My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.4 Madrid Apr. 2014
PICTURES IN DIGESTIVE PATHOLOGY
Anorectal melanoma associated with colonic metastasis
Melanoma anorrectal asociado a metástasis colónicas
Macarena Fernández-Albornoz, Joaquín Irarrázaval-Espinoza, Andrés Larach-Kattan and Leonardo Espíndola-Silva
Hospital Militar. Santiago, Chile
Case report
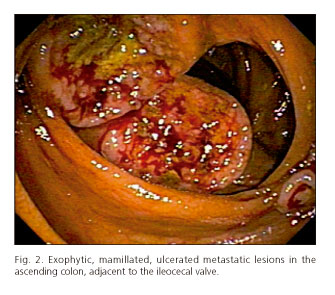
A 67-year-old female patient with no medical history presents with pain and increased volume in her right lower limb for the last three weeks. She is admitted with a diagnosis of right-side iliac-femoral-popliteal deep venous thrombosis and bilateral pulmonary thromboembolism. She developed rectorrhagia following anticoagulation. Colonoscopy revealed an exophytic, mamillated, friable, anteriorly ulcerated lesion from the anal margin to the mid rectum (Fig. 1), two lesions with similar characteristics in the ascending colon, and three such lesions at the ileocecal valve (Fig. 2). Histopathology and immunohistochemical studies are consistent with melanoma. Abdominal and pelvic CT and MRI scans show a solidly thickened wall with lumpy contours, heterogeneous structure, and poorly delimited borders in the mid and lower rectum, cecum, and ascending colon. She also has neoplastic-looking adenopathies in the right external iliac chain, right hypogastric chain, and aortic bifurcation. The patient received symptomatic palliative care.
Discussion
Anorectal melanoma represents 0.1 %-4.6 % (3) of anorectal neoplasms, and less than 2 % of all melanomas, with a median survival below 20 months (1). Lower gastrointestinal bleeding is the most common clinical manifestation (55 %) (4). A differential diagnosis with other colorectal neoplasms is difficult to establish with only colonoscopy, hence histological and immunohistochemical confirmation (positivity for HMB-45 and protein S-100) is essential (2). At the time of diagnosis, over 30 % of subjects have distant metastases on CT or MRI images (4). Colonic melanoma metastases represent 22-28 % of all gastrointestinal metastases (3). Surgical resection is used for localized cases; however, survival is related to metastasis development rather than local disease control. The role of chemotherapy is uncertain and radiation therapy is useful for palliation (2,4).
References
1. Stefanou A and Nalamati S. Anorectal Melanoma. Clin Colon Rectal Surg 2011;24:171-6. [ Links ]
2. Meguerditchian A, Meterissian S, Bullard Dunn K. Anorectal melanoma: Diagnosis and treatment. Dis Colon Rectum 2011;54:638-44. [ Links ]
3. Díaz-Sánchez A, Lara MA, Ortega P, Aramendi T, González C, Alberdi JM, et al. Melanoma colorrectal: revisión de dos formas diferentes de presentación. Gastroenterol Hepatol 2011;34:83-8. [ Links ]
4. Heeney A, Mulsow J, Hyland J. Treatment and outcomes of anorectal melanoma. The Surgeon 2011;9:27-32. [ Links ]











 text in
text in