My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.9 Madrid Sep. 2018
https://dx.doi.org/10.17235/reed.2018.5419/2017
ORIGINAL PAPERS
Efficacy and safety of transoral outlet reduction via endoscopic suturing in patients with weight regain after a surgical Roux-en-Y gastric bypass
1Unidad de Tratamiento Endoscópico de la Obesidad. Hospital Universitario Dexeus. Barcelona, Spain
1Endosmedicina. Clínica Diagonal. Barcelona, Spain
1Departamento de Endoscopia Bariátrica. Hospital Universitario Madrid Sanchinarro. Madrid Spain
INTRODUCTION
The World Health Organization (WHO) defines being overweight and obesity as an abnormal or excessive accumulation of fat that can be harmful to health, with a considerable associated morbidity and mortality 1. The rising prevalence of obesity and its associated metabolic diseases have led to a marked increase in the number and type of bariatric procedures. Today, bariatric surgery remains the most effective long-term therapeutic option for patients with morbid obesity. Furthermore, RYGB remains the predominant bariatric surgical procedure, which results in an average excess weight loss (% EWL) in the range of 65-80% after 2-3 years 2,3. However, after the initial weight loss many patients can regain weight, either partial or total. One study reported an average weight regain of 18 kg after two years 4; at ten years post-RYGB, the average weight regain was reported to be over 30% of the weight initially lost and over 25% of patients regained almost all the weight lost 5,6.
Etiologies and mechanisms for weight regain are not fully understood and the process is likely multifactorial. This has been related to preoperative factors (previous body mass index [BMI] and genetic factors), endocrine-metabolic factors (patient dietary adherence or neuroendocrine-metabolic dysregulation) or mechanic factors (type of surgery, gastro-gastric fistula or enlargement of the gastric pouch) 7,8. Recently, a positive linear association between the size of the gastro-jejunal anastomosis (GJA) and weight regain has been reported. A GJA diameter > 15 mm was proposed as a cut-off for dilated GJA 9.
Weight regain treatment may be surgical or endoscopic. Surgical revisions include the recreation of the gastro-jejunostomy, reduction of a gastric pouch, placement of an adjustable gastric band, taking down the Roux limb and distal gastric bypass. Although effective, surgical techniques have a high complication rate of up to 50%. The mortality rates are 2%, which is more than double that of the original procedure. Furthermore, there are high costs and many patients do not wish to undergo surgery 10,11. Therefore, less-invasive, endoscopic revision methods can have an enormous potential in these patients. To date, sclerotherapy techniques and different experimental models of gastric sutures have been used 12,13,14,15.
This is the first Spanish series published using the full-thickness endoscopic suture system, OverStitch(r) (Apollo Endosurgery, Austin, Texas, USA), for this condition. The study includes a retrospective descriptive review of our initial experience on the technical feasibility, safety and early efficacy of the endoscopic transoral outlet reduction (TORe) procedure in patients with weight regain after a RYGB and a short-term follow-up. Plications were applied around the GJA to reduce the aperture and also in the gastric pouch to provide further size reductions. The patients were followed-up for six months.
PATIENTS AND METHODS
Consecutive patients submitted to a TORe evaluation from June 2014 to June 2016 with weight regain after RYGB were included in the study. The time interval between RYGB and endoscopic re-intervention was eleven years (range 3-16). All gastro-jejunal anastomosis (GJA) were performed with mechanical sutures; they were dilated with a diameter of > 15 mm. Patients with a GJA of < 15 mm and cases that underwent suturing procedures for a gastro-gastric fistula or marginal ulceration were excluded from the study. The procedures were performed by three endoscopists at the Dexeus University Hospital in Barcelona and at the Hospital Universitario Sanchinarro in Madrid, Spain.
