My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.5 Madrid May. 2016
Enhanced flat adenoma detection rate with high definition colonoscopy plus i-scan for average-risk colorectal cancer screening
Antonio Rodríguez-D'Jesús and Esteban Saperas
Gastroenterology Department. Hospital General de Catalunya. Sant Cugat del Valles, Barcelona. Spain
ABSTRACT
Background and aim: The usefulness of high definition colonoscopy plus i-scan (HD+i-SCAN) for average-risk colorectal cancer screening has not been fully assessed. The detection rate of adenomas and other measurements such as the number of adenomas per colonoscopy and the flat adenoma detection rate have been recognized as markers of colonoscopy quality. The aim of the present study was to compare the diagnostic performance of an HD+i-SCAN with that of standard resolution white-light colonoscope.
Methods: This is a retrospective analysis of a prospectively collected screening colonoscopy database. A comparative analysis of the diagnostic yield of an HD+i-SCAN or standard resolution colonoscopy for average-risk colorectal screening was conducted.
Results: During the period of study, 155/163 (95.1%) patients met the inclusion criteria. The mean age was 56.9 years. Sixty of 155 (39%) colonoscopies were performed using a HD+i-SCAN. Adenoma-detection-rates during the withdrawal of the standard resolution versus HD+i-SCAN colonoscopies were 29.5% and 30% (p = n.s.). Adenoma/colonoscopy values for standard resolution versus HD+i-SCAN colonoscopies were 0.46 (SD = 0.9) and 0.72 (SD = 1.3) (p = n.s.). A greater number of flat adenomas were detected in the HD+i-SCAN group (6/60 vs. 2/95) (p < .05). Likewise, serrated adenomas/polyps per colonoscopy were also higher in the HD+i-SCAN group.
Conclusions: A HD+i-SCAN colonoscopy increases the flat adenoma detection rate and serrated adenomas/polyps per colonoscopy compared to a standard colonoscopy in average-risk screening population. HD+i-SCAN is a simple, available procedure that can be helpful, even for experienced providers. The performance of HD+i-SCAN and substantial prevalence of flat lesions in our average-risk screening cohort support its usefulness in improving the efficacy of screening colonoscopies.
Key words: Serrated adenomas. i-Scan. Adenoma detection rate. Average-risk. Screening. Colonoscopy.
Introduction
A high-quality colonoscopy that ensures the detection and removal of all neoplastic lesions is key for the efficacy of screening and surveillance of colorectal cancer (CRC) (1,2). Unfortunately, up to 20% of all neoplastic lesions, especially small and flat lesions, are still missed during a colonoscopy (3-5). This unsatisfactorily high overall miss rate remains a concern and is one of the key factors in the development of interval cancer (6). Many common reasons for missing lesions are related to a number of elements of procedural quality such as bowel preparation (7,8), but they also partly result from the highly operator-dependent nature of the procedure (9). In fact, the quality of a colonoscopy as measured by the adenoma detection rate (ADR), which is an independent predictor of the risk of interval cancer, varies widely among physicians (9-12). Detection of flat, subtle lesions in the colon, including serrated adenomas/polyps, remains a challenge depending on a careful operator technique. Appropriate endoscopist performance characteristics with meticulous inspection and an adequate withdrawal time increase colonoscopy yield, reducing the substantial miss rate reported with standard resolution white light colonoscopies (SRWL) (13,14).
However, missing non-polypoid or flat lesions that often evade detection with SRWL might be a factor for colonoscopy failure as well (15). Importantly, these flat adenomas may carry a higher risk of developing into CRCs than polypoid adenomas (5,16,17).
