My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.6 Madrid Jun. 2018
https://dx.doi.org/10.17235/reed.2018.5207/2017
ORIGINAL PAPERS
Outbreak of acute hepatitis A in the health area served by the Hospital Universitario Virgen de la Victoria (HUVV): a change in epidemiology
1UGC de Aparato Digestivo. Instituto de Investigación Biomédica de Málaga (IBIMA). Hospital Universitario Virgen de la Victoria. Málaga. Spain
2Centro de Investigación Biomédica en Red de Enfermedades Digestivas y Hepáticas (CIBERehd). UGC de Microbiología y Parasitología. Hospital Universitario Virgen de la Victoria. Málaga. Spain
3Medicina Preventiva y Epidemiología. Hospital Universitario Virgen de la Victoria. Málaga. Spain
INTRODUCTION
Hepatitis A virus (HAV) usually induces a self-limited acute infectious illness in humans. Transmission is mainly via the fecal-oral route due to contaminated water and food, and may also occur due to person-to-person contact. Sexual transmission has been associated with epidemic outbreaks among men who have sex with men (MSM) since 1980 1, some of these cases in Spain 2,3,4. However, recent reports suggest that this is related to the European hepatitis A outbreak in 2016 5. Outbreaks have also been reported in parenteral drug users in association with infected fomites blood transfusion recipients 6). Infection is usually asymptomatic or mild in children and more severe in adults. The mean incubation period is 28 days and infectiveness peaks during the second half of the incubation period when patients are still asymptomatic. Most cases are deemed as noncontagious from one week after jaundice onset. Diagnosis relies on serologic testing, and the presence of anti-HAV immunoglobulin M (IgM) or HAV-RNA are indicative of an acute infection 7. No specific therapy is available for acute infection with HAV. Stringent hygiene measures, avoidance of risky contact and vaccination of exposed individuals have proven effective to prevent new cases. Both active and passive immunization are effective when administered within two weeks after exposure 8.
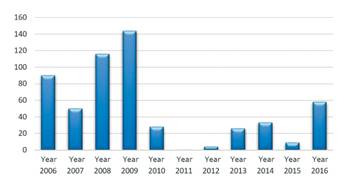
Improved hygienic and healthcare conditions in Spain have contributed to a reduced fecal-oral viral transmission. During 2008-2009, a significant outbreak via water transmission was recorded in our health area. No relevant outbreaks were recorded until 2016, when cases notably increased during the last few months of the year. This situation persists as of today, as reported by the World Health Organization 9. This may result from a lower number of immunized individuals but also from increasing sexual transmission.
The goal of the study was to describe an epidemic outbreak of hepatitis A in our setting with epidemiological and clinical characteristics of cases and to assess potential changes in viral transmission mechanisms.
MATERIALS AND METHODS
A retrospective study was carried out from January 1st to December 31st 2016 at the Hospital Universitario Virgen de la Victoria in Málaga. The study included all patients who had suffered from acute HAV infection and for whom a serum sample was analyzed by the microbiology laboratory. IgM against HAV was tested in 3,440 patients in 2016. Anti-HAV immunoglobulin G (IgG) and IgM antibodies were detected using a lateral-flow immunochromatographic immunoassay (ORTHO(r), Clinical Diagnostics).
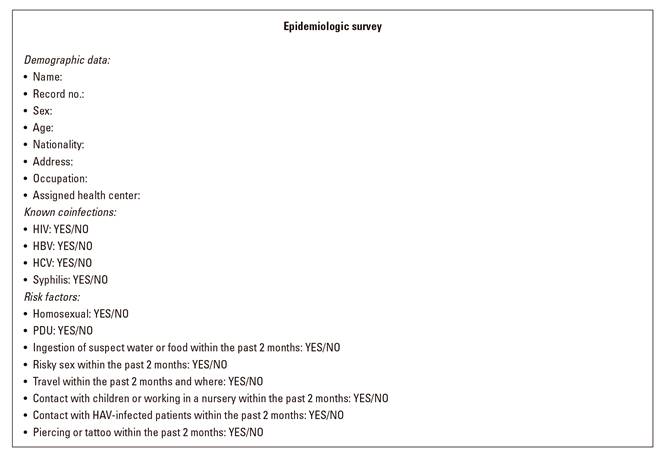
The following variables were analyzed: sex, nationality, date of diagnosis, presence of a coinfection with human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV) or Treponema pallidum. In addition, risk factors for infection (using an epidemiologic survey [Fig. 1]) as well as biochemistry parameters (aminotransferases, total bilirubin, gamma-glutamyl transpeptidase [GGT], alkalyne phosphatase [AP], international normalized ratio [INR] and prothrombin time [%]), the presence of free fluid on abdominal US scans and other clinically interesting aspects (hepatic encephalopathy, need for hospitalization or admission to an ICU and length of hospital stay) were also analyzed.