TORe was performed using the OverStitch(r) Endoscopic Suturing System (Apollo Endosurgery, Austin, Texas, USA), which attaches to a double-channel Olympus gastroscope (GIF-2T160, Olympus America, Central Valley, Penn, USA) that is passed through a specific overtube, 25 cm in length. TORe was performed under general anesthesia with endotracheal intubation controlled by an anesthesiologist, with antibiotics and proton pump inhibitors (PPIs) prophylaxis. The procedure was performed by three endoscopists with prior experience in advanced suturing methods (e.g., endoscopic sleeve gastroplasty) using the same endoluminal suturing system. However, they had no previous experience in stoma reduction; a standard gastroscopy was first completed to discard contraindications and to measure the diameter of the anastomosis and the pouch. These were measured using a polipectomy handle or a balloon (anastomosis) and distance from the incisors to the anastomosis and Z-line (pouch). Tissue at the rim of the anastomosis was ablated circumferentially using argon-plasma coagulation at a setting of 60 W and a flow rate of 1.6 l/min, in order to improve the narrowing of the lumen by healing and strengthening the fusion of the sutured edges. Interrupted transmural stitches were placed in the anastomosis from right to left until reaching a diameter < 12 mm. Patients with a dilated pouch (greater than 5 cm in length) also underwent a suture and reduction, beginning at the distal region until reaching a size of < 5 cm.
