could generate a mental link between hospitalization and fatal outcomes due to a lot of reports confirming a high prevalence of comorbidities in the hospitalized patients (Prado-Galbarro et al., 2020). Some demographic variables have already been associated with the emotional state during this pandemic and correspond mainly to age, gender, ethnicity, among others (Proto & Quintana-Domeque, 2021), however, so far little is known about these variables in a specific context as Hospitals in Mexico City. In this study, we have identified an association between levels of emotional states and the age of patients when they are submitted in an experience of hospitalization. Also, data revealed at least three times more probability to show high scores in depression and anxiety subscales in DASS-21 in patients with an age less than 50 years old, however, no evidence was found that state of stress is associated with age. These findings in which young people are more susceptible to emotional disturbances was also reported in an international cross-sectional study shown that although older adults are more vulnerable to the SARS-CoV-2 virus are young adults who have a major risk of be affected in their mental health (Stanton et al., 2020; Varma et al., 2021). This association could be related with the lifestyle, productive activities, physical activities including a break in the social activities preferentially in focused to younger people while older people is not deeply affected being that they are the community most oriented to other activities which have been less impacted by COVID-19 pandemic such as housing, nonphysical activities, etc. (Harangi-Rákos et al., 2022).
In the same way, this study identified a relation between mental health and gender in where women have almost four times most probability to have high score in anxiety subscale and more than five times of probability to have high score in stress subscale in comparison with male gender so that likely new components could add emotional load contributing to the prevalence of anxiety and stress such as the cultural component when we consider the fact that the Mexican family system is mainly matriarchal, which adds an emotional load to female gender because they are family heads (Acuna-Zegarra et al., 2020). Additionally, several reports confirm that women could be affected by the pandemic due to changes in the workplace, work overload at home, in addition to the fact that have been showed women are more vulnerable to contagion by relatives (Burki, T. 2020; Riello et al., 2020). Some studies in Italy and Spain reported that 66% and 72% of infected healthcare workers are women versus 34% and 28% of men respectively, reflecting that gender has a special role in the development of mental illness during this pandemic (Burki, 2020). This study shown that the emotional state of relatives is associated with the physical health of their patients during the hospitalization process and this could be explained for a close relationship which is based on the concept of family considered by Mexican society as the mesh of its social structure (Zeiders et al., 2011) revealing here a new characteristic that could significantly affect emotional states when one of its members undergoes is sick due to the SARS-CoV-2 virus. Reinforcing this idea, this study findings qualitative and narrative were associated with the prevalence of each psychological component DASS-21 which agrees with other studies conducted during the pandemic which is useful to reveal indicators about negative emotional conditions such as irritability, insomnia, altered ability to maintain in focused and even anxiety and depression (Salari et al., 2020). Moreover, this interaction that exists between relatives and their patients during the hospitalization has been little reported because the conception of this institution is varied for the different geographic areas, however in the case of Mexico, this aspect was relevant because the values of the Mexican family as well as their beliefs contribute to processes of resilience to adverse events. In this sense, the family could provide to members a positive attitude towards life, despite unfortunate circumstances as well as a protectionist feeling invaluable against traumatic events such as the hospitalization process so that could affect entire families and not just patients (Bermudez & Mancini, 2013). In comparison between patients and relatives, we identified in relatives the existence of a higher prevalence of anxiety that includes a very severe degree. Interestingly, results revealed a significant association between the group of participants with hospitalized relatives with a major susceptibility to have symptoms of anxiety, depression and stress in contrast with hospitalized patients group themselves, additionally data revealed a risk until four times more to suffer an emotional impact (Beck et al., 2021) . Relatives who have any family member in hospitalization could assume a caregiver role implying the acquisition of new emotional loads associated with responsibility (Zarit, Reever, & Bach-Peterson, 1980). New evidence has been identified using new tools such as the COVID-19 Caregiver Limitation Scale (CCLS-9) as the COVID-19 added to the stress and pain of the caregiver (Sheth et al., 2020). This pandemic contains new components not quantified previously and provides new ways to increase the emotional load in relatives that is not shared with theirs patients and one of its could be the perception of this disease in a new context generated by the rapid acquisition of information showed by television and digital media, another for the visual impact for the clinical management of patients, low knowledge related with the COVID-19 and high association with the comorbidities and fatal outcomes in hospitalized patients with COVID-19.
On the other hand, the COVID-19 pandemic has generated a strong direct impact on mental health, psychological and financial situation on patients and their relatives, due to diverse reports that indicate that socioeconomic situation of patients and relatives could affect their emotional states when they in face the high cost of hospitalization processes and in general when they live the experience of being groups affected by COVID-19 (Pedrosa et al., 2020). For example, in the United States, at least one in ten adults has reported effects on their mental health, whether for economic reasons, including the loss of a job, the health of their relatives and increasing the incidence of sleep disturbances, a change in eating habits and the increase in substances of abuse as well as alcohol (Medina‐Mora et al., 2021). We not found association between socioeconomic level with impact in mental health, but that revealed a trend for participants low-income levels with higher scores in DASS-21 (Pieh et al., 2020). Studies previous have reported that the socioeconomic level is associated with the tranquility and well-being that directly affects the emotional state (Mena et al., 2021). Therefore, we consider that the evaluation of mental health in our sample could have cultural aspects and nested social models that operate above the socioeconomic level, such as family or religion (Koenig, 2020). However, our work provides some limitations, especially due to the lack of knowledge about the dynamics of contagions at the national level reported at the moment of the surveys and in general because of how much we still need to learn about this new disease in the both frames pre and post-vaccination era, additionally , the result of this study may not be generalized for a national context because of the potential sample selection bias arising from the data of COVID-19 cases admitted to the healthcare center. However, Mexico has been one of the countries most affected by the pandemic and we believe that this work will be able to offer another perspective about what happened a few months ago in the hospitals of Mexico City, which can help generate proposals more complex to quantify mental health levels and its mitigation as reinforce mental health services, establish community support networks including self-help groups specially for vulnerable groups, communicate actively about the new medical advances against COVID-19, enhance as soon as be possible some aspects basic of the social dynamic (Tayyib, 2021; Tausch et al., 2022). Another limiting of this work, it was that the interviews were conducted during the clinical course of COVID-19 in patients who required hospitalization showing only a temporal point that should be extended to future dates to achieve a complete understanding how the contagious chain could impact the mental health of this population. However, there is still a long way to advance in the unlockdown and many of these emotions that surround the pandemic could become more acute over time. This evidence together additional cross-sectional studies can help to describe better the emotional impact in mental health at individual and collective level of the COVID-19 pandemic in Mexican population and provide unknown faces for other regions to support new strategies to mitigate its damage.
Conclusions
This research carried out during the ascent of contagious in the second wave of COVID-19 outbreak in México revealed an association between emotional disturbances such as anxiety, stress and depression in individuals involved in the hospitalization process by COVID-19. We concluded that our sample of COVID-19 patients maintain a high prevalence of mental alterations and some factors such as age, gender and socioeconomic status contribute to modify the magnitude of these perturbations.