My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 n.5 Madrid May. 2015
PICTURES IN DIGESTIVE PATHOLOGY
Endoscopic radiofrequency ablation for APC refractory gastric antral vascular ectasia using the HALO90 system in a kidney transplant candidate
Gemma Ibáñez-Sanz1, Laura Rivas1, Eduardo Melilli2, Jordi Guardiola3, Carme Baliellas4 and Joan B. Gornals1
1Endoscopy Unit, Department of Digestive Diseases.
2Department of Nephrology.
3Gastroenterology Unit, Department of Digestive Diseases.
4Hepatology Unit, Department of Digestive Diseases. Hospital Universitari de Bellvitge-IDIBELL. Barcelona, Spain
Introduction
Gastric antral vascular ectasia (GAVE) is a rare but important cause of gastrointestinal bleeding and anemia. Endoscopic ablation, such as argon plasma coagulation (APC), is usually successful, but treatment-refractory cases do occur (1). Recently, radiofrequency ablation (RFA) has been described as an alternative therapeutic option for GAVE, or actinic proctitis, with positive results and minor complications (2-5).
Case report
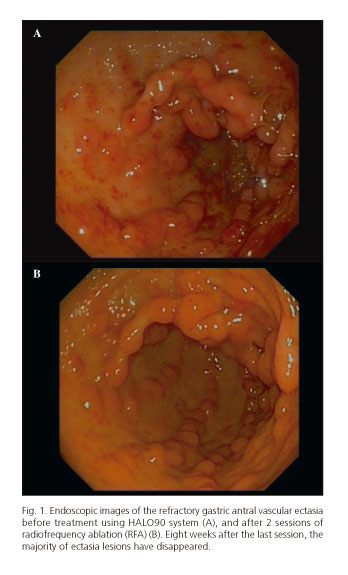
A 60-year-old man with chronic renal failure in hemodialysis, liver cirrhosis, and chronic iron-deficiency anemia (hemoglobin 7.5 g/dL) with transfusion requirements. GAVE was diagnosed after upper endoscopy, without evidence of portal hypertensive gastropathy (Fig. 1A). In the preceding four years his transfusion requirements had increased (2 packed-red-cells monthly) although he underwent 17 APC sessions. An endoscopic ablation of antral lesions with RFA was considered.
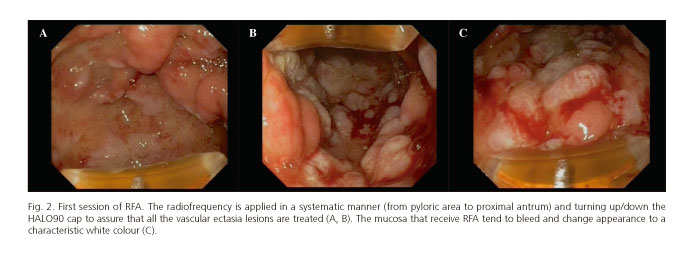
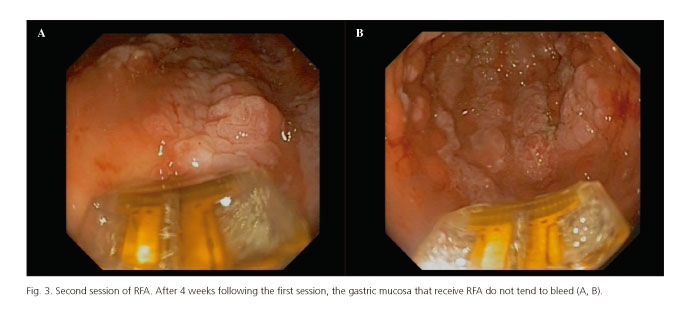
The radiofrequency device was inserted at the gastroscope end. The vascular antral anomalies were treated using the HALO90 system (BARRX Medical, Sunnyvale, CA). In the first session, GAVE lesions received 31 ablations (at 12 Joules/cm2/40 watts), twice per area, with direct and retroverted view (Fig. 2 A-C) for 29 minutes with good patient tolerance. A second session was scheduled at 4 weeks, and 68 ablations were applied for 36 minutes (Fig. 3 A and B). No complications were reported in either session.
Three months later, the majority of antral lesions had disappeared (Fig. 1B). Hemoglobin increased to 12 g/dL without any further transfusion requirement, and the patient could be included in a kidney transplant waiting list.
Discussion
RFA is popular in the context of Barrett's esophagus dysplasia treatment. Only four published case series have reported the utility of RFA in GAVE lesions (2,3).
This clinical case suggests that RFA using the HALO90 system is a real and safe option for chronic bleeding related to refractory GAVE after attempted APC in patients with chronic renal failure and awaiting kidney transplantation.
References
1. Patwardhan VR, Cardenas A. Review article: The management of portal hypertensive gastropathy and gastric antral vascular ectasia in cirrhosis. Aliment Pharmacol Ther 2014 Jun 2. doi: 10.1111/apt.12824. [ Links ]
2. Gross SA, Al-Haddad M, Gill KR, et al. Endoscopic mucosal ablation for the treatment of gastric antral vascular ectasia with the HALO90 system: A pilot study. Gastrointest Endosc 2008;67:324-7. [ Links ]
3. McGorisk T, Krishnan K, Keefer L, et al. Radiofrequency ablation for refractory gastric antral vascular ectasia (with video). Gastrointest Endosc 2013;78:584-8. [ Links ]
4. Díez-Redondo P, de-la-Serna C, Vallecillo MA, Núñez H, Gil-Simón P, Pérez-Miranda M. Radiofrequency ablation: A novel and effective treatment of severe bleeding secondary to actinic proctitis. Rev Esp Enferm Dig 2013;9:555-6. [ Links ]
5. Gutkin E, Schnall A. Gastroesophageal junction tear from HALO 90 System: A case report. World J Gastrointest Endosc 2011;3:105-6. [ Links ]