Data were analyzed using the IBM SPSS Statistic 21 software package, primarily using descriptive statistics such as frequency distribution and percentage for qualitative variables and central tendency measures, dispersion and position for quantitative variables. The Kolmogorov-Smirnov normality test was used to determine the variables with and without a normal distribution. Variables meeting the normality criteria are expressed as mean, standard deviation and 95% confidence intervals, whereas variables not meeting this criteria are shown as median and interquartile range (IQR) values.
The study complied with the Spanish Law 14/2007, dated July 3rd, of biomedical research, and all personal data were kept confidential (Organic Law 15/1999, December 13th, for the protection of personal data). Personal data were anonymized in a central database, which is protected by a password known by authorized study staff.
RESULTS
Of all 3,440 samples that were tested, 58 (1.7%) were positive for anti-HAV IgM and 51 patients received a positive test during an episode of acute hepatitis. These subjects were included in the study. Figure 2 shows a histogram of all cases identified in our health area during the past ten years; the previously mentioned significant increase is shown for the last year. Table 1 shows the patient characteristics that were considered. Forty-six (90%) were male with a mean age of 35.75 years (95% CI: 33-39). The cases were predominantly Spanish (82%), followed by Finnish and Romanian cases (4% each). No cases were identified among tourists and none of the cases had recently been abroad.
Table 1 Demographic, clinical and laboratory characteristics of patients in the study cohort
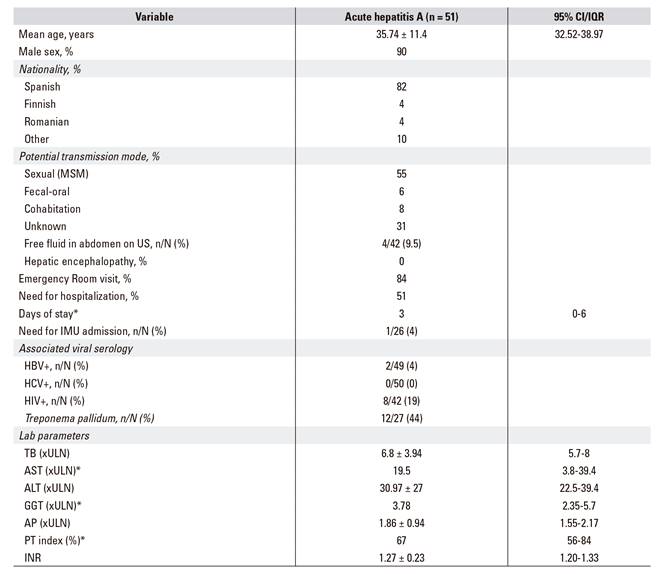
*Variables not following a normal distribution. MSM: men who have sex with men; IMU: intensive medicine unit; HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus; TB: total bilirubin (ULN 0,3 mg/dl); ULN: upper limit of normal; AST: aspartate aminotransferase (ULN = 40 IU/l); ALT: alanine aminotransferase (ULN = 50 IU/l); GGT: gamma-glutamyl transpeptidase (ULN = 28 IU/l); AP: alkaline phosphatase (ULN = 190 IU/l); PT: prothrombin time; INR: international normalized ratio.
