My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.6 Madrid Jun. 2018
https://dx.doi.org/10.17235/reed.2018.5062/2017
ORIGINAL PAPERS
A prospective, controlled assessment of the technical characteristics of a novel forward-viewing echoendoscope
1Servicios de Gastroenterología y Hepatología. IRYCIS. Hospital Universitario Ramón y Cajal. Madrid. Spain
2Servicio de Gastroenterología. Hospital Universitario Quirón. Madrid. Spain
3Servicios de Anatomía Patológica. IRYCIS. Hospital Universitario Ramón y Cajal. Madrid. Spain
INTRODUCTION
Endoscopic ultrasound (EUS) was introduced in the early 1980s 1,2,3 and has had a strong impact in the management of many diseases. Especially for the preoperative diagnosis and staging of malignancies 4,5,6,7,8 and the study of the bile duct and benign pancreatic conditions 9,10,11. EUS also allows tissue samples to be obtained under real-time echoendoscopic guidance with fine-needle aspiration (EUS-FNA). Sample collection is usually performed with a complex echoendoscope that, in contrast to conventional endoscopes, provides an oblique rather than a forward view image with respect to the longitudinal axis of the endoscope. Similarly, the ultrasonic plane is also lateral to the endoscope's longitudinal axis. Finally, the working channel through which the fine needle is advanced is also oblique to the endoscope's longitudinal axis (oblique-viewing curved linear array, OV-CLA). This complex design allows the needle and ultrasonic bundle to be on the same plane, which facilitates safe and efficient punctures. However, this echoendoscope has some limitations from a technical perspective 12, including an inadequate visualization in a retroflex position. The so-called push-back phenomenon occurs due to the force that is applied for puncturing with the needle, which pushes the endoscope backwards due to the angled working channel. This results in difficulties to advance the therapeutic devices (stents, dilators, etc.) due to the above-mentioned angled channel and the presence of an elevator at the tip of the endoscope 12. Recently a forward-viewing curved linear array (FV-CLA) echoendoscope has been introduced, which might theoretically overcome the above limitations of OV-CLA devices 13. The FV-CLA provides a forward view (endoscopy and ultrasound), a working channel that runs parallel (rather than oblique) to the optics and an ultrasonic plane that is frontal rather than lateral to the tip of the endoscope (only 90 degrees of US vision). It has been hypothesized that these differential characteristics may facilitate the performance of EUS-FNA and/or endoscopic therapy, due to an improved instrument force transmission. These characteristics make the FV-CLA a highly promising echoendoscope, particularly for therapeutic procedures (pseudocyst drainage, celiac plexus neurolysis, etc.). However, the evidence to date of the potential benefit of the FV-CLA over the OV-CLA is scarce and even the most appropriate indications and locations/stations remain unclear. There are no reports of the use of this new echoendoscope in the gastroenterology field. Therefore, this prospective study was performed to assess the clinical performance of the FV-CLA in the upper GI tract in a systematic and controlled manner.
MATERIAL AND METHODS
The study was carried out at two university hospitals in the Autonomous Community of Madrid. The prospectively collected information was stored in a database for subsequent analysis. The study was approved by the hospital's ethics committee. A total of 45 patients were prospectively and consecutively included in the study during January and February 2016. Inclusion criteria: all patients referred for EUS due to a clinically established indication. Exclusion criteria: a patient refusal to participate and a contraindication for sedation. The procedures were performed by three expert echoendoscopists (JFO, FGP, EVS) with more than five years of experience in EUS and EUS-FNA with conventional echoendoscopes (OV-CLA) and no prior experience with a FV-CLA. All participating echoendoscopists routinely use the same model of linear echoendoscope in their daily practice, the Olympus GF-UC160P OL5 with an Aloka Model Alpha 5 or 7 ultrasound console.
Information regarding patient baseline characteristics and EUS indication was collected. The conventional endosonographic stations and most significant structures explored during EUS were routinely assessed in all patients. These included stations 2, 4L, 5, 7, 8, 9, perigastric and periduodenal space, celiac trunk, gastrohepatic ligament, pancreatic region, pyloric antrum, gallbladder and the common bile duct. A score was assigned from 0 to 10 for visualization quality (0 = poor visualization/image and 10 = best visualization/image) according to a visual analog scale (VAS). Echoendoscope maneuverability was also assessed using a VAS from 0 to 10, with 0 representing the poorest maneuverability and 10, the best maneuverability (10 was equivalent to using a conventional gastroscope). Ratings were grouped together as follows: grade "A" (VAS score between 9 and 10), grade "B/C" (VAS score between 7 and 8) and grade "D" (VAS score < 7). The participating echoendoscopists met twice before beginning the study in order to establish the characteristics of each endosonographic station and the technical aspects required to assign a score of 0 to 10 on a VAS.