After the procedure, the patients remained in observation for a few hours and were discharged on the same day if there were no clinically apparent adverse events. Each patient was managed by the endoscopist for the first week. Patients were then followed by a nutritionist, who initially established a regimen based on a liquid diet during the first two weeks, followed by soft intake for another two weeks. From day 30 to six months, a standard hypocaloric diet was followed, which is used for other obese patients. Furthermore, the nutritionist used the same dietary guidelines as those established before TORe. Therefore, the endoscopic procedure could be considered as the only variant and modification related to weight changes. PPIs were maintained for one month and clinical follow-up was performed at one, three and six months.
The study was approved by the Ethics Committee of the Hospital, all details of the technique were explained to all patients and they gave their written informed consent for the procedure and follow-up.
RESULTS
A total of 13 patients (8 females) were included in the study. The mean patient age was 50 years (range 39-66). The average interval between RYGB and TORe was eleven years (range 3-16), with a mean maximum weight loss post-RYGB of 37.69 kg and a subsequent mean weight regain of 21.62 kg (Table 1). At the time of the TORe, the patients had an average weight of 98.48 kg (range 80.00-131.80), which was equivalent to a mean excess weight of 35.03 kg (55.69% of excess weight) and a mean BMI of 37.33 kg/m² (range 30.12-45.60) (Table 2).