During the last two decades, a number of advances have been made to overcome the limitations of standard white light and traditional forward-viewing angle colonoscopies in recognizing flat lesions. Among these advances, the higher resolution provided by high definition (HD) scopes coupled with chromoscopy provides a more detailed imaging of the colonic mucosa and might improve the detection of these subtle lesions that would otherwise be overlooked by an SRWL colonoscopy. However, despite these potential benefits, this technique has shown a moderate gain (18,19), and its role in average-risk patients undergoing routine screening has not been fully established. The HD+i-SCAN (Pentax, Japan) method is a post processing image technique that enhances the contrast of the image using computerized spectral estimation technology that selects specific light wavelengths. The HD+i-SCAN technique has not been as widely implemented as narrow band imaging, and less evidence is available for evaluation of this application of the technique.
The aim of the present study was to determine whether the use of a HD+i-SCAN colonoscopy improves diagnostic performance of a colonoscopy compared to the use of a SRWL colonoscopy with respect to ADR, adenoma per colonoscopy (APC) and flat ADR (FADR) in an average risk population undergoing a comprehensive CRC screening colonoscopy.
Methods
This is a retrospective analysis of a prospectively collected screening colonoscopy database.
The data from consecutive asymptomatic outpatients without any familial CRC background who were 50 years of age or older and undergoing their first CRC screening colonoscopy in the Hospital General de Catalunya were analyzed. A comparative performance analysis of HD+i-SCAN (90i series, Pentax, Tokyo, Japan) versus SRWL (EC-3870FZK, Pentax) colonoscopies was performed. Assignment to conventional endoscopy or HD+i-SCAN was determined only by the availability of high-definition or conventional endoscope at the time of exploration.
Only patients with excellent or good preparations and cecal intubation were included. All comprehensive standardized colonoscopies were performed by two experienced endoscopists (A.R.; E.S). Withdrawal times were targeted to exceed at least 6 minutes in all colonoscopies. All withdrawal times were recorded and they were defined as the amount of time spent examining the colon (without taking into account polypectomy or biopsy times) during withdrawal of the colonoscope. Time recording began after cecal intubation ("time Zero"). Cecal intubation was defined as the ability to touch the cecal pole with the tip of the colonoscope.
Patients were excluded if they had previous surgery of the colon, known inflammatory bowel disease, acute gastrointestinal bleeding, a genetic-associated colon cancer risk or impaired coagulation parameters (international normalized ratio [INR] > 1.74, partial thromboplastin time [PTT] > 50 seconds).
Prior to colonoscopy, patients were prepared using one of two standard preparations: MoviPrep (polyethylene glycol 3,350 and additives) (Norgine de España, S.L.U. Madrid, Spain) or two sachets of Citrafleet (sodium picosulfate) (Casen Recordati, S.L., Zaragoza, Spain). All patients received written instructions for the colonoscopy preparation method used. All colonoscopy procedures were performed under deep sedation with propofol, which was administered by the assistant or attending anesthetist.
The preparation grade was measured by the previously validated Aronchick scale (i.e., excellent, good, fair, poor, and unsatisfactory) (20).
A detailed examination of the colon was started when the cecum was reached, and the surface enhancement function was activated throughout the withdrawal of the instrument. The i-scan mode has been previously described elsewhere (21). Physicians were allowed to switch between HD imaging alone and the i-scan mode as pleased. Identified lesions in the HD+i-SCAN group were further characterized using the p- and v- modes (21).
Detected colorectal lesions were characterized according to the Paris Classification system (22). Resections were performed on all identified lesions. Location, size and pathology results were recorded. The term "flat adenoma" was only used if the adenoma lesion was either slightly elevated (0-IIa) or completely flat (0-IIb) (absolutely depressed lesions were not included in this definition) compared to the adjacent mucosa.
The data were classified according to numbers of polyps and adenomas, adenomas proximal to the splenic flexure (proximal adenomas), and advanced adenomas (i.e., > 1 cm in size, villous, or containing high-grade dysplasia or cancer). Detection rates were calculated for polyps (PDR), adenomas (ADR), flat adenomas (FADR) and proximal adenomas (PADR). Additionally, the number of adenomas (APC) and serrated adenomas (SAPC) per colonoscopy were also calculated.
As a retrospective evaluation, this study did not require ethics committee approval.
