My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 n.2 Madrid Feb. 2009
Colonoscopy quality assessment
Valoración de la calidad en la práctica de la colonoscopia
S. Morán Sánchez, E. Torrella1, P. Esteban Delgado1, R. Baños Madrid2, A. García3, A. Ono2, E. Pérez Cuadrado1, P. Parra4, J. Cruzado Quevedo5, F. Pérez Riquelme5 and F. Carballo Álvarez2
Department of Digestive Diseases. University Hospital Santa María del Rosell. Cartagena, Murcia.
1University Hospital Morales Meseguer. Murcia.
2University Hospital Virgen de la Arrixaca. Murcia.
3University Hospital Reina Sofía. Murcia.
4Dirección General de Calidad Asistencial. Consejería de Sanidad de la Región de Murcia.
5Dirección General de Salud Pública. Consejería de Sanidad de la Región de Murcia. Spain
This study was supported in part by a grant from the EMCA program of "Fundacion para la Formacion e Investigacion Sanitarias de la Región de Murcia", Ministerio de Salud, Región de Murcia.
ABSTRACT
Aim: colonoscopy has become accepted as the most effective method for colon exploration. Some application problems have been detected in the setting of normal clinical care due to its wide range of uses in recent years, and therefore there is a need to measure colonoscopy quality. For that purpose valid quality indicators are necessary to be defined. The application process of some quality indicators is presented in this study. The proposed indicators in this study are: quality of bowel preparation, cecal intubation rate, withdrawal time, adenoma detection rate, and adenoma removal rate.
Material and method: this is a prospective 12-month study where colonoscopies performed in the VI health area of Murcia Region were evaluated. From February 2006 to February 2007 a total of 609 subjects were eligible for colonoscopy after a positive fecal blood test in the setting of a colorectal cancer screening program. A sample of thirty patients (n: 30) was considered representative to assess the reliability of quality indicators and for a preliminary analysis of results.
Results: indicators results are: quality of bowel preparation (87%), kappa 0.74 (95% CI: 0.48-0.99); cecal intubation rate (90%) 0.74 (95% CI: 0.49-0.99); adenoma detection and removal rate (96%), kappa: 0.78 (95% CI: 0.53-0.99); withdrawal time: 13.36 min (95% CI: 10.48-16.11). Kappa: 0.78 (95% CI: 0.49-0.99).
Conclusions: quality indicators definition and application in colonoscopy performance is possible. More studies are necessary to define the role of these indicators in the setting of clinical practice.
Key words: Quality. Quality indicators. Colonoscopy. Endoscopy.
RESUMEN
Objetivo: la colonoscopia constituye la técnica exploratoria del colon más importante en la actualidad. Su uso, cada vez más frecuente conlleva la aparición de problemas en su aplicación. Es necesario medir la calidad en la realización de esta técnica, para ello es preciso definir indicadores válidos que permitan la realización de ciclos de evaluación de la calidad. En este estudio se presenta la aplicación de algunos de estos indicadores. Los indicadores propuestos en este estudio son: nivel de limpieza, intubación cecal, indicador de pólipos y tiempo de retirada.
Pacientes y método: estudio prospectivo de 12 meses de las colonoscopias realizadas en un programa de cribado de cáncer colorrectal en el área de salud VI de la Región de Murcia. En este estudio se incluyen todos los pacientes con resultado positivo al test de sangre oculta en heces (SOH) desde febrero de 2006 a febrero de 2007 (n: 609). Se extrae una muestra de 30 pacientes para evaluar la fiabilidad de los indicadores y realizar un análisis preliminar de los resultados.
Resultados: los resultados preliminares obtenidos de cumplimiento para cada indicador fueron los siguientes: indicador de nivel de limpieza (87%). Índice de kappa 0,74 (IC del 95%: 0,48-0,99); intubación cecal (90%) 0,74 (IC del 95%: 0,49-0,99); indicador de pólipos (96%), índice de kappa de 0,78 (IC del 95%: 0,53-0,99); tiempo de retirada: 13,36 min (IC del 95%: 10,48-16,11). Índice kappa de 0,78 (IC del 95%: 0,49-0,99).