Table 1 Clinical characteristics related to RYGB
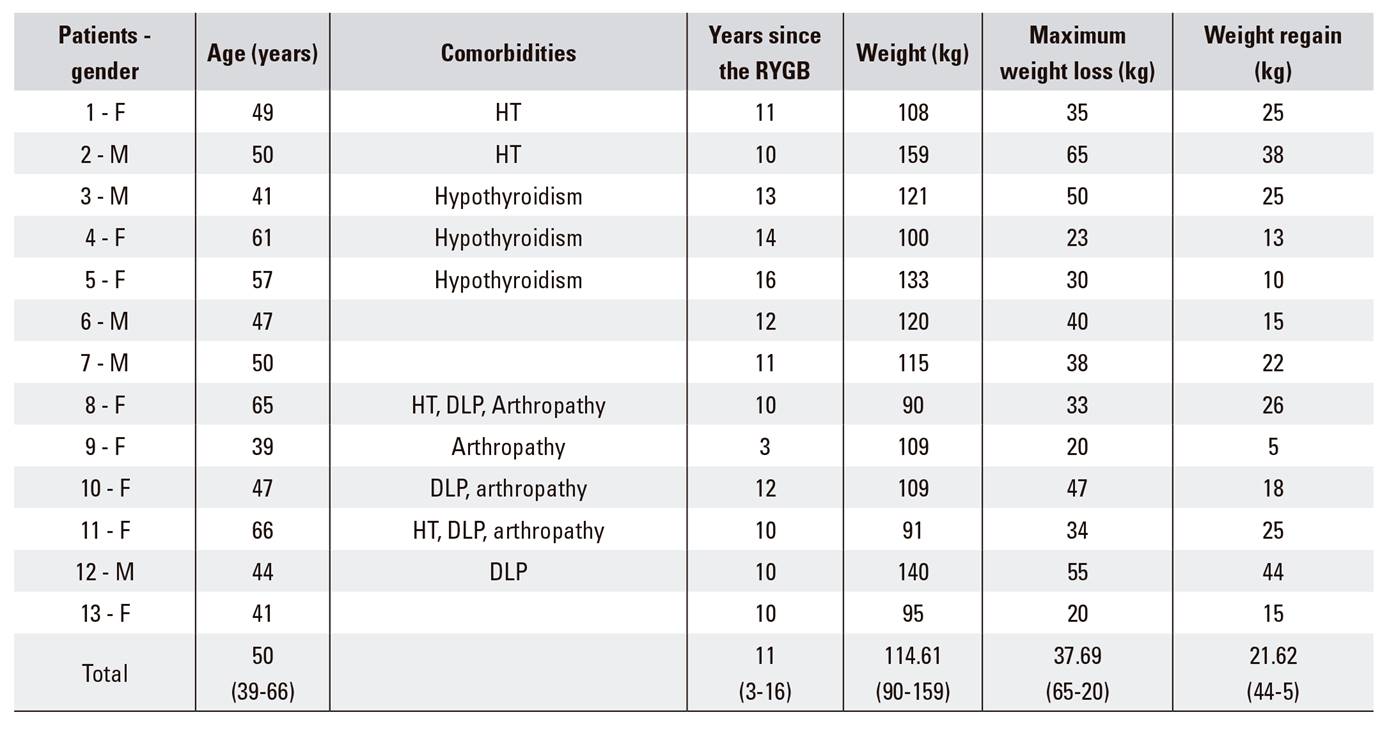
M: male; F: female; HT: arterial hypertension; DLP: dyslipidemia.
Table 2 Efficacy of TORe
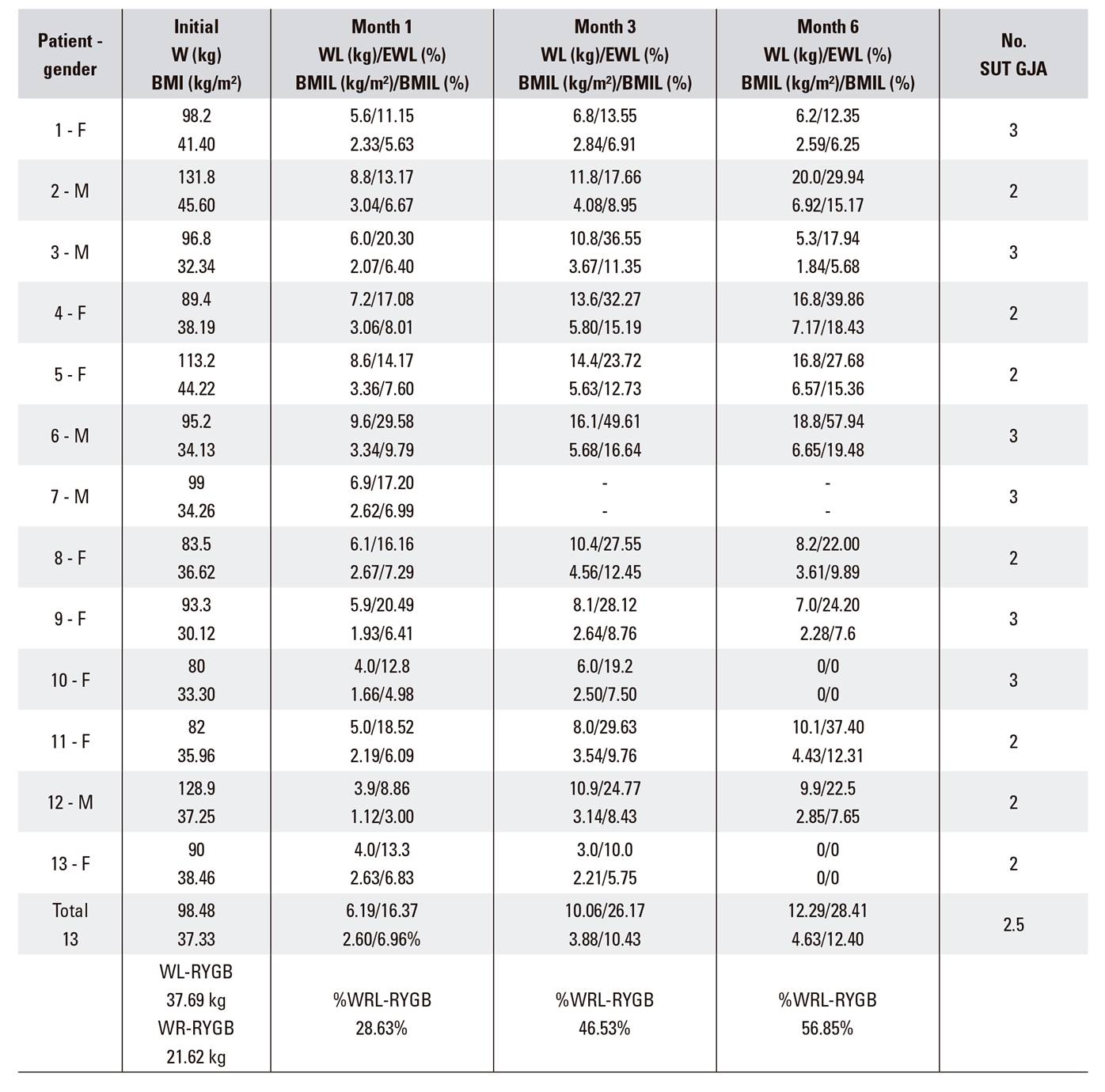
M: male; F: female; W: weight; WL: weight loss; EWL: excess weight loss; BMIL: BMI loss; No. SUT-GJA: number of sutures in the gastro-jejunal anastomosis; WL-RYGB: weight loss post-RYGB; WR-RYGB: Weight regained post-RYGB; %WRL-RYGB: % of weight lost regained post-RYGB.
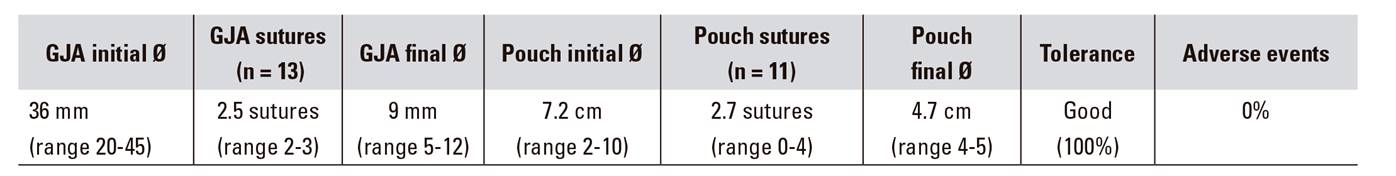
The average diameter of the GJA was 36 mm (range 20-45). After preparing the anastomosis with argon plasma coagulation, an average of 2.5 sutures were used (range 2-3). This reduced the anastomosis to a mean diameter of 9 mm (range 5-12), which resulted in an average reduction of 27 mm (75% reduction) (Table 3). A final diameter of less than 12 mm was obtained in all cases. There was one case of weight gain with a re-dilation of the stoma (from 10 to 20 mm after 12 months), which was successfully reduced to 9 mm without any incidents. The average size of the pouch was 7.2 cm (range 2-10) and was dilated in 11/13 patients. An average of 2.7 plications were created (range 0-4), reducing the mean length to 4.7cm (range 4-5). This resulted in an average decrease of 2.5 cm (34.72% reduction) (Table 3).
