My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 n.8 Madrid Aug. 2012
https://dx.doi.org/10.4321/S1130-01082012000800008
PICTURES IN DIGESTIVE PATHOLOGY
Giant splenomegaly and non-Hodking's lymphoma
Esplenomegalia gigante y linfoma no Hodgkin
Luis Erik Álvarez-Burneo, Luis Kerlin Mercedes and Armando Arce-Álvarez
Department of General Surgery. Hospital Virgen de la Luz. Cuenca, Spain
Case report
A 35-year-old male presented to our clinic with asthenia, hyporexia, and weight loss (3 kg in two months) of one month duration. Physical examination was positive for an abdominal mass that occupied left side of abdomen, right iliac fossa and flank consistent with splenomegaly. Blood tests showed moderated anemia (Hb: 10 g/dL) and hypercalcemia (Ca: 13.1 mg/dL). Chest/abdominal CT scan revealed splenomegaly of 27 cm major axis with multiple hypodense areas and hiliar splenic adenopathies about 17-28 cm size (Fig. 1). Presumptive diagnosis of lymphoma was established and diagnostic/therapeutic splenectomy was scheduled.
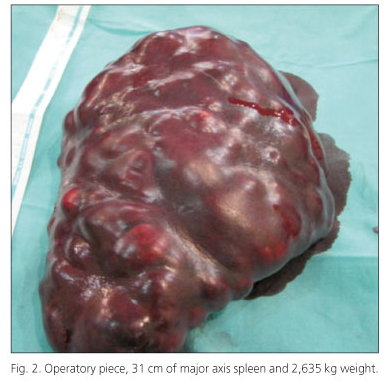
Splenic resection was performed without complication via a subcostal laparotomy using an "in situ" technique (Fig. 2). Pathology returned as a diffuse large B-cell lymphoma and the patient was started on combined chemotherapy treatment (CHOP and rituximab).
Discussion
Diffuse large B-cell lymphoma is the most frequent variety of non-Hodgkin's lymphoma, representing approximately 33% of all cases (1). Presumptive diagnosis of lymphoma is based on clinical presentation, blood tests, and imaging. Splenectomy is necessary for a definitive anatomopathological diagnosis (1,2) in addition to being therapeutic (solves problems related with splenomegaly and hypersplenism) (3,4). After splenectomy blood counts return to normal values, transfusional requirements are reduced, and subsequent chemotherapy tolerance is improved (1,3,4).
Surgical approach using "in situ" technique is recommended for this kind of surgery (giant spleen and programmed surgery) (5).
References
1. Le Gouill S. Mantle cell lymphoma: an overview from diagnosis to future therapies. La Revue de Médecine Interne 2010;31:615-20. [ Links ]
2. Iriyama N, Horikoshi A, Hatta Y, Kobayashi Y, Sawada S, Takeuchi J. Localized, splenic, diffuse large B-cell lymphoma presenting with hypersplenism: risk and benefit of splenectomy. Internal Medicine 2010;49:1027-30. [ Links ]
3. Pottakkat B, Kashyap R, Kumar A, Sikora S , Saxena R, Kapoor V. Redefining the role of splenectomy in patients with idiopathic splenomegaly. ANZ Journal of Surgery 2006;76:679-82. [ Links ]
4. Carr JA, Shuarafa M, Velanovich V. Surgical indications in idiopathic splenomegaly. Archives of Surgery 2002;137:64-8. [ Links ]
5. Breil P. Splénectomie. Techniques chirurgicales- Appareil Digestif. Encycl Méd Chir. Paris-France: Elsevier; 1997.p. 40-750, 10 p. [ Links ]











 text in
text in