A number of technical aspects of the EUS-FNA procedure performed with the FV-CLA were also assessed; these included the difficulty of puncturing and needle visibility in the ultrasonographic plane using a VAS 0-10 (as with the above items). Lesion type and histopathology, diagnostic accuracy and the rate of adverse events associated with EUS and EUS-FNA were also documented.
Equipment
A forward-viewing echoendoscope (TGF-UC180J, Olympus(r) Medical Systems, Japan) connected to an EU-ME2 ultrasound processor (Olympus(r) Medical Systems, Japan) was used in all procedures. Conventional COOK 22G (EchoTip(r) Ultra ECHO 3-22) and 19G (EchoTip(r) Ultra ECHO-19) cytology needles were used for the study. EUS-FNA was performed as per the standard technique and every FNA sample was assessed by an onsite pathologist.
Statistical analysis
A descriptive analysis was performed of the results obtained. A commercially available statistical software was used for data analysis (JMP version 7.0.2, SAS Institute Inc., Cary, NC). Discrete variables are presented as a percentage with confidence interval (95% CI) and continuous variables are shown as mean, standard deviation (SD) and range (or median and interquartile range in the case of non-normally distributed variables). Statistical analysis were carried out using the Pearson χ2 test or Fisher's exact test for discrete variables. The analysis of variance or Mann-Whitney U-test was used for continuous variables, depending on data distribution. Statistical significance was set at a p value of < 0.05. All authors had access to the final results of the study, for review and approval.
RESULTS
A total of 45 consecutive patients were included during the study enrollment period. All EUS procedures included in the statistical analysis were performed in the upper GI tract. The most common indication was a clinical suspicion of a pancreatic tumor (12 cases, 26.6%) (Table 1).
Table 1 Baseline characteristics of patients (n = 45)

IQR: interquartile range; WOPN: walled-off pancreatic necrosis.
EUS and EUS-FNA characteristics are listed in Table 2. All procedures were carried out by an expert echoendoscopist and were completed until reaching the second part of the duodenum without significant difficulties. Lesions were punctured under FV-CLA guidance according to the present findings in 20 of 45 procedures (45.5%). FV-CLA manageability was rated overall with an "A" by all three echoendoscopists. Ease of passage through the oropharynx and overall visibility in the ultrasonographic plane were rated overall with a "B/C" by the experts involved in the study.
Table 2 General characteristics of the procedures
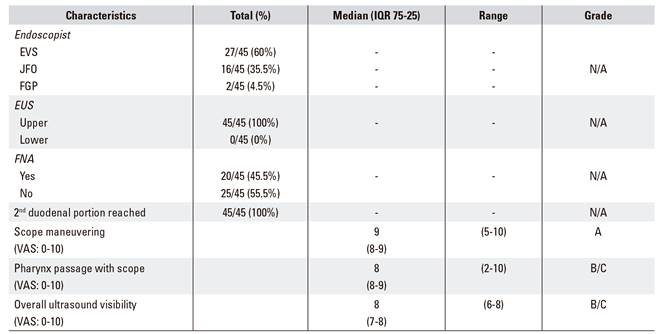
IQR: interquartile range; FNA: fine needle aspiration; VAS: visual analog scale; N/A: not applicable; EUS: endoscopic ultrasound.
The rating of structure and both thoracic and abdominal station assessment with the FV-CLA is shown in Table 3. Visualization and characterization were rated with an "A" grade (score of 9-10 over 10) for the mediastinal station 7 (subcarinal), gastrohepatic ligament, gallbladder, and pancreatic body and neck. Mediastinal stations 4L and 5 (left inferior paratracheal/aortopulmonary window and subaortic, respectively) were rated with a "D" grade (score < 7 over 10) due to difficulties to obtain an adequate endosonographic image.
Table 3 Assessment of the thoracic and abdominal structures with FV-CLA

VAS: visual analog scale; IQR: interquartile range.