An increase in the number of cases was seen during November and December and 31 (60%) were identified during these two months. This trend persisted from January to May 2017. A structured epidemiologic survey was performed with 42 patients (the remaining cases refused to participate) in order to identify the transmission mechanism involved. Twenty-six (62%) acknowledged that they were MSMs and 19 (73%) said that they had had risky sex within two months before diagnosis. Furthermore, the initial cases had visited the same sexual encounter venues. An additional four patients said they were not MSMs but admitted to having had risky sex. Overall, sexual transmission seemed to be the primary risk factor in 55% of subjects, followed by the fecal-oral (6%) and cohabitation (8%) mechanisms. A potential transmission mechanism was not identified in 31% of subjects.
Cases were primarily identified via the Emergency Room (84%) due to symptomatic hepatitis. Twenty-six of these cases required hospital admission (51%) mainly due to impaired coagulation times, with a median prothrombin time (PT) of 67% (IQR 56-84%) and an INR of 1.27 ± 0.23, (95% CI 1.20-1.33). Abdominal US scans were obtained from 42 subjects, four (9.5%) of whom had free intraperitoneal fluid, albeit in small amounts. The median stay for admitted patients was three days (IQR 0-6). One patient (4%) had to be admitted to the ITU for three days due to severe coagulopathy (INR 2.2) and received a frozen fresh plasma transfusion. No subjects had hepatic encephalopathy and there were no cases of fulminant liver failure, liver transplantation or death.
With regard to laboratory tests, the standardized means of liver function parameters on admission according to the upper normal limit were as follows: total bilirubin (TB) 6.8 ± 3.94 (95% CI 5.7-8.0), aspartate aminotransferase (AST) 19.5 (IQR 3.8-39.4), alanine aminotransferase (ALT) 30.97 ± 27.00 (95% CI 22.5-39.4), GGT 3.78 (IQR 2.35-5.70) and AP 1.86 ± 0.94 (95% CI 1.55-2.17). With regard to the associated viral serology, two patients (4%) had chronic HBV liver disease and were under treatment with tenofovir, one of whom had cirrhosis and evidence of portal hypertension. Eight cases were HIV+ (19%), one diagnosed with an acute episode and 12 patients (44%) had a positive serology for Treponema pallidum according to nontreponemal tests (RPR).
DISCUSSION
The patient profile in our area is a Spanish adult male. Sexual intercourse among men who have sex with men is the primary risk factor for HAV transmission and represents a change in the traditional epidemiology of this disease. Half of the cases in this study required hospital admission, mainly due to coagulopathy, which highlights the significance of this epidemiologic change due to the increased number of hospital admissions for acute hepatitis during the study period. No cases had serious complications. Ironically, there is no HAV vaccine available at present in our health area, therefore therapy with gamma-globulin was selected and administered to cohabitants. The main limitation of our study, in comparison with other reported European studies, is the absence of viral sequencing in order to relate our cases to the two strains mainly responsible for infection among European populations. Furthermore, whether the increased number of cases resulted from reduced protection, increased promiscuity, or changing hygiene in the area is difficult to ascertain. The origin was unknown in up to 30% of cases but high-risk sexual activities were often concealed due to patient privacy. The fact that the initially described patients among the MSM population had all visited sexual encounter venues in a nearby town favors the theory of increased promiscuity as a cause. Even though this association became weaker as the outbreak progressed, it is reasonable to conclude that cases who visited these venues subsequently passed on the infection via sexual intercourse and to their cohabitants via the traditional fecal-oral transmission route.
As of January 2017 5,10, 37 cases of hepatitis A had been reported in MSM patients throughout the United Kingdom; nine (24.3%) cases said they had recently travelled to Spain, where they had risky sex. Cases have also been reported in Ireland, Sweden and Germany involving individuals who had recently visited Spain, and the European Centre for Disease Prevention and Control (ECDC) described two outbreaks in Europe in 2016 5,11. With regard to the so-called strain 1 11, 24 cases were reported in the UK with the VRD_521_2016 sequence, IA genotype; 22 of these were males from 19 to 63 years of age, with a mean age of 35 years and 79% acknowledged their MSM status. Eight of these cases had visited Spain during the incubation period. Cases were reported both in Ireland and Sweden who had recently travelled to Spain. While reported cases have increased both in Italy and Spain, no genotype studies have been performed that show an association with event 1. This is consistent with our cohort, with a mean age of 35.6 years, 90% were males and MSM status was acknowledged by 55% of cases.
