My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.7 Madrid Jul. 2016
https://dx.doi.org/10.17235/reed.2016.4215/2016
LETTERS TO THE EDITOR
Management of non-surgical pneumoperitoneum
Manejo del neumoperitoneo no quirúrgico
Key words: Pneumoperitoneum. Percutaneous endoscopic gastrostomy (PEG). Gastrostomy.
Palabras clave: Neumoperitoneo. Gastrostomía percutánea endoscópica (PEG). Gastrostomía.
Dear Editor,
Percutaneous endoscopic gastrostomy (PEG) is a safe procedure, although complications have been described. The rate of pneumoperitoneum after PEG oscillates between 0 and 1.2% (1). When related to an extravasation of insufflated air, the use of carbon dioxide for insufflation would reduce this complication given its rapid absorption.
Case report
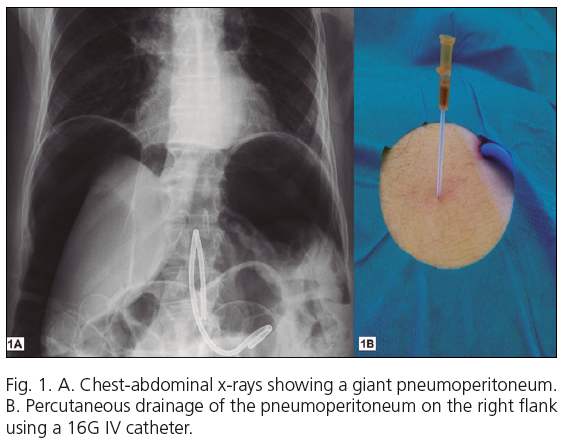
An 85-year-old male not eligible for oral feeding, with anticoagulation for cardiac arrhythmia and on proton-pump inhibitors (PPIs), presented, 6 hours after a PEG procedure to the gastric antrum, dyspnea and abdominal distension with no peritoneal irritation signs. Chest-abdominal X-rays revealed a giant pneumoperitoneum (Fig. 1A). Contrast computerized tomography (CT) revealed a huge pneumoperitoneum compressing the diaphragm and abdominal viscera with no contrast leakage or additional findings. Given the absence of abdominal manifestations, a percutaneous air drainage was performed using a 16G IV catheter (Abbocath-T®) (Fig. 1B). The plastic sleeve was kept in place, and manual abdominal compression maneuvers were carried out. Air removal reduced the abdominal circumference, and the patient remained asymptomatic. The catheter was in place for 2 hours, and was withdrawn after X-rays confirmed the resolved pneumoperitoneum. The patient was discharged from hospital after 4 days.
Key risk factors for PEG-related complications include advanced age, comorbidities, malnutrition, and PPI use (2). Our patient had all of them.
In the presence of pneumoperitoneum after PEG in an asymptomatic patient who is hemodynamically stable with no peritoneal irritation signs, as in our case, non-surgical management should be initially considered (3), with urgent surgery being indicated for individuals with impaired general status or peritoneal irritation signs.
Abdominal decompression by percutaneous puncture is a simple, safe, effective procedure that reduces surgery-associated morbidity and mortality, rapidly resolves pneumoperitoneum, and prevents compartmental syndrome (3).
Antonio José Fernández-López, Francisco Miguel González-Valverde
and Marcelino Méndez-Martínez
Department of General Surgery. Hospital General Universitario
Reina Sofía de Murcia. Murcia, Spain
References
1. Valera Sánchez Z, Pareja Ciuró F, Docobo Durantez F, et al. Neumoperitoneo gigante secundario a gastrostomía percutánea endoscópica. Rev Esp Enferm Dig 2007;99:115-22. DOI: 10.4321/S1130-01082007000200016. [ Links ]
2. Lucendo AJ, Friginal-Ruiz AB. Percutaneous endoscopic gastrostomy: An update on its indications, management, complications, and care. Rev Esp Enferm Dig 2014;106:529-39. [ Links ]
3. García-Santos E, Puerto-Puerto A, Sánchez-García S, et al. Síndrome compartimental abdominal por neumoperitoneo a tensión secundario a barotrauma. Presentación de un caso. Cir Cir 2015;83:429-32. DOI:10.1016/j.circir.2015.05.046. [ Links ]











 text in
text in