With regard to the difficulty to perform EUS-FNA with the forward-view echoendoscope (FV-CLA) (Table 4), the overall rating by the expert endoscopists was grade "B" and needle visibility was also rated with a "B". Punctures were mainly performed from the gastric body (40%). However, they were carried out from the second duodenal portion in 20% of cases and from the duodenal bulb in 15% of procedures. Other areas where EUS-FNA was performed included the celiac trunk, gastrohepatic ligament, stations 7 and 8 and the gastric antrum (5% each). Despite the fact that adenopathies were the lesions that were most commonly punctured (20%), samples were also taken from solid and cystic lesions in the pancreatic head, uncinate process, body and tail, among others. Cytopathology results (provided by an on-site pathologist) included neoplasm (65%), necrosis, pseudocyst and benign lesions (10% each) and an abscess of an adenopathy in one case. The EUS-FNA diagnostic accuracy was 90% (18/20 cases, 95% CI: 68-99). Two punctures initially had a negative cytology and were subsequently diagnosed as malignant by other diagnostic tests. The median number of needle passes performed during the procedure was 1 (range 1-4).
Table 4 FNA features with FV-CLA

FNA: fine needle aspiration; IQR: interquartile range; VAS: visual analog score; N/A: not applicable; WOPN: walled-off pancreatic necrosis.
Adverse events developed in 2.2% of procedures (with or without FNA) (1/45 cases, 95% CI: 0-12%). Mild complications recorded included bleeding as the needle was withdrawn after the puncture of a pancreatic pseudocyst. This adverse event was successfully treated by the placement of a fully covered self-expandable metal stent (complication rate for EUS-FNA, 1/20 cases, 5%, CI: 0-25%).
DISCUSSION
This initial study that systematically assessed the performance characteristics of the forward-view echoendoscope (FV-CLA) has clearly shown the clinical usefulness and the diagnostic yield of this new device in our field. This study shows that, in expert hands, diagnostic accuracy approaches 90% with a complication rate of approximately 2%.
Most studies to date of the use of a FV-CLA have only evaluated uncontrolled cases 14,15,16 where areas of interest are not systematically examined during the procedure. These studies have provided biased data that do not allow an understanding of the limitations and strengths of this new tool. Despite the fact that some studies have compared the performance characteristics of the OV-CLA and the FV-CLA 17,18,19, no study to date has consistently assessed the usefulness of the FV-CLA at the various echoendoscopic stations in a prospective cohort of patients.
This study provides a systematic description of the different endosonographic stations with the FV-CLA by following a pre-established protocol including prospective data collection. This represents a novel approach compared to previously reported studies. The rating system by expert echoendoscopists (using a VAS 0-10), even though it may be considered to be subjective, provides the opinion of experts of the difficulties to perform endosonographic examinations with this new device.
The degree of flexibility of this novel echoendoscope, which has a wide forward view (120°), allows the second portion of the duodenum to be easily reached and a number of intervening stations were studied in all cases. The passage through the oropharynx does not seem to be particularly difficult, in contrast with reports from other studies 12. However, the ultrasonographic plane provided by the transducer, which is narrower than usual (90°), may occasionally provide a suboptimal visibility of the sonographic plane. This may require angulation of the distal end for an appropriate visualization of adjacent structures in some stations. This is the case with some of the structures that can be observed from the esophageal body. For this reason, mediastinal 4L and 5 stations received the poorest grades by the echoendoscopists. This suggests that the FV-CLA may not be appropriate for patients requiring FNA in these mediastinal areas. The gastric cavity provided more space to bend the tip of the endoscope, which facilitated the desired views, and other structures could also be reached from the gastric body. These were better visualized as compared to periesophageal structures. Angulation issues when seeking an appropriate plane may also occur when studying the bulb and second duodenal portion. However, this occurred to a lesser extent than in the esophagus in the present prospective study.
Attempting to assess the theoretical advantages of the FV-CLA versus the OV-CLA may be challenging. We found that, on occasions, the "push back" phenomenon may persist with the FV-CLA. Even though the working channel runs parallel to the tube, which should theoretically allow a more effective force transmission when accessing lesions. The push back effect may lead to an unstable scope position and, together with the narrower ultrasonic field and the absence of a tip elevator, may result in a loss of the needle out of the sonographic plane. This makes the puncture a little more challenging. However, our experience with therapeutic maneuvers such as draining pancreatic collections, was successful without great difficulty (Fig. 1). This potential inconvenience did not preclude the performance of EUS-FNA in any of the 20 patients whose lesions were punctured. This impression is consistent with reports by other groups who found no differences compared with the OV-CLA 20. Visualization of the common bile duct has been reported to be more accurate than with an OV-CLA 12. However, this procedure was graded as a "B/C" in our study, which suggests that bile duct drainage may not be an appropriate indication for the FV-CLA. However, the frontal viewing echoendoscope provides excellent views of the gallbladder and intrahepatic duct (gastrohepatic ligament), so it may become a highly valuable tool to perform cholecystogastrostomies and hepatogastrostomies in the near future 21. This is also true for the pancreatic body, where cystogastrostomy may be facilitated by the direct, frontal access provided by the FV-CLA. However, such potential therapeutic uses of the FV-CLA must be validated in future prospective studies by comparing the results with those of the conventional system (OV-CLA). Similarly, it would be interesting to assess whether the placement of lumen apposing self-expandable metal stents, such as the AXIOS(r) stent (Boston Scientific), is easier with a FV-CLA or with an OV-CLA. Therefore, the friction resulting from stent advancement through the distally angled working channel in an OV-CLA could be avoided. Twelve lower GI tract echoendoscopies were performed out-of-protocol with the FV-CLA, although this data was not included in the analysis. The splenic angle was readily reached in all cases. The forward view provided by this echoendoscope represents an advantage when the target lesion is located in the proximal colon, as advancing through the colon may be safer with the novel forward viewing echoendoscope as compared to the oblique viewing device 22. Some studies have suggested that this device may be useful for the study of fibrosis in advanced polyps, which would help to predict the possibilities of a successful resection 23.