Statistical analysis
Continuous variables were expressed as the mean and standard deviation (SD). Categorical variables were summarized as frequency and percentage. The 95% confidence interval (CI) was calculated using the standard formula. Predictive factors for the detection rates were analyzed by univariate analysis using a Chi-square test for categorical variables and a t-test for continuous variables. A p va-lue less than 0.05 was considered to be statistically significant. All calculations were performed using SPSS statistical software version 20.0 (IBM SPSS INC, Chicago).
Results
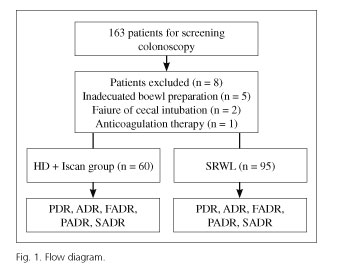
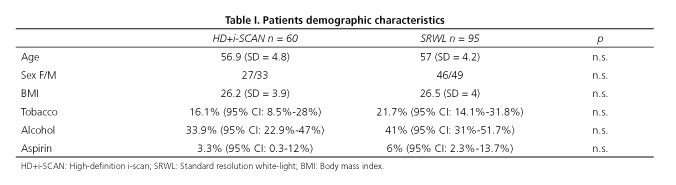
From January 2013 to March 2015, 163 consecutive screening colonoscopies were performed in the general population; 155 (95.1%) patients met the inclusion criteria (Fig. 1). Sixty of 155 (39%) colonoscopies were performed using a HD+i-SCAN colonoscope, and the remaining 95 (61%) were performed using a SRWL colonoscope. Both groups were similar in terms of age (56.9 and 57 years old in the HD+i-SCAN group and SRWL group, respectively), gender (41.5% and 48.4% males ratio, respectively, for each group), BMI, alcohol use, aspirin use and cigarette use (Table I). Both endoscopists used both types of colonoscopes, and no significant differences were found between the performances of the two endoscopists. Withdrawal times for both groups were also similar (HD+i-SCAN = 8.8 min vs. SRWL group = 8.4)
The overall number of lesions revealed was 230, with a total of 88 adenomatous polyps in 155 patients. The global ADRs were 36.6% for male patients (95% CI: 27%-47.4%) and 21.9% for female patients (95% CI: 13.9-32.8%) (p < .05).
The APC values were 0.7 (SD = 1.2) for male patients and 0.4 (SD = 1) for female patients (p = n.s.). The mean size of adenomatous polyps was 4.2 mm (SD = 3.2) (3.9 mm [range: 1-6 mm] for the SRWL group and 4.6 mm [range: 2-10mm] for HD+i-SCAN).
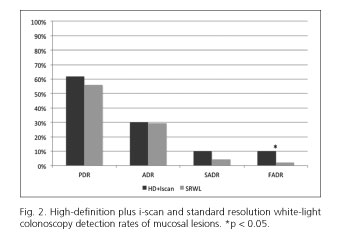
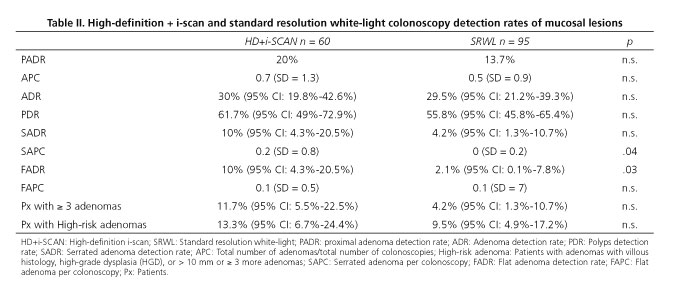
There were no significant differences between ADR or APC for procedures performed with the HD+i-SCAN and SRWL colonoscopes (Fig. 2).
FADR was significantly higher in the HD+i-SCAN group (10%, 95% CI: 4.3%-20.5%) than in the SRWL group (2.1%, 95% CI: 0.1-7.8%) (p = 0.03), with most lesions found in the right colon. Likewise, SAPC was also higher in the HD+i-SCAN group (0.2 [SD = 0.8] vs. 0 [SD = 2]) (p < .05).
