My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Cirugía Oral y Maxilofacial
On-line version ISSN 2173-9161Print version ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 n.4 Madrid Jul./Aug. 2007
ARTÍCULO CIENTÍFICO
Platelet-rich plasma quality: a study on platelet activation
Calidad del plasma rico en plaquetas: estudio de la activación plaquetaria
C. Sáez-Torres Barroso1, J. Calvo Benito1, A. Gayà Puig2
1 Médico.
2 Médico. Director del Banco de Tejidos de las Islas Baleares.
Fundació Banc de Sang i Teixits de les Illes Balears, España
ABSTRACT
Objective. Platelet
Rich Plasma (PRP) is an autologous preparation currently used in oral and
maxillofacial reconstructive surgery. Blood collection and preparation of
platelet concentrates may lead to platelet activation and the premature loss of
their granular load. In this study, we have analyzed the quality of the PRP
obtained from a small volume of whole blood through a double centrifugation
technique, so called "tube method".
Design. We obtained 50 ml
of whole blood from 45 patients and centrifuged at 200 g for 10 minutes. The
plasma and buffy-coat were collected and we then centrifuged at 700g for 15
minutes. The pellet was resuspended after discarding 2/3 of the plasma. The
platelet concentration, platelet activation and the functional response to
thrombin were analyzed in these samples.
Results. By using this method of
PRP preparation, we obtained a 364 ± 177% increase in platelet concentration in
comparison with whole blood levels. Platelet activation, measured by flow
cytometry analysis of CD62 expression, was of 2.7% in unprocessed blood and 3.6%
in fresh PRP. This figure increased to 16% in PRP samples after overnight
storage at room temperature. A percentage of 96% of platelets showed activation
in PRP samples after thrombin stimulation.
Conclusion. Our results show
that platelets contained in PRP concentrates obtained by this method are not
significantly activated. A good functional platelet reserve is preserved through
the procedure, since platelets maintained a satisfactory response to thrombin
after PRP preparation.
Key words: Bone regeneration; Platelet Rich Plasma; Platelet activation; CD62.
RESUMEN
Objetivo. El plasma rico en plaquetas (PRP) es utilizado de forma cada vez más frecuente en técnicas quirúrgicas de regeneración tisular. No obstante, el procesamiento de la sangre hasta obtener PRP puede desencadenar la activación prematura de las plaquetas y la pérdida de los factores bioactivos. En este trabajo estudiamos la calidad de los concentrados de plaquetas obtenidos siguiendo la técnica de doble centrifugación en tubo.
Método. Se someten 50 ml de sangre a una primera centrifugación a 200g 10 minutos, se recoge el
sobrenadante y se centrifuga a 700g 15 minutos. Posteriormente, tras eliminar
las 2/3 partes del plasma, se resuspenden las plaquetas y se analiza el grado de
enriquecimiento, el estado de activación y la reserva funcional de las
plaquetas.
Resultados. El enriquecimiento en plaquetas del
PRP fue de 364±177% (n=45) respecto de los niveles presentes en sangre total.
Mediante el estudio de la expresión de CD62 por citometría de flujo se
determinó el porcentaje de plaquetas activadas en las muestras de 8 donantes.
Mientras que en la sangre no procesada se detectó un 2,7% de plaquetas
activadas, tras la preparación del PRP éste era sólo de 3,6%, aumentando
hasta el 16% en el concentrado almacenado toda la noche a 22º C. Tras la
estimulación con trombina el porcentaje de plaquetas activadas fue de 96,2%.
Conclusión. Este protocolo de preparación
de PRP no produce una activación significativa de las plaquetas. La respuesta a
la estimulación con trombina de los concentrados indica un buen estado de
reserva plaquetaria.
Palabras clave: Regeneración ósea; Plasma rico en plaquetas; Activación plaquetaria; CD62.
Introduction
The investigation carried out in the field of bone regeneration is geared towards the formation of bone of greater quality at an earlier stage and, on occasions, of greater quantity. When defining the techniques and materials that can provide the best conditions for this process, a knowledge of the physiology behind bone repair is required. In this context a