The average procedure time was 50 minutes (range 120-25 minutes). The most durable were the first cases and those that also required a joint stoma and pouch suture. The shorter ones required only the stoma suture. There were no complications related with the procedure and TORe was well tolerated in all cases. One patient had an intra-procedural self-limited bleed from a needle puncture site. Epigastric pain was common for the first 48 hours. Nausea was experienced in two patients during the first 24 hours. All were treated conservatively and were discharged on the same day of the intervention; there were no delayed adverse events during follow-up.
Follow-up data were available for 12/13 patients at one, three and six months. There was an average weight loss of 6.19, 10.06 and 12.29 kg, respectively, which represents a EWL of 16.37, 26.17 and 28.41% and an average BMI loss percentage of 6.96, 10.43 and 12.40%, respectively. These results demonstrate a loss of 28.63, 46.53 and 56.85% of post-RYGB weight regained (Table 2). The weight loss at six months in the eleven patients treated simultaneously for a GJA and gastric pouch (12.8 kg, 29.52% EWL) was somewhat higher compared to the two cases treated only for a stoma (11.3 kg, 26.60% EWL). However, the difference was not statistically significant.
DISCUSSION
RYGB represents the most effective treatment for morbid obesity and its co-morbidities 2,3. Nevertheless, many patients tend to regain weight over time 4,5,6. Surgical revision is one option, although it has a higher rate of morbidity and mortality than the primary surgery 10,11. For this reason, there is an increasing interest in less invasive techniques, especially endoluminal 12,13,14,15.
In this study, we describe our initial experience of the technical feasibility and weight changes that resulted from the transoral outlet reduction (TORe) in patients with weight regain after RYGB and with a dilated GJA. Our patient cohort had an average weight regain after RYGB of 21.62 kg, and the data in the literature varies and oscillates in some studies between 13-23 kg 16,17 or 52.6% of the lost weight 18. Dilated GJA was defined as an anastomosis diameter of > 15 mm 9. The success of the technique was defined as its reduction to < 12 mm, which was achieved in all cases. These results are similar to those described previously. A rate of 94.9% was described by Changella et al. 16 and one of 100% by Jirapinyo et al. 18. In addition, when the gastric pouch was dilated with a measured length of > 5 cm, this was thought to require a reduction as an adjunct to the anastomosis reduction in the same endoscopic procedure. Combined stoma and pouch treatment is scarcely documented in the literature 15,19.
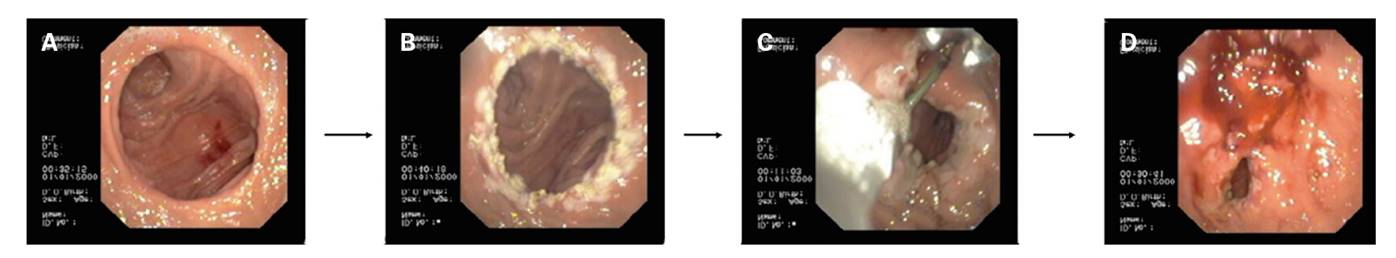
Fig. 1 The TORe procedure. A. Dilated stoma. B. Circular treatment with argon. C. Reduction of the diameter with an OverStitch of Apollo. D. Reduced diameter, the final result.