With regard to strain 2 with the RIVM-HAV16-090 sequence and IA genotype, ten of 13 cases were reported from a total of 48 that were described in the Netherlands 12 during the "Europride" festival in July 2016; 17 (35%) were MSMs with a mean age of 35 years. With regard to the 29 non-MSM male patients, the reported mean age was lower (20 years) and most came from countries such as Turkey, Romania and Morocco. Thirteen cases have been reported with this strain in the UK; 12 were males with a mean age of 39 years and 75% of these acknowledged their MSM status. Seven of these patients had travelled to Spain during the incubation timeframe and two had visited Germany; the epidemiologic data were similar to those of our patients.
In our health area alone, 26 cases have been reported in MSM up to December 31st 2016. Even though there are no reports based on the country as a whole, travelling to Spain is clearly considered as a risk factor for the disease by international publications 11. The similarities of our cohort with those reported in the UK and the Netherlands should be highlighted. This includes a similar mean age of 25 years, a high proportion of males and homosexual intercourse as the primary risk factor. This should also be compared to other cohorts such as an epidemiologic study from 2010 to 2014 in Spain 13. In this study, females were almost as numerous as males (41% of women), with a younger mean age than that reported in our cohort and the aforementioned European series (24.48 vs 35.7 years). Compared to studies in developing countries, the epidemiology is not associated with the outbreak in our health area but more closely resembles the Spanish reports during 2014. In China, the primary risk factor for this disease is no vaccination and agricultural work 14. Similarly in Taiwan 15, the mean age at the time of transmission is lower and the fecal-oral route is the primary mechanism. An outbreak with nearly 1,000 cases was recently reported in northern Taiwan and should be highlighted here; 70% of cases involved MSMs, 60% were HIV-positive and 60% were associated with sexually transmitted diseases such as syphilis and gonorrhea. The causal sub-genotype in this outbreak was IA, the same as in Europe, with epidemiologic parameters closely resembling our cohort 15,16.
Also outside Europe, an outbreak of hepatitis A was reported in 2016 in Tel Aviv in Israel 17) that involved 19 patients; 18 were male and 17 acknowledged their MSM status. The sole female case had recently travelled to India and the genetic testing revealed a typically Indian, non-European strain. The mean age was 48.5 years. Subtypes were analyzed in 14 patients, eight were strain 2 as reported in Europe and six were strain 1. A total of three patients had recently travelled to Europe. New cases have also been reported in Berlin 18. As of January 20th 2017, 38 new cases of hepatitis A had been reported since November 2016. Of these, 37 were male and one, female. Sexual orientation was known in 32 cases (31 males, one female). Of these, 30 males were MSMs. With regard to the cases reported in Munich and Frankfurt, a strain different from the two reported European types (sequence V16-25801) was found. Approximately one third of the males diagnosed in Berlin said they visited sexual encounter venues, had not been vaccinated or had received only one dose of vaccine.
Our findings stress the importance of offering the hepatitis A vaccine to those MSMs with high-risk sexual behavior, in addition to specifically oriented informative campaigns about the need to prevent sexually transmitted diseases (STDs) and to reinforce epidemiologic surveillance in Europe due to the ability of pathogens to easily spread across frontiers.