Conclusiones: la definición y aplicación de indicadores de calidad en la práctica de la colonoscopia es posible. Se precisan más estudios para definir el papel de estos indicadores en la práctica asistencial.
Palabras clave: Calidad. Indicadores de calidad. Colonoscopia. Endoscopia.
Introduction
Colonoscopy is presently the gold standard method for colonic examination. Not only is it widely accepted as a diagnostic technique but also as a procedure which enables treatment for a wide variety of conditions involving the intestinal tract. This unique feature explains why its practice is done in most hospitals of present-day healthcare systems.
Quality measurements for any process require firstly a definition of valid and reliable indicators to enable assessment (1). In recent years many attempts have been tried in order to define useful criteria for this purpose; however, its use has not been completely accepted to date by the different medical societies (2-5).
There is strong evidence that colonoscopy performance varies among different centers and endoscopists (6-12). The issue we presently face is the unavailability of adequate tools to measure these parameters.
The use of colonoscopy has proven the most effective method to reduce colorectal cancer (CRC) mortality (13-15). A wide variety of screening modalities have been developed to date, and a majority proved effective to reduce colorectal cancer incidence and mortality rates, with colonoscopy being the last resort in the screening sequence regardless of the initial screening method used (16-19).
In this study we present the application and adaptation of several parameters to a specific context in order to evaluate the quality of a screening program. This is a complicated process which requires a staff used to specific quality evaluation methods (20,21).
The following recommendations should be followed when criteria or valid indicators are elaborated as quality measurement tools (Table I).
In this study we present four indicators elaborated for the assessment of colonoscopy quality in the setting of a screening program.
Material and method
This study was performed in the setting of a CRC screening program. The aim of this study was to measure a number of quality parameters for this diagnosis confirmation stage by using some indicators (22).
The study population consisted of subjects participating in the screening program with a quantitatively positive immunochemical occult blood test (≥ 100 ng/ml) who accepted to undergo colonoscopy (609 participants) between February 2006 and February 2007. The unit of the study consisted of each participant enrolled in the program.
A number of indicators were settled upon based on the best scientific evidence available to date for quality assessment and measurement (2,3,5). The aforementioned indicators measure the magnitude of the scientific-technical quality of colonoscopy.
All participants were given detailed information about the screening process, which is registered in the clinical records of each participant. All colonoscopies performed were completely recorded and stored in a digital system. Each participant was assigned an individual number, which was used for case identification. A written informed consent was obtained from each participant to be included in an anonymous way.
The screening program was performed by two endoscopists who were specially trained to use these indicators. A pilot program was carried out in order to confirm the reliability of the proposed indicators. For this purpose a randomized sample of 30 patients was obtained to calculate a specific consistency index for each indicator. The analysis of such indicators was carried out by three endoscopists who did not participate in the screening program.
The data source for the indicators evaluating colonoscopy was the recorded examination, subsequently visualized to draw conclusions.
Indicators analyzed in this study were as follows:
-Bowel preparation quality.
-Cecal intubation rate.
-Polyp detection and resection rate.
-Colonoscope withdrawal time.
Definition of criteria
Adequate bowel preparation for colonoscopy
It is an indicator of the process and evaluates the quality of bowel cleanliness prior to colonoscopy. The colonoscope explores the tract from the anus to the cecum and the small bowel; for an optimal evaluation of the colonic mucosa, the patient must be prepared for the procedure by removing feces from the digestive tract (23,24).
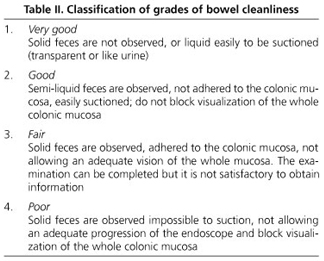
To evaluate the quality of bowel preparation during colonoscopy the following classification was used (Table II):
According to the established criteria, bowel preparation was classified as "very good" or "good" for the procedure to be considered valid and meet the criteria.
