My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 n.10 Madrid Oct. 2006
CARTAS AL DIRECTOR
Development of hepatocellular carcinoma (HCC) in peginterferon and ribavirin HCV-infected cirrhotic treated patients
Aparición de carcinoma hepatocelular en el curso del tratamiento con interferón-pegilado y ribavirina en pacientes con cirrosis secundaria al VHC
Palabras clave: Carcinoma hepatocelular. Interferón. Ribavirina. Virus hepatitis C. Cirrosis.
Key words: Hepatocellular carcinoma. Peginterferon. Ribavirin. Hepatitis C virus. Cirrhosis.
Dear Editor:
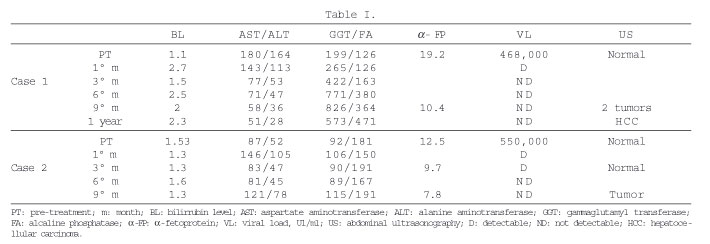
Antiviral therapy for chronic HCV has improved in the last few years, particularly with the introduction of the pegylated form of interferon and its combination with ribavirin (1). This improvement has also been demonstrated in the group of patients with advanced disease (i.e. bridging fibrosis and compensated cirrhosis). Despite the potential for serious adverse events during therapy, particularly infections and cytopenias, antiviral treatment is frequently started in this subgroup population, and is also tried in the candidate for liver transplantation. In patients with compensated cirrhosis, the major aim of therapy is to eradicate the infection and, in doing so, to prevent/revert the progression of disease and HCC development (2,3). Indeed, it has been suggested that the prolonged suppression of viral replication might reduce hepatocyte turnover and subsequently the risk of cancer (2,4,5). We report two cases of patients who, in contrast to what is typically observed, developed a hepatocellular carcinoma while on antiviral therapy, after achieving a virologic response with clearance of viral nucleic acid from the serum. In both cases, the pre-treatment liver biopsy showed avanced hepatitis with cirrhosis and, in both the infecting genotype was HCV 1b. Treatment was followed by improvement in liver tests with progressive reduction in transaminase levels and early virologic response. However, an ultrasound performed in the 9th month of treatment showed the development of an HCC, despite the virologic response with negativization of HCV-RNA in serum at 3 and 6 months, respectively (Table I).
The incidence of HCC (5.5-15 per 100,000 population), considered the most common primary liver cancer in the world (564,000 cases/year), is increasing worldwide mainly because of the dissemination of HCV infection. Cirrhosis, mostly of viral origin, is the strongest predisposing factor for its development (6). In fact, once cirrhosis is established, screening of HCC based on ultrasonography every six months, is recommended in order to make an early diagnosis when a potentially curative treatment is more likely. In addition, the elimination of the cause responsible for liver disease, particularly HCV and hepatitis B virus, might further prevent the development of HCC among cirrhotic patients (6). Up to date, two meta-analysis based on Japanese and European population have been published that compare the incidence of HCC between interferon-treated and untreated cirrhotic patients. Despite the fact that the results were not fully conclusive, a lower incidence of HCC is observed among virological and biochemical responders (2,3).
One less debated aspect in the literature is the development of HCC in virologic responders (7). Thus, regardless of viral clearance and, even though the treatment might induce fibrosis regression, it is very important to continue screening for HCC in cirrhotic patients on antiviral therapy. Screening in these patients should possibly be the same to that performed in other cirrhotic patients, that is ultrasonography every 4-6 months (6). Furthermore, from a clinical point of view, both examples raise the issue of the potential complications in treated-cirrhotic patients which not strictly related with the administration of interferon and ribavirin.
In conclusion, in HCV-treated cirrhotic patients, the management of the frequent antiviral-related side-effects should not let us forget about complications of the natural history of cirrhosis.
M. Iborra Colomino, V. Aguilera Sancho-Tello and M. Berenguer Haym
Service of Hepatogastroenterology. Hospital Universitario La Fe. Valencia
This work was supported in part by grant C03/C02 of Red Nacional de Centros de Investigación en Hepatología y Gastroenterología (RNIHG), Instituto de Salud Carlos III.
References
1. Hadziyannis S, Sette H, Morgan T, Balan V, Diago M, Marcellin P, et al. Peginterferon alfa-2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med 2004; 140: 346-55.
2. Camma C, Giunta M, Andreone P, Craxi A. Interferon and prevention of hepatocellular carcinoma in viral cirrhosis: an evidence-based approach. J Hepatol 2001; 34: 593-602.
3. Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: National surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. Ann Intern Med 1999; 131: 174-81.
4. Sypsa V, Touloumi G, Papatheodoridis GV, et al. Future trends of HCV-related cirrhosis and hepatocellular carcinoma under the currently available treatments. J Viral Hepat 2005; 12 (5): 543-50.
5. Donato MF, Degott C, Arosio E, Martinot M, Monti V, Morabito A, et al. Interferon-alpha suppresses liver cell proliferation in patients with chronic hepatitis C virus infection. J Viral Hepat 2005; 12 (5): 499-506.
6. Solís-Herruzo JA, Solís-Muñoz P. Hepatitis virus and hepatocellular carcinoma. An Med Interna 2005; 22 (4): 157-61.
7. Makiyama A, Itok Y, Kasahara A, Imai Y, Kawata S, Yoshiota K, et al. Characteristics of patients with chronic hepatitis C who develop hepatocellular carcinoma after a sustained response to interferon therapy. Cancer 2004; 101 (7): 1616-22.