We were able to decrease the mean diameter of the GJA from 36 to 9 mm (range 5-12), which represents a 75% reduction of the initial diameter. The final result can be compared to two published studies by Jirapinyo et al. and Kumar et al. 20,21, where the mean diameter was reduced to 6 and 6.9 mm. The review by Changela et al. 16 reported an average GJA reduction from 24.85 to 8 mm. One patient in our cohort required a second TORe due to a partial failure of the first procedure, due to weight regain and the GJA re-dilated after 12 months. We were able to successfully reduce the stoma in the second TORe, which supports the possibility of sequential treatments with this system. In this sense, Kumar et al. have estimated that the number of sessions required to stop weight regain was 1.0 at six months, 1.1 at one year and 1.2 at two and three years. The number of sessions required to maintain a weight loss of > 5 kg from TORe was 1.2 at six months, 1.5 at one year, 1.9 at two years and 2.0 at three years 21.
No major adverse events were reported in our study; three intra-procedural events were described in 25 patients in the first series published using a first generation suturing device 22. These included one small esophageal abrasion from the overtube treated with fibrin glue and two patients with arterial bleeding that was stopped by over-sewing. There were also six post-procedural events; two hemorrhages and four cases of major vomiting, two with torn sutures and a GJA stenosis in another case that required endoscopic balloon dilation. In subsequent series, the procedure was a safe and reliable intervention with few complications, and there were only some isolated cases of bleeding and stenosis 16,17,18,19,20,21.
In our study, all procedures were performed with general anesthesia with endotracheal intubation. Prophylaxis with PPIs and intra-procedural antibiotics were systematically provided due to the placement of transmural sutures. The safety, good tolerance and short duration of the procedure (less than other series; an average of 74 minutes was reported by Changela et al. 16)) allowed us to perform the procedures in the endoscopic room with a same day discharge (outpatient procedure).
The patients were under the care of the endoscopist the first week after the procedure and subsequently, of a dietician. In our opinion, the post-procedure management plan used in this study was effective. From 30 days after TORe and up to six months later, the dietary guidelines used by the dietician were similar to those established before TORe and also standardized for all obese patients. No specific diet was established for these patients, thus the endoscopic procedure was the only factor that could affect weight changes at three and six months of follow-up. In the same way, a randomized multicenter clinical trial also concluded that the weight loss efficacy of patients that underwent TORe was greater than that of the control group 22.
With regard to efficacy, an average weight loss of 10.06 kg at three months was obtained. These results are similar to four studies and a review of 59 patients which obtained a 10.1 kg weight loss 16. At six months, the weight loss was 12.29 kg (28.41% EWL); this data is similar to that published by Jirapinyo et al. (11.7 kg) 20 and somewhat better than the study by Gitelis et al. (5.6 kg, 12.4% EWL) 17. This may be due to our follow-up care program, a somewhat lower initial BMI or a gastric pouch reduction in most of our patients. Kumar et al. 21 performed the longest series published to date and reported an average weight loss of 10.5-9.0-9.5 kg (24.9-20.0-19.2% EWL) at one, two and three years, respectively. Jirapinyo et al. 18 observed a total weight loss of 9.6% and 8.4% at six and 12 months, respectively. In addition, the technique also seems to improve metabolic diseases 18,22, although this was not evaluated in our study. In our series, two patients had no weight loss after six months of follow-up (patients 10 and 13) (Table 2). Both patients did not adhere to the dietary instructions and neither made any additional lifestyle changes. The patient that was lost to follow-up had changed their care to another hospital (patient 7).