This indicator was used in all colonoscopies performed during the screening program.
Complete examination of the colon (cecal intubation)
An appropriate examination of the proximal colon or cecum with colonoscopy is essential. In daily practice a complete colonoscopy implies an intubation of the entire colon until the cecum is visible. Only the visualization of the ileocecal valve and/or intubation of the terminal ileum provides reassurance on the procedure's completeness (6,25-27). Thus, it is necessary to document the procedure in a digital source once the cecum is reached in order to confirm the fulfillment of this criterion. In procedures where the endoscope found a stenosis, this indicator was not evaluated regardless of stenosis nature.
Resected polyps and flat lesions
Every lesion detected during colonoscopy must be resected. Colonoscopy in a screening program is performed under the most suitable conditions regarding tolerance as well as preparation. Every detected lesion which can be endoscopically resected is removed. There is a strong relationship between polyp size and histological type so that any lesion with a size larger than 10 mm is considered of high risk (28-31). In recent years the neoplastic potential of lesions smaller in size has been analyzed, specially regarding flat lesions, making the resection of every visible polyp a necessary condition regardless of size (10,11). To achieve fulfillment for this indicator all visualized lesions should be endoscopically resected except certain lesions. Those lesions which endoscopically suggest a hyperplastic polyp (pale, sessile lesions that disappear after insufflation) and measure less than 3 mm in size can be biopsied with no necessity to resect all lesions to meet indicator criteria.
In cases with more than 20 polyps detected the removal of all polyps can be performed in a second examination without invalidating the established criteria. In such patients genetic susceptibility to colorectal adenomatous lesions may be suspected
In situations where the lesion cannot be removed at initial colonoscopy due to its large size, resection can be postponed. The minimal size to evaluate whether endoscopic resection is necessary in a second colonoscopy is 3 cm for polypoid lesions and 2 cm for flat lesions.
Measuring examination time during colonoscopy withdrawal
Examination time during colonoscope withdrawal is measured from the cecum to the anus. Endoscopic examination consists of the insertion of an optical system in the colon with the purpose of identifying treatable lesions (32).
Scientific evidence demonstrates that withdrawal is most suitable for the detection of lesions (33,34). Examinations where complete colonoscopy is achieved by a clear visualization of the cecum, as previously mentioned, will be evaluated.
It has been recently demonstrated that a withdrawal time superior to 6 minutes is associated with good endoscopic practice since it enables higher detection rates for colonic lesions (34,35).
If, during the examination, a specific technique different from lesion identification is performed, this time will not be considered to evaluate the indicator, and therefore will be taken from total examination time.
Statistical analysis
The statistical analysis was performed with the Epidat system (v 3.1.January 2006). Sample tests, inference over statistical parameters, and definition of confidence intervals were all performed with this program.
Results
Bowel preparation quality
A total of 30 examinations were evaluated and bowel cleanliness was classified as follows: 3 (10%) "very good", 23 (77%) "good", 4 (13%) "fair", and 0 "poor". An analysis of indicator reliability was performed, and the global kappa index (K) for all three observers was: 0.47 (95% CI: 0.24-0.70). These consistent results were related to the assessment of bowel preparation using the proposed classification. Since the kappa value was in the limit of desirable, corrective modifications were performed. When a concordance analysis was done by gathering indicators as follows: "very good" or "good" as adequate examination, and "fair" or "poor" as inadequate examination, the value of kappa was modified to 0.74 (95% CI: 0.48-0.99) (Fig. 1).
Cecal intubation
Among the evaluated sample of 30 patients, the cecum was identified in 27 patients (90%) according to the previously mentioned criteria. Of the 3 patients where the cecum could not be reached, intolerance in spite of medication was the reason in two (6%); in one, cecum was not achieved due to an anatomical feature (dolichocolon). The kappa index obtained for indicator evaluation by all three observers was 0.74 (95%CI: 0.49-0.99).
