My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.9 Madrid Sep. 2016
PICTURES IN DIGESTIVE PATHOLOGY
Actinomyces infection as a complication of a post-radiotherapy rectal ulcer
Úlcera rectal postradioterapia complicada con infección por Actinomyces
Carmen Martos-Plasencia, Pilar Olivencia-Palomar, Roberto Patón-Arenas, Cristina Verdejo-Gil, Rosario Salmoral-Luque, Melvyn Peña-Gómez, Eva de-la-Santa-Belda, Bartolomé López-Viedma and José Olmedo-Camacho
Department of Gastroenterology. Hospital General Universitario de Ciudad Real. Ciudad Real, Spain
Background
Brachytherapy, as a part of the treatment in prostate cancer, could associate early and late local complications in the rectum (1,2). Actinomyces usually grows as an opportunistic infection in ischemic-necrotic tissue. It is rarely involved in actinomycosis, a disease which consists in the development of oral, pulmonary and gastrointestinal abscess (3,4).
Case Report
We present the case of a 72-year-old man who underwent radical prostatectomy after he had been diagnosed with adenocarcinoma. After three years, the patient presented a biochemical recurrence of the disease, so that he received 33 brachytherapy sessions.
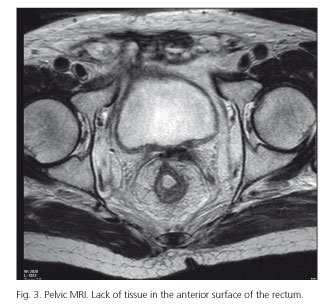
Five month later, he was admitted for rectal pain and bleeding. A colonoscopy was performed, revealing a severe proctitis, diffuse edema, and ulceration. The entire rectal surface was covered with an exudate, areas of necrosis and a nodular pseudopolyp formation. In the central area of a large ulcer there was a depression with a fistulous opening (Fig. 1). Feces for microbiological testing and biopsy specimen were taken. The pathology report described a granulation tissue and degenerative thickening of blood vessel wall compatible with actinic proctitis. Furthermore, there were PAS-positive granules suggestive of typical actinomycosis "sulfur granules" (Fig. 2). A pelvic MRI showed a lack of tissue of 29 x 13 mm in the anterior surface of the rectum. Moreover, there was an absence of sphincter and a fistulous tract between the rectum and the prostatectomy bed. It was difficult to control anal pain; therefore, the use of opioids drugs was needed. The patient started an antibiotic regimen with levofloxacin and metrominazol.
Finally, a discharge colostomy was performed in order to interrupt the intestinal transit through the affected rectal area. Currently, the patient is receiving hyperbaric treatment as an attempt to improve tissue oxygenation. This might increase healing and re-epithelialization capacities in the anterior rectal wall.
References
1. Krol R, Smeenk RJ, Van Lin EN, et al. Systematic review: Anal and rectal changes after radiotherapy for prostate cancer. Int J Colorectal Dis 2014;29:273-83. DOI: 10.1007/s00384-013-1784-8. [ Links ]
2. Wolff JH, Goldberg EM, Drachenberg CB. Large solitary rectal ulcer as a complication of prostate brachytherapy. Gastrointest Endosc 2009;70:389-90; discussion 90. DOI: 10.1016/j.gie.2009.04.026. [ Links ]
3. Bowden GHW. Actinomycosis in: Baron's Medical Microbiology. Baron S, et al. eds. 4th ed. Univ of Texas Medical Branc; 1996. [ Links ]
4. Coremans G, Margaritis V, Van Poppel HP, et al. Actinomycosis, a rare and unsuspected cause of anal fistulous abscess: Report of three cases and review of the literature. Dis Colon Rectum 2005;48:575-81. DOI: 10.1007/s10350-004-0809-3. [ Links ]











 text in
text in