With regard to the eleven patients treated simultaneously with a GJA and pouch, the weight loss was somewhat higher in the two cases treated only for the stoma. However, the difference was not statistically significant. Schulman et al. 19 compared the TORe (traditional pattern of simple sutures) with the purse-string, and no significant differences in weight loss after six months were identified. However, they concluded that although TORe is effective, the purse-string technique results in a greater weight loss than the traditional interrupted suture pattern 12 months after the procedure.
The study presents several limitations, such as the retrospective descriptive design, the absence of a control group (only the weight changes before and after the procedure are described), the small sample size of 13 patients, the short follow-up time period of six months, the lack of prior experience with this technique and the fact that only two centers participated in the study. We did not assess the effect of the procedure on the metabolic syndrome. Endoscopic follow-up was not systematically performed to confirm the diameter of the GJA or the pouch, since the study was not a sponsored clinical trial.
Although the results are quite similar to the few published reports in the literature, future randomized interventional studies with a greater number of patients and longer follow-up will be necessary to confirm our results. From a technical point of view, it will be necessary to define improvements in the device, the endoscopic technique, the suture pattern and the location of the stitches. Based on our short experience, we feel that there is a need to complement the reduction of the diameter of the GJA with the reduction of the gastric pouch when it is dilated.
In summary, the results of this preliminary descriptive case series suggest that TORe with the OverStitch Endoscopic Suturing System could be a feasible and safe procedure for the management of weight regain after RYGB. The reduction of the GJA seems to offer good weight loss results in the short term, especially if it is complemented with a gastric pouch reduction and supported with a regimented dietary and nutritional control. These initial results of feasibility, efficacy and safety should be confirmed in future randomized clinical trials.
ACKNOWLEDGMENTS
This study lacks any kind of help, scholarship or funding.
This manuscript has been reviewed by Dr. Christopher J. Gostout, M.D. The authors thank him for his altruistic effort and dedication.
REFERENCES
1. Organización Mundial de la Salud. Obesidad y sobrepeso. Nota descriptiva nº 311. Septiembre 2006. [ Links ]
2. Higa KD, Ho T, Boone KB. Laparoscopic Roux-en-Y gastric by-pass: technique and 3-years follow-up. J Laparoendosc Adv Surg Tech 2011;11:377-82. DOI: 10.1089/10926420152761905 [ Links ]
3. Buchwald H, Avidor Y, Braunwalkd E, et al. Bariatric surgery: a systemic review and meta-analysis. JAMA 2004;292:1724-37. DOI: 10.1001/jama.292.14.1724 [ Links ]
4. Powers PS, Rosemurgy A, Boyd F, et al. Outcome of gastric restriction procedures: weight, psychiatric diagnoses, and satisfaction. Obes Surg 1997;7:471-7. DOI: 10.1381/096089297765555197 [ Links ]
5. Christou N, Look D, Maclean L. Weight gain after short- and long-limb gastric bypass in patients followed for more than 10 years. Ann Surg 2006;244:734-40. DOI: 10.1097/01.sla.0000217592.04061.d5 [ Links ]
6. Sjostrom L, Lindroos A, Peltonem M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004;351:2683-93. DOI: 10.1056/NEJMoa035622 [ Links ]