A larger proportion of patients were found to have at least three adenomas in the HD+i-SCAN group than in the SRWL group (11.6% vs. 4.4%), although this difference did not reach statistical significance.
Discussion
The usefulness of an HD+i-SCAN colonoscope for screening colonoscopies remains controversial. Our study found that the HD+i-SCAN revealed more non-polypoid adenomas than the SRWL in a series of 155 consecutive average-risk patients undergoing a screening colonoscopy. FADR was significantly higher with the HD+i-SCAN colonoscope than with the SRWL colonoscope, whereas there was no significant difference between the overall ADR detected by both imaging techniques. Although our findings should be interpreted cautiously, our results provide evidence that the higher resolution and surface mucosal contrast provided by HD+i-SCAN helped endoscopists to detect subtle lesions that might not have been detected by an SRWL endoscope. The lack of difference regarding ADR between the two colonoscopes is likely explained, at least in part, by the fact that the HD+i-SCAN colonoscope is not expected to improve the detection of polypoid lesions that can be easily identified without enhanced resolution and contrast. It is also possible that the good ADR for all adenomas in our "control" SRWL group as a consequence of the excellent bowel preparation and comprehensive examination might have limited any additional improvement in the yield with the use of the HD+i-SCAN method. Finally, the relatively small number of procedures used to determine the ADR might not have been sufficient to ascertain statistical significance.
ADR is an accepted surrogate marker for the quality of a screening colonoscopy. However, measurement of ADR alone might not reliably assess the quality of a colonoscopy because it does not take into account other important determinants of interval cancer risk such as size, location or pathology of the removed lesions. It is possible that other indicators such as FADR, PADR, APC or advanced adenoma detection rate together with ADR could be a better method to determine the quality of the endoscopist performance in a screening colonoscopy (11,23,24).
Our results can be compared with those of previous randomized controlled trials that have compared chromoscopy with a SRWL colonoscope in terms of detection of colorectal adenomas. Our findings are fully consistent with those of Le Rhun et al. (25), who found that although a high-definition colonoscopy with chromoscopy (indigo) increased the detection of flat adenomas compared to a standard definition colonoscopy, the overall ADR was not significantly improved in a population at increased risk for colonic neoplasia. In contrast, a Cochrane database systematic review reports that chromoscopy with indigo carmine is likely to yield significantly more patients with at least one neoplastic lesion (OR 1.67 [CI 1.29-2.15]) and significantly more patients with three or more neoplastic lesions (OR 2.5 [CI 1.5-4.4]) (26). However, it is important to quote that, currently, digital chromoendoscopy (such as i-SCAN, NBI and FICE) has not shown in any metaanalysis to be superior to SRWL for detection of adenomas, so both techniques (digital chromoendoscopy vs. dye chromoendoscopy) could have different detection yield.
Our finding that HD+i-SCAN technology identified more flat polyps than the SRWL technique is consistent with those of one previous prospective randomized controlled trial (21) and that of one retrospective study of a large cohort of consecutive outpatients undergoing screening, diagnostic and surveillance colonoscopies (27). Recently, Kim et al. have published similar results in a comparative study exclusively in average risk patients for CRC as in our study (28).
Our study differs from these reports in several important aspects. In contrast to previous studies, we excluded the influence of bowel preparation and patients' baseline characteristics and compared the efficacy of HD+i-SCAN with that of SRWL colonoscopies according to lesion size, location and histology.
Our study has several strengths. First, the study was performed on a highly selected group of asymptomatic average-risk patients undergoing their first screening colonoscopy using current clinical practices. The distribution of gender, smoking or alcohol habits, and aspirin use was similar in both groups. Second, all patients were examined under optimal comprehensive conditions. All procedures were performed by experienced endoscopists, and comprehensive technique with a standardized withdrawal time was used. Only patients with excellent or good bowel preparations using a split dose bowel preparation and those in which the cecum was intubated and the entire length of the colon was screened were included. We standardized examination times to exceed at least 6 minutes in all colonoscopies, which minimized the impact of detection bias because a longer examination time would lead to a higher ADR.