Polyp resection
Of the 30 patients evaluated, this indicator was met in 25 patients (96%). Among the remaining 5, 4 cases were considered exceptions; 3 had hyperplastic polyposis, and one case required a second colonoscopy for polypectomy of a large-size polyp (greater than 3 cm). Only one case did not meet indicator criteria. A kappa index of 0.78 (95%CI: 0.53-0.99) was obtained in the consistency analysis (Fig. 2).
Withdrawal time
The following results were obtained: nearly 97% of patients met the established criteria. Mean withdrawal time was 13.36 min (95% CI: 10.48-16.11). A reliability analysis of minimal withdrawal time measurement was performed, which obtained a kappa index of 0.78 (95% CI: 0.49-0.99) (Fig. 3).
Discussion
Quality is an essential paradigm in daily clinical activity. In recent years remarkable efforts have been made to devise tools able to establish optimal quality standards in the different processes of medical practice (2,5,18).
Gastrointestinal endoscopy has become a diagnostic-therapeutic tool essential for daily clinical practice, presently its practice being done in most hospitals of present-day healthcare systems.
This globalization has determined the present technological development, which enables us to assure there is no site in the gastrointestinal tract impossible to be explored. However, this same globalization has contributed to a certain level of heterogeneity, still to be defined, which does not allow comparisons between the different settings where it is performed (36). For this purpose it is necessary to establish resources capable of objectively assessing an activity regardless of the healthcare setting considered.
There is growing interest in the elaboration of such models, and different scientific societies have introduced their own models, adapting them to their own practical settings (2,5,18). The observed tendency with these models is a progression to simplicity, since the more complex they are, the more problematic their application becomes, with a consequent loss in efficacy.
When a model is introduced the possibility of its modification must be clearly established since one of the main features should be continuous improvement.
One of the main problems emerging when a quality model is put to the test for a certain medical practice is framework; routine medical practice frequently has difficulties when all parts making up a process need to be controlled; consequently, a low rate of implementation for such models is mostly observed. Many attempts to consolidate a proposed quality model have been made in the setting of a CRC screening program (2,5). A screening program enables the organization of such activity by settling a healthcare process; the management of each process in the entire healthcare framework generated by the screening strategy allows controlling the whole activity performed in a more adequate fashion.
Therefore, carrying out the study in the screening program enabled us to control colonoscopy practice, performed in this framework in a more simple way than in classic medical practice, and consequently allowing that the proposed model be put to the test.
The proposed process for this study has a clearly established model defined by a number of indicators whose application will enable the settling of a certain quality level and its support by monitoring techniques.
Measuring bowel cleanliness is somewhat difficult when levels have to be established. The possibility to establish levels according to the amount of clean mucosa measured in percentage seems unfeasible from a practical point of view due to the impossibility to define the different paths of the colon in absolute terms. One of the most relevant conclusions to reach from the assessment of this indicator was the necessity to group levels together in order to simplify interpretations on cleansing quality. Thus, when colonoscopy cleansing quality has to be evaluated a scale of two levels is most reliable: valid or not valid. The results presented in this study reveal that more than 90% of examinations were considered valid for bowel cleansing.
In published series of observational studies, a rate of fulfillment for this indicator above 70% represented an adequate level of cleanliness (2,3,5).
Cecal intubation implies the end of the examination, and therefore a complete colon examination is assumed. Population-based series of cecal intubation not related to screening programs report rates of 90% as their highest levels (2,37). Thus, cecum intubation rates up to 97% have been reported in the setting of a screening program (2,3,6,25). The results observed in this study (90%) were within the expected range. The two reasons for failure in achieving this indicator were patient intolerance and the presence of a specific anatomical feature (dolichocolon).
In the indicators assessed in our study, it is important to mention that to a certain extent they are indirect markers that do not directly establish whether colonoscopy was "high quality", but determine the most suitable conditions in which colonoscopy can be performed. The only result indicator that directly reflects colonoscopy quality is the one related to polyp resection and removal. This indicator summarizes in a schematic fashion how the procedure should be performed - more polyps analyzed means better visualization, hence a more thorough bowel preparation.