7. Peruginin RA, Mason R, Czerniach DR, et al. Predictors of complication and suboptimal weight loss after laparoscopic Roux-en-Y bypass: a series of 188 patients. Arch Surg 2003;138:541-5. DOI: 10.1001/archsurg.138.5.541 [ Links ]
8. Odom J, Zalesin KC, Washington TL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg 2010;20:349-56. DOI: 10.1007/s11695-009-9895-6 [ Links ]
9. Abu Dayyeh BK, Lautz DB, Thompson CC. Gastrojejunal stoma diameter predicts weight regain after Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol 2011;9:228-33. DOI: 10.1016/j.cgh.2010.11.004 [ Links ]
10. Schwartz R, Strodel W, Simpson W, et al. Gastric bypass revision: lessons learned from 920 cases. Surgery 1988;104:806-12. [ Links ]
11. Gumbs AA, Pomp A, Gagner M. Revisional bariatric surgery for inadequate weight loss. Obes Surg 2007;17:1137-45. DOI: 10.1007/s11695-007-9209-9 [ Links ]
12. Catalano MF, Rudic G, Anderson AJ, et al. Weight gain after bariatric surgery as result of a large gastric stoma: endotherapy with sodium morrhuate may prevent the need for surgical revision. Gastrointest Endosc 2007;66:240-5. DOI: 10.1016/j.gie.2006.06.061 [ Links ]
13. Abu Dayyeh BK, Jirapinyo P, Weitzner Z, et al. Endoscopic sclerotherapy for the treatment of weight regain after Roux-en-Y gastric bypass: outcomes, complications, and predictors of response in 575 procedures. Gastrointest Endosc 2012;76:275-82. DOI: 10.1016/j.gie.2012.03.1407 [ Links ]
14. Mikami D, Needleman B, Narula V, et al. Natural orifice surgery: initial US experience utilizing the StomaphyX device to reduce gastric pouches after Roux-en-Y gastric bypass. Surg Endo 2010;24:223-8. DOI: 10.1007/s00464-009-0640-y [ Links ]
15. Horgan S, Jacobsen G, Weiss DG, et al. Incisionless revision of post-Roux-en-Y bypass stomal and pouch dilation: multicenter registry results. Surg Obes Relat Dis 2010;2:290-5. DOI: 10.1016/j.soard.2009.12.011 [ Links ]
16. Changela K, Ofori E, Duddempudi S, et al. Peroral endoscopic reduction of dilated gastrojejunal anastomosis after bariatric surgery: techniques and efficacy. World J Gastrointest Endosc 2016;8(4):239-43. DOI: 10.4253/wjge.v8.i4.239 [ Links ]
17. Gitelis M, Ujiki M, Farwell L, et al. Six month outcomes in patients experiencing weight gain after gastric bypass who underwent gastrojejunal revision using an endoluminal suturing device. Surg Endosc 2015;29(8):2133-40. DOI: 10.1007/s00464-014-3954-3 [ Links ]
18. Jirapinyo P, Kröner PT, Thompson CC. Purse-string transoral outlet reduction (TORe) is effective at inducing weight loss and improvement in metabolic comorbidities after Roux-en-Y gastric bypass. Endoscopy 2018;50(4):371-7. DOI: 10.1055/s-0043-122380 [ Links ]
19. Schulman AR, Kumar N, Thompson CC. Transoral outlet reduction: a comparison of purse-string with interrupted stitch technique. Gastrointest Endosc 2018;87(5):1222-8. DOI: 10.1016/j.gie.2017.10.034 [ Links ]
20. Jirapinyo P, Slattery J, Ryan MB, et al. Evaluation of an endoscopic suturing device for transoral outlet reduction in patients with weight regain following Roux-en-Y gastric bypass. Endoscopy 2013;45(7):532-6. DOI: 10.1055/s-0032-1326638 [ Links ]
21. Kumar N, Thompson CC. Transoral outlet reduction for weight regain after gastric bypass: long-term follow-up. Gastrointest Endosc 2016;83(4):776-9. DOI: 10.1016/j.gie.2015.08.039 [ Links ]
22. Thompson CC, Chand B, Chen YK, et al. Endoscopic suturing for transoral outlet reduction increases weight loss after Roux-en-Y gastric bypass surgery. Gastroenterology 2013;145(1):129-37. DOI: 10.1053/j.gastro.2013.04.002 [ Links ]
Received: December 20, 2017; Accepted: February 25, 2018











 text in
text in