My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.8 Madrid Aug. 2018
https://dx.doi.org/10.17235/reed.2018.5571/2018
LETTERS
Ileal tubular adenoma as a cause of lower gastrointestinal bleedingin infants
1Servicio de Gastroenterología. Centro de Enfermedades Hepáticas y Digestivas CEHYD. Bogotá, Colombia
2Servicio de Gastroenterología. Hospital Italiano de Buenos Aires. Buenos Aires, Argentina
3Unidad de Endoscopia Digestiva. Instituto de Gastroenterología Boliviano Japonés. La Paz, Bolivia
Key words: Lower gastrointestinal bleeding; Adenomatous polyp; Endoscopic excision; Infant
Dear Editor,
Lower gastrointestinal bleeding is a common pathology with diverse causes depending on the patients' age. The most common causes in adults are polyps, neoplasias, diverticular disease and angiodysplasia; in neonates, necrotizing enterocolitis and volvulus; and anal fissures and bowel intussusception in infants. Polyps are reported as a cause of bleeding only in children of preschool age 1.
Case report
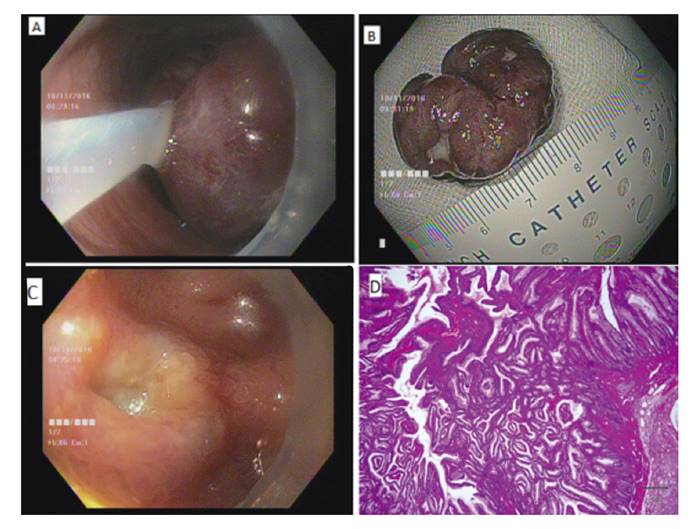
The patient was a 12-month old female with asthenia, pale skin and vomiting of a two week duration. The blood analysis was as follows: hemoglobin, 4 g/dl; hematocrit, 12.3%; and serum iron, 36 µg/dl (normal: 35-145 µg/dl). The white blood cell count and platelet count were normal. Transfusion of packed red blood cells was indicated, based on a diagnosis of hypochromic microcytic anemia. The patient had two hematochezia episodes when hospitalized and therefore, underwent a colonoscopy. A polypoidal and ulcerated mass with no active bleeding was observed in the ileum, which involved 80% of the gut lumen (Fig. 1A). A polypectomy was performed and the polyp was retrieved for histopathological study (Fig. 1B and Fig. 1C). The patient was discharged, and had an adequate evolution and no new bleeding episodes. The histopathological study identified an eroded polyp that measured 3.5 x 2.5 x 2.0 cm, covered in blood, with a thin and short implantation pedicle. The diagnosis was an inflamed tubular adenoma (Fig. 1D).
Discussion
Polyps are infrequent in children and may present as an isolated tumor or as polyposis syndrome. They are located in the colon and manifest as a bowel obstruction that requires surgery 2,3. Capsule endoscopy is a diagnostic alternative that can be used even in infants 4. Distal ileum must always be evaluated during endoscopy and endoscopic excision is feasible despite the polyp size.
Bibliografía
1. Pant C, Sankararaman S, Deshpande A, et al. Gastrointestinal bleeding in hospitalized children in the United States. Curr Med Res Opin 2014;30(6):1065-9. DOI: 10.1185/03007995.2014.887003 [ Links ]
2. Attard TM, Cuffari C, Tajouri T, et al. Multicenter experience with upper gastrointestinal polyps in pediatric patients with familial adenomatous polyposis. Am J Gastroenterol 2004;99(4):681-6. DOI:10.1111/j.1572-0241.2004.04115x [ Links ]
3. Wang L, Lee H, Yeung Ch, et al. Gastrointestinal polyps in children. Pediatr Neonatol 2009;50(5):196-201. DOI: 10.1016/S1875-9572(09)60063-2 [ Links ]
4. Argüelles-Arias F, Donat E, Fernández-Urien I, et al. Guideline for wireless capsule endoscopy in children and adolescents: a consensus document by the SEGHNP (Spanish Society for Pediatric Gastroenterology, Hepatology, and Nutrition) and the SEPD (Spanish Society for Digestive Diseases). Rev Esp Enferm Dig 2015;107(12):714-31. DOI: 10.17235/reed.2015.3921/2015 [ Links ]











 text in
text in