One of the issues or criticisms raised regarding this study is the fact that endoscopists are aware of their being observed since the entire exploration is recorded and subsequently visualized. Such effect can theoretically determine a bias that may modify study data, even though the aim of the study is the systematization of how colonoscopy should be performed. In this first instance, the purpose is not an evaluation of the endoscopist's skills but to assess whether we can define and put into practice some valid indicators to evaluate a certain manner of colonoscopy performance. This bias could become beneficial subsequently in a positive way. More studies are necessary to clarify which are the most reliable indicators to measure colonoscopy quality. Once the validity of these indicators is defined and demonstrated, they will be used in the setting of a screening program in order to evaluate the required quality parameters.
The efficacy of CRC screening programs depends on several factors; high-quality colonoscopic examinations are desirable to facilitate success for such programs (38).
References
1. Características de los indicadores clínicos. Joint Commission on Accreditation of Healthcare Organizations. Control de Calidad Asistencial 1991; 6(3): 65-74. [ Links ]
2. Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2006; 63(4 Supl.): S16-28. [ Links ]
3. Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on colorectal cancer. Am J Gastroenterol 2002; 97: 1296-308. [ Links ]
4. Lieberman D. Quality and colonoscopy: a new imperative. Gastrointest Endosc 2005; 61: 392-4. [ Links ]
5. Faigel DO, Pike IM, Baron TH, Chak A, Cohen J, Deal SE, et al; ASGE/ACG Taskforce on Quality in Endoscopy. Quality indicators for gastrointestinal endoscopic procedures: an introduction. Am J Gastroenterol 2006; 101: 866-72. [ Links ]
6. Bowles CJA, Leicester R, Romaya C, Swarbrick E, Williams CB, Epstein O. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut 2004; 53: 277-83. [ Links ]
7. Levin TR, Farraye FA, Schoen RE, Hoff G, Atkin W, Bond JH, et al. Quality in the technical performance of screening flexible sigmoidoscopy: recommendations of an international multi-society task group. Gut 2005; 54: 807-13. [ Links ]
8. Atkin W, Rogers P, Cardwell C, et al. Wide variation in adenoma detection rates at screening flexible sigmoidoscopy. Gastroenterology 2004; 126: 1247-56. [ Links ]
9. Schoen RE, Pinsky PF, Weissfeld JL, et al. Results of repeat sigmoidoscopy 3 years after a negative examination. JAMA 2003; 290: 41-8. [ Links ]
10. Rex DK, Cutler CS, Lemmel GT, et al. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology 1997; 112: 24-8. [ Links ]
11. Pickhardt PJ, Nugent PA, Mysliwiec PA, et al. Location of adenomas missed by optical colonoscopy. Ann Intern Med 2004; 141: 352-9. [ Links ]
12. Bressler B, Paszat LF, Vinden C, et al. Colonoscopic miss rates for right-sided colon cancer: a population-based analysis. Gastroenterology 2004; 127: 452-6. [ Links ]
13. Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med 1993; 328: 1365-71. [ Links ]
14. Ransohoff DF. Colon cancer screening in 2005: status and challenges. Gastroenterology 2005; 128: 1685-95. [ Links ]
15. Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Results of screening colonoscopy among persons 40 to 49 years of age. N Engl J Med 2002; 346: 1781-5. [ Links ]
16. Mandel JS, Church TR, Bond JH, Ederer F, Geisser MS, Mongin SJ, et al. The effect of fecal occult-blood screening on the incidence of colorrectal cancer. N Engl J Med 2000; 343: 1603-7. [ Links ]
17. Castells A, Marzo M, Bellas B, Amador FJ, Lanas A, Mascort JJ, et al. Clinical guidelines for the prevention of colorectal cancer. Gastroenterol Hepatol 2004; 27: 573-634. [ Links ]