Third, our ADRs were higher than those of previous studies and surpassed the proposed US Multi-Society Task Force on Colorectal Cancer threshold targets for populations undergoing a screening colonoscopy (29). Additionally, the ADR of each participating endoscopist was similar; therefore, data could be compared as a whole. Our study also analyzed the flat ADR, APC, and PADR, which have not been reported in other previous studies.
Our study has several limitations that should be addressed. First, it is a retrospective, not randomized, single-center study. Second, it involved a small number of experienced endoscopists and might therefore not reflect the true diagnostic yield when performed in the conditions of routine practice. In addition, endoscopists could not be blinded to the techniques being used, which may have induced an unintentional bias towards one of the two techniques. However, the fact that the HD+i-SCAN colonoscope revealed more flat ADRs than the SRWL endoscope using a comparable colonoscopy technique and withdrawal time suggests that the increased diagnostic yield is, in fact, a result of technical improvement. Although there is some evidence suggesting that both HD and i-scan contribute to improved adenoma detection, the design of our study does not allow delineating the relative benefit provided by each one of the image enhancing components of the HD+i-SCAN system.
Finally, it is also important to note that, according to most current guidelines, with the use of an HD+i-SCAN colonoscope, in our study, a higher proportion of patients (although not statistically significant) would be classified as having high-risk-adenoma, in which the recommended post-polypectomy surveillance interval for an effective prevention of CRC is shortened to 3 years (30,31) (Table II and Fig. 2).
Lesions can also evade detection due to their location on the proximal hidden side of the haustral folds and flexures. It has been estimated that 10% of the colonic surface remains unobserved by the standard forward-viewing colonoscope even with a good bowel preparation. This is due to the limitation of the torquing and turning capabilities of the flexible bending portion of standard colonoscopes. We assume that the HD+i-SCAN colonoscope will not help to inspect the blind mucosa and therefore will not have any impact on the detection of missed lesions on the reverse side of the mucosal folds. Other recently developed ancillary techniques that may assist in detecting hidden lesions in the blind mucosal surface, such as cap-assisted, Endocuff, EndoRing, and balloon colonoscopies, work on the principle of flattening the haustral folds during withdrawal and, therefore, expanding the surface area of the colonic mucosa being visualized; the Third Eye Retroscope retrograde-viewing auxiliary device, or wider angle colonoscopes can be useful adjuncts (32-36).
In conclusion, our study found that the use of a HD+i-SCAN colonoscope yielded an increase in flat ADR compared to a SRWL colonoscope in average-risk CRC screening colonoscopies. HD+i-SCAN is a simple, quick and widely available technique that can be helpful, even for experienced providers, in detecting more subtle lesions in the right-side colon. The performance of HD+i-SCAN and the substantial prevalence of flat lesions in our average-risk screening cohort support its usefulness in improving efficacy of screening colonoscopies.