Fig. 1 A and B. FV-CLA images showing the drainage of a pancreatic collection that was identified by endoscopic ultrasound. C-F. The radiographic control shows how the FV-CLA follows the longitudinal axis of the echoendoscope to reach the collection, rather than the oblique path seen with a conventional OV-CLA (G).
Our study has some limitations which deserve further discussion. Firstly, this was a pilot study with a relatively small number of patients (n = 45). Furthermore, heterogeneous lesions were evaluated and EUS-FNA was performed in some cases from different locations, which may limit the robustness of the conclusions drawn. Therefore, further prospective, comparative, randomized studies are needed in order to make definitive conclusions.
In summary, we report, for the first time in our field, the potential usefulness of the forward-viewing echoendoscope (FV-CLA) for the diagnosis and treatment of lesions in the GI tract and adjacent structures. The findings of this prospective, controlled study highlight multiple areas that are better visualized and accessed with this type of echoendoscope (gallbladder, gastrohepatic ligament, subcarinal region). This may be important in the future when planning EUS-guided therapies in the aforementioned areas. Further prospective, randomized studies are needed to verify the potential superiority of the forward-view echoendoscope over the oblique-view device for indications such as cholecystogastrostomy or hepatogastrostomy. The promising results obtained in this preliminary study support the future research in the field.
BIBLIOGRAFÍA
1. DiMagno EP, Buxton JL, Regan PT, et al. Ultrasonic endoscope. Lancet 1980;22;1629-31. DOI: 10.1016/S0140-6736(80)91122-8 [ Links ]
2. Wiersema MJ, Kochman ML, Chak A, et al. Real-time endoscopic ultrasound-guided fine-needle aspiration of a mediastinal lymph node. Gastrointest Endosc 1993;39:429-31. DOI: 10.1016/S0016-5107(93)70122-4 [ Links ]
3. Chang KJ, Albers CG, Erickson RA, et al. Endoscopic ultrasound-guided fine needle aspiration of pancreatic carcinoma. Am J Gastroenterol 1994;89: 263-6. [ Links ]
4. Eloubeidi MA, Jhala D, Chhieng DC, et al. Yield of endoscopic ultrasound-guided fine-needle aspiration biopsy in patients with suspected pancreatic carcinoma. Cancer 2003;99:285-92. DOI: 10.1002/cncr.11643 [ Links ]
5. Vázquez-Sequeiros E, Levy MJ, Clain JE, et al. Routine vs. selective EUS-guided FNA approach for preoperative nodal staging of esophageal carcinoma. Gastrointest Endosc 2006;63:204-11. DOI: 10.1016/j.gie.2005.08.053 [ Links ]
6. Vázquez-Sequeiros E, Wiersema MJ, Clain JE, et al. Impact of lymph node staging on therapy of esophageal carcinoma. Gastroenterology 2003;125:1626-35. DOI: 10.1053/j.gastro.2003.08.036 [ Links ]
7. Laudanski J, Kozlowski M, Niklinski J, et al. The preoperative study of mediastinal lymph nodes metastasis in lung cancer by endoscopic ultrasonography (EUS) and helical computed tomography (CT). Lung Cancer 2001;34(Suppl 2):S123-6. DOI: 10.1016/S0169-5002(01)00353-1 [ Links ]
8. Polkowski M, Palucki J, Wronska E, et al. Endosonography versus helical computed tomography for locoregional staging of gastric cancer. Endoscopy 2004;36:617-23. DOI: 10.1055/s-2004-814522 [ Links ]
9. El Chafic AH, Dewitt J, Leblanc JK, et al. Impact of preoperative endoscopic ultrasound-guided fine needle aspiration on postoperative recurrence and survival in cholangiocarcinoma patients. Endoscopy 2013;45:883-9. DOI: 10.1055/s-0033-1344760 [ Links ]