18. Rex DK, ACG Board of Trustees. American College of Gastroenterology action plan for colorectal cancer prevention. Am J Gastroenterol 2004; 99: 574-7. [ Links ]
19. Jorgensen OD, Kronborg O, Fenger C. A randomised study of screening for colorectal cancer using faecal occult blood testing: results after 13 years and seven biennial screening rounds. Gut 2002; 50: 29-32. [ Links ]
20. Saturno PJ. Evaluación y Mejora de la Calidad en Servicios de Salud. Conceptos y Métodos. Murcia: Consejería de Sanidad y Consumo de la Región de Murcia; 2000. [ Links ]
21. Saturno PJ, Quintana O, Varo J. ¿Qué es calidad? En: Tratado de Calidad Asistencial en Atención Primaria. Madrid: Dupont Pharma; 1997. p. 17-45. [ Links ]
22. Plan de Salud 2003-2007. Región de Murcia. Consejería de Sanidad de la Comunidad Autónoma de la Región de Murcia; 2003. [ Links ]
23. Harewood Gc, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc 2003; 58: 76-9. [ Links ]
24. Froelich F, Wietlisbach V, Gonvers JJ, et al. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European Multicenter Study. Gastrointest Endosc 2005; 61: 378-84. [ Links ]
25. Marshall JB, Barthel JS. The frequency of total colonoscopy and terminal ileal intubation in the 1990s. Gastrointest Endosc 1993; 39: 518-20. [ Links ]
26. Rex DK. Still photography versus videotaping for documentation of cecal intubation: a prospective study. Gastrointest Endosc 2000; 51: 451-9. [ Links ]
27. Lieberman DA, Weiss DG, Bond JH, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med 2000; 343: 162-8. [ Links ]
28. Pabby A, Schoen RE, Weissfeld JL, et al. Analysis of colorectal cancer occurrence during surveillance colonoscopy in the dietary Polyp Prevention Trial. Gastrointest Endosc 2005; 61: 385-91. [ Links ]
29. Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med 1993; 329: 1977-81. [ Links ]
30. Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, et al.; Gastrointestinal Consortium Panel. Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology 2003; 124: 544-60. [ Links ]
31. Citarda F, Tomaselli G, Capocaccia R, et al. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut 2001; 48: 812-5. [ Links ]
32. Williams C. Insertion technique. In: Waye J, Rex D, Williams C, editors. Colonoscopy: principles and practice. Oxford: Blackwell Publishing; 2003. p. 318-38. [ Links ]
33. Barclay R, Vicari JJ, Johanson JF, et al. Variation in adenoma detection rates and colonoscopic withdrawal times during screening colonoscopy (abstract). Gastrointest Endosc 2005; 61: AB107. [ Links ]
34. Rex DK. Colonoscopic withdrawal technique is associated with adenoma miss rates. Gastrointest Endosc 2001; 51: 33-6. [ Links ]
35. Simmons DT, Harewood GC, Baron TH, Petersen BT, Wang KK, Boyd-Enders F, et al. Impact of endoscopist withdrawal speed on polyp yield: implications for optimal colonoscopy withdrawal time. Aliment Pharmacol Ther 2006; 24: 965-71. [ Links ]
36. Lieberman D. Quality and colonoscopy: a new imperative. Gastrointest Endosc 2005; 61: 392-4. [ Links ]
37. Rex DK. Quality in colonoscopy: cecal intubation first, then what? Am J Gastroenterol 2006; 101: 732-4. [ Links ]
38. Navarro M, Peris M, Binefa G, Nogueira JM, Miquel JM, Espinás JA, Catalan Colorectal Cancer Screening Pilot Programme Group. Colonoscopic findings from a pilot screening study for colorectal cancer in Catalonia. Rev Esp Enferm Dig 2008; 100: 343-8. [ Links ]
![]() Correspondence:
Correspondence:
Senador Morán Sánchez.
Sección de Digestivo.
Hospital Santa María del Rosell.
Paseo Alfonso XIII, 61.
30203 Cartagena, Murcia, spain.
e-mail: senadormoran@yahoo.es
Received: 01-07-08.
Accepted: 15-01-09.











 text in
text in