References
1. Zauber AG, Winawer SJ, O Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687-96. DOI: 10.1056/NEJMoa1100370. [ Links ]
2. Leaper M, Johnston MJ, Barclay M, et al. Reasons for failure to diagnose colorectal carcinoma at colonoscopy. Endoscopy 2004;36:499-503. DOI: 10.1055/s-2004-814399. [ Links ]
3. Van Rijn JC, Reitsma JB, Stoker J, et al. Polyp miss rate determined by tandem colonoscopy: A systematic review. Am J Gastroenterol 2006;101:343-50. DOI: 10.1111/j.1572-0241.2006.00390.x. [ Links ]
4. Xiang L, Zhan Q, Zhao XH, et al. Risk factors associated with missed colorectal flat adenoma: A multicenter retrospective tandem colonoscopy study. World J Gastroenterol 2014;20:10927-37. DOI: 10.3748/wjg.v20.i31.10927. [ Links ]
5. Hart AR, Kudo S, Mackay EH, et al. Flat adenomas exist in asymptomatic people: Important implications for colorectal cancer screening programmes. Gut 1998;43:229-31. DOI: 10.1136/gut.43.2.229. [ Links ]
6. Le Clercq CM, Bouwens MW, Rondagh EJ, et al. Postcolonoscopy colorectal cancers are preventable: A population-based study. Gut 2014;63:957-63. DOI: 10.1136/gutjnl-2013-304880. [ Links ]
7. Lebwohl B, Kastrinos F, Glick M, et al. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc 2011;73:1207-14. DOI: 10.1016/j.gie.2011.01.051. [ Links ]
8. Chokshi RV, Hovis CE, Hollander T, et al. Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest Endosc 2012;75:1197-203. DOI: 10.1016/j.gie.2012.01.005. [ Links ]
9. Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 2010;362:1795-803. DOI: 10.1056/NEJMoa0907667. [ Links ]
10. Robertson DJ, Lieberman DA, Winawer SJ, et al. Colorectal cancers soon after colonoscopy: A pooled multicohort analysis. Gut 2014;63:949-56. DOI: 10.1136/gutjnl-2012-303796. [ Links ]
11. Saini SD, Schoenfeld PS, Vijan S. Can the adenoma detection rate reliably identify low-performing endoscopists? Results of a modeling study. Dig Dis Sci 2013;58:1856-62. DOI: 10.1007/s10620-013-2592-2. [ Links ]
12. Atia MA, Patel NC, Ratuapli SK, et al. Nonneoplastic polypectomy during screening colonoscopy: The impact on polyp detection rate, adenoma detection rate, and overall cost. Gastrointest Endosc 2015;82:370-5. DOI: 10.1016/j.gie.2015.01.016. [ Links ]
13. Abu Dayyeh BK, Thosani N, Konda V, et al. ASGE Technology Committee systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc 2015;81:502.e1-16. DOI: 10.1016/j.gie.2014.12.022. [ Links ]
14. Barclay RL, Vicari JJ, Doughty AS, et al. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med 2006;355:2533-41. DOI: 10.1056/NEJMoa055498. [ Links ]
15. Lau PC, Sung JJ. Flat adenoma in colon: Two decades of debate. J Dig Dis 2010;11:201-7. [ Links ]
16. Rembacken BJ, Fujii T, Cairns A, et al. Flat and depressed colonic neoplasms: A prospective study of 1,000 colonoscopies in the UK. Lancet 2000;355:1211-4. DOI: 10.1016/S0140-6736(00)02086-9. [ Links ]
17. Tsuda S, Veress B, Tóth E, et al. Flat and depressed colorectal tumors in a southern Swedish population: A prospective chromoendoscopic and histopathological study. Gut 2002;51:550-5. DOI: 10.1136/gut.51.4.550. [ Links ]
18. Pellisé M, Fernández-Esparrach G, Cárdenas A, et al. Impact of wide-angle, high-definition endoscopy in the diagnosis of colorectal neoplasia: A randomized controlled trial. Gastroenterology 2008;135:1062-8. DOI: 10.1053/j.gastro.2008.06.090. [ Links ]
19. Erim T, Rivas JM, Velis E, et al. Role of high definition colonoscopy in colorectal adenomatous polyp detection. World J Gastroenterol 2011;17:4001-6. DOI: 10.3748/wjg.v17.i35.4001. [ Links ]
20. Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc 2004;59:482-6. DOI: 10.1016/S0016-5107(03)02875-X. [ Links ]
