My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.6 Madrid Jun. 2018
https://dx.doi.org/10.17235/reed.2018.5370/2017
PICTURES IN PATOLOGY DIGESTIVE
Hepatic encephalopathy secondary to a splenorenal shunt that manifested a long time after a liver transplantation
1Departamentos de Aparato Digestivo. Hospital Universitario Virgen de la Arrixaca. El Palmar, Murcia, Spain
2Departamentos de Radiodiagnóstico. Hospital Universitario Virgen de la Arrixaca. El Palmar, Murcia, Spain
CASE REPORT
A 79-year-old female had undergone a liver transplantation in 2002 due to cryptogenetic cirrhosis and suffered no post-transplant complications. In January 2016, the immunosuppressive therapy was successfully withdrawn. The initial symptoms included bradypsychia, somnolence and behavior alterations. The serum ammonia levels were 94 μg/dl and the remaining blood test were normal. Treatment with lactulose enemas was started, which resulted in a partial improvement of the symptoms. The thyroid hormones, vitamin B12 and folic acid analyses were normal.
A doppler ultrasonography, a brain magnetic resonance scan, an electroencephalogram and a liver biopsy were normal. The patient was evaluated by the neurologist and a neurological-origin pathology was ruled out. Computed tomography (CT) identified two venous branches that created a splenorenal shunt (Fig. 1 and Fig. 2) and the portal vein was permeable. A shunt embolization using coils + ethoxystyrenol foam was performed due to these findings with a good outcome (Fig. 3). The patient was asymptomatic after this procedure and has not experienced a new hepatic encephalopathy episode.
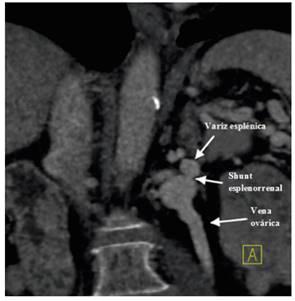
Fig. 1 CT examination with intravenous contrast in the venous phase. Coronal view showing a splenorenal shunt.
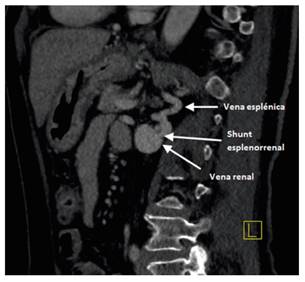
Fig. 2 CT examination with intravenous contrast in the venous phase. Sagittal image showing another venous branch that created the splenorenal shunt.
DISCUSSION
Splenorenal shunts usually occur in patients with chronic liver disease and portal hypertension and rarely occur in non-cirrhotic patients 1. Nowadays, interventional radiology techniques based on embolization with metal micro-coils, or the use of balloons in shunt occlusion and injecting sclerosing substances are frequently used 3.
After a review of the literature, only two cases of hepatic encephalopathy secondary to splenorenal shunt were found, in the absence of cirrhosis that manifested a long time after the liver transplantation. Both cases were resolved by vascular radiology 2,3. There was no evidence of a splenorenal shunt at the time of surgery in the current case and it was not documented during the imaging tests prior to liver transplantation.
BIBLIOGRAFÍA
1. Rogal S, Hu A, Bandi R, et al. Novel therapy for non-cirrhotic hyperammonemia due to a spontaneous splenorenal shunt. World J Gastroenterol 2014;20(25):8288-91. DOI: 10.3748/wjg.v20.i25.8288 [ Links ]
2. Braun M, Bar-Nathan N, Shaharabani E, et al. Postshunt hepatic encephalopathy in liver transplant recipients. Transplantation 2009;87(5):734-9. DOI: 10.1097/TP.0b013e318196340d [ Links ]
3. Crespo L, Graus J, García-Hoz F, et al. Hepatic encephalopathy secondary to porto-systemic shunt satisfactorily treated with interventionist radiology. Rev Esp Enferm Dig 2007;99(11):667-70. DOI: 10.4321/S1130-01082007001100010 [ Links ]











 text in
text in 