10. Pérez-Miranda M, De la Serna-Higuera C. EUS access to the biliary tree. Curr Gastroenterol Rep 2013;15:349. DOI: 10.1007/s11894-013-0349-x [ Links ]
11. Barthet M, Lamblin G, Gasmi M, et al. Clinical usefulness of a treatment algorithm for pancreatic pseudocysts. Gastrointest Endosc 2008;67:245-52. DOI: 10.1016/j.gie.2007.06.014 [ Links ]
12. Takuji Iwashita, Yousuke Nakai, John G Lee, et al. Newly-developed, forward-viewing echoendoscope: a comparative pilot study to the standard echoendoscope in the imaging of abdominal organs and feasibility of endoscopic ultrasound-guided interventions. J Gastroenterol Hepatol 2012;27:362-7. DOI: 10.1111/j.1440-1746.2011.06923.x [ Links ]
13. Imaizumi H, Irisawa A. Preliminary experience of a prototype forward-viewing curved linear array echoendoscope in a training phantom model. Dig Endosc 2010;22(Suppl 1):S123-7. DOI: 10.1111/j.1443-1661.2010. 00975.x [ Links ]
14. Voermans RP, Eisendrath P, Bruno MJ, et al. Initial evaluation of a novel prototype forward-viewing US endoscope in transmural drainage of pancreatic pseudocysts (with videos). Gastrointest Endosc 2007;66:1013-7. DOI: 10.1016/j.gie.2007.02.057 [ Links ]
15. Larghi A, Seerden TC, Galasso D, et al. EUS-guided therapeutic interventions for uncommon benign pancreaticobiliary disorders by using a newly developed forward-viewing echoendoscope (with videos). Gastrointest Endosc 2010;72(1):213-5. DOI: 10.1016/j.gie.2009.11.003 [ Links ]
16. Fusaroli P, Cortecchia S, Caletti G. EUS-FNA using a forwardview echoendoscope in difficult cases. J Gastrointestin Liver Dis 2011;20:216-7. [ Links ]
17. Voermans RP, Ponchon T, Schumacher B, et al. Forward-viewing versus oblique-viewing echoendoscopes in transluminal drainage of pancreatic fluid collections: a multicenter,randomized, controlled trial. Gastrointest Endosc 2011;74:1285-93. DOI: 10.1016/j.gie.2011.07.059 [ Links ]
18. Matsuzaki I, Miyahara R, Hirooka Y, et al. Forward-viewing versus oblique-viewing echoendoscopes in the diagnosis of upper GI subepithelial lesions with EUS-guided FNA: a prospective, randomized, crossover study. Gastrointest Endosc 2015;82:287-95. DOI: 10.1016/j.gie.2014.12.051 [ Links ]
19. Eloubeidi MA. Initial evaluation of the forward-viewing echoendoscope prototype for performing fine-needle aspiration, Tru-cut biopsy, and celiac plexus neurolysis. J Gastroenterol Hepatol 2011;26:63-7. DOI: 10.1111/j.1440-1746.2010.06409.x [ Links ]
20. Fusaroli P, Ceroni L, Caletti G. Forward-view endoscopic ultrasound: a systematic review of diagnostic and therapeutic applications. Endosc Ultrasound 2013;2:64-70. DOI: 10.4103/2303-9027.117689 [ Links ]
21. Trevino JM, Varadarajulu S. Initial experience with the prototype forward-viewing echoendoscope for therapeutic interventions other than pancreatic pseudocyst drainage (with videos). Gastrointest Endosc 2009;69:361-5. DOI: 10.1016/j.gie.2008.09.021 [ Links ]
22. Uchida N, Galasso D, Seerden TC, et al. EUS-FNA of extracolonic lesions by using the forward-viewing linear echoendoscope. Gastrointest Endosc 2010;72:1321-3. DOI: 10.1016/j.gie.2010.03.1068 [ Links ]
23. Makino T, Kanmura S, Sasaki F, et al. Preoperative classification of submucosal fibrosis in colorectal laterally spreading tumors by endoscopic ultrasonography. Endosc Int Open 2015;3:E363-7. DOI: 10.1055/s-0034-1391782 [ Links ]
Received: May 22, 2017; Accepted: December 11, 2017











 text in
text in 