21. Hoffman A, Sar F, Goetz M, et al. High definition colonoscopy combined with I-Scan is superior in the detection of colorectal neoplasias compared with standard video colonoscopy: A prospective randomized controlled trial. Endoscopy 2010;42:827-33. DOI: 10.1055/s-0030-1255713. [ Links ]
22. Participants in the Paris Workshop. The Paris endoscopic classification of superficial neoplastic lesions: Esophagus, stomach, and colon. Gastrointest Endosc 2003;58:S3-43. DOI: 10.1016/S0016-5107(03)02159-X. [ Links ]
23. Ross WA, Thirumurthi S, Lynch PM, et al. Detection rates of premalignant polyps during screening colonoscopy: Time to revise quality standards? Gastrointest Endosc 2015;81:567-74. [ Links ]
24. Zorzi M, Senore C, Da Re F, et al. Detection rate and predictive factors of sessile serrated polyps in an organized colorectal cancer screening program with immunochemical fecal occult blood test: The EQuIPE study (Evaluating Quality Indicators of the Performance of Endoscopy). Gut 2016. (Epub ahead of print) DOI: 10.1136/gutjnl-2015-310587. [ Links ]
25. Le Rhun M, Coron E, Parlier D, et al. High resolution colonoscopy with chromoscopy versus standard colonoscopy for the detection of colonic neoplasia: A randomized study. Clin Gastroenterol Hepatol 2006;4:349-54. DOI: 10.1016/j.cgh.2005.12.009. [ Links ]
26. Brown SR, Baraza W. Chromoscopy versus conventional endoscopy for the detection of polyps in the colon and rectum. Cochrane Database Syst Rev 2010;10:CD006439. [ Links ]
27. Testoni PA, Notaristefano C, Vailati C, et al. High-definition colonoscopy with i-Scan: Better diagnosis for small polyps and flat adenomas. World J Gastroenterol 2012;18:5231-9. [ Links ]
28. Kim WJ, Park SY, Park I, et al. Increased detection of colorectal polyps in screening colonoscopy using high definition i-SCAN compared with standard white light. Clin Endosc 2016;49:69-75. DOI: 10.5946/ce.2016.49.1.69. [ Links ]
29. Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015;81:31-53. DOI: 10.1016/j.gie.2014.07.058. [ Links ]
30. Hassan C, Quintero E, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2013;842-51. DOI: 10.1055/s-0033-1344548. [ Links ]
31. Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after polypectomy: A consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology 2012;143:844-57. DOI: 10.1053/j.gastro.2012.06.001. [ Links ]
32. Tsiamoulos ZP, Misra R, Bourikas L, et al. Sa1423 Endocuff-vision: Impact on colonoscopist performance during screening. Gastrointest Endosc 2015;81:AB209. DOI: 10.1016/j.gie.2015.03.194. [ Links ]
33. Gralnek IM, Segol O, Suissa A, et al. A prospective cohort study evaluating a novel colonoscopy platform featuring full-spectrum endoscopy. Endoscopy 2013;45:697-702. DOI: 10.1055/s-0033-1344395. [ Links ]
34. Gralnek IM. Emerging technological advancements in colonoscopy: Third Eye® Retroscope® and Third Eye® Panoramic TM, Fuse® Full Spectrum Endoscopy® colonoscopy platform, Extra-Wide-Angle-View colonoscope, and NaviAid TM G-EYE TM balloon colonoscope. Dig Endosc 2015;27:223-31. DOI: 10.1111/den.12382. [ Links ]
35. Westwood D, Alexakis N, Connor SJ. Transparent cap-assisted colonoscopy versus standard adult colonoscopy: A systematic review and meta-analysis. Dis Colon Rectum 2012;55:218-25. DOI: 10.1097/DCR.0b013e31823461ef. [ Links ]
36. Dik VK, Moons LM, Siersema PD. Endoscopic innovations to increase the adenoma detection rate during colonoscopy. World J Gastroenterol 2014;20:2200-11. DOI: 10.3748/wjg.v20.i9.2200. [ Links ]
![]() Correspondence:
Correspondence:
Antonio Rodríguez-D'Jesus.
Gastroenterology Department.
Hospital General de Catalunya.
Pedro i Pons, 1.
Sant Cugat del Valles, Barcelona. Spain
e-mail: anjoro76@gmail.com
Received: 20-09-2015
Accepted: 17-03-2016