BIBLIOGRAFÍA
1. Høybye G, Skinhøj P, Hentzer B, et al. An epidemic of acute viral hepatitis in male homosexuals. Etiology and clinical characteristics. Scand J Infect Dis 1980;12(4):241-4. DOI: 10.3109/inf.1980.12.issue-4.01 [ Links ]
2. Tortajada C, De Olalla PG, Díez E, et al. Hepatitis A among men who have sex with men in Barcelona, 1989-2010: insufficient control and need for new approaches. BMC Infect Dis 2012;12:11. DOI: 10.1186/1471-2334-12-11 [ Links ]
3. Tortajada C, De Olalla PG, Pinto RM, et al. Outbreak of hepatitis A among men who have sex with men in Barcelona, Spain, September 2008-March 2009. Euro Surveill 2009;14(15). [ Links ]
4. Llach-Berné M, Pañella H, Domínguez A, et al. Descriptive study of hepatitis outbreaks occurring in Catalonia (1999-2003). Enferm Infecc Microbiol Clin 2006;24(7):431-6. DOI: 10.1157/13091780 [ Links ]
5. Beebeejaun K, Degala S, Balogun K, et al. Outbreak of hepatitis A associated with men who have sex with men (MSM), England, July 2016 to January 2017. Euro Surveill 2017;22(5). DOI: 10.2807/1560-7917.ES.2017.22.5.30454 [ Links ]
6. ECDC. European Centre for Disease Prevention and Control. Hepatitis A virus in the EU/EEA. Stockholm; 2016. pp. 1975-2014. [ Links ]
7. Nainan OV, Xia G, Vaughan G, et al. Diagnosis of hepatitis a virus infection: a molecular approach. Clin Microbiol Rev 2006;19(1):63-79. DOI: 10.1128/CMR.19.1.63-79.2006 [ Links ]
8. Plotkin S, Orenstein W, Offit P. Hepatitis A vaccines. Vaccines. 6th ed. Elsevier; 2012. pp. 183-205. [ Links ]
9. WHO. Hepatitis A outbreaks mostly affecting men who have sex with men - European Region and the Americas. 2017. Accessed on December 29, 2017. Available from: http://www.who.int/csr/don/07-june-2017-hepatitis-a/en/ [ Links ]
10. ECDC. European Centre for Disease Prevention and Control. Hepatitis A outbreaks in the EU/EEA mostly affecting men who have sex with men. Stockholm; 2017. [ Links ]
11. Freidl GS, Sonder GJ, Bovée LP, et al. Hepatitis A outbreak among men who have sex with men (MSM) predominantly linked with the EuroPride, the Netherlands, July 2016 to February 2017. Euro Surveill 2017;22(8). DOI: 10.2807/1560-7917.ES.2017.22.8.30468 [ Links ]
12. Gullón P, Varela C, Martínez EV, et al. Association between meteorological factors and hepatitis A in Spain 2010-2014. Environ Int 2017;102:230-5. DOI: 10.1016/j.envint.2017.03.008 [ Links ]
13. Wang Z, Chen Y, Xie S, et al. Changing epidemiological characteristics of hepatitis A in Zhejiang Province, China: increased susceptibility in adults. PLoS One 2016;11(4):e0153804. DOI: 10.1371/journal.pone. 0153804 [ Links ]
14. Chen CM, Chen SC, Yang HY, et al. Hospitalization and mortality due to hepatitis A in Taiwan: a 15-year nationwide cohort study. J Viral Hepat 2016;23(11):940-5. DOI: 10.1111/jvh.12564 [ Links ]
15. Chen GJ, Lin KY, Sun HY, et al. Incidence of acute hepatitis A among HIV-positive patients during an outbreak among MSM in Taiwan: impact of HAV vaccination. Liver Int 2017. DOI: 10.1111/liv.13468 [ Links ]
16. Chen GJ, Lin KY, Hung CC, et al. Hepatitis A outbreak among men who have sex with men in a country of low endemicity of hepatitis A infection. J Infect Dis 2017;215(8):1339-40. DOI: 10.1093/infdis/jix123 [ Links ]
17. Gozlan Y, Bar-Or I, Rakovsky A, et al. Ongoing hepatitis A among men who have sex with men (MSM) linked to outbreaks in Europe in Tel Aviv area, Israel, December 2016-June 2017. Euro Surveill 2017;22(29). DOI: 10.2807/1560-7917.ES.2017.22.29.30575 [ Links ]
18. Werber D, Michaelis K, Hausner M, et al. Ongoing outbreaks of hepatitis A among men who have sex with men (MSM), Berlin, November 2016 to January 2017 - Linked to other German cities and European countries. Euro Surveill 2017;22(5). DOI: 10.2807/1560-7917.ES.2017.22.5.30457 [ Links ]
Received: August 24, 2017; Accepted: January 05, 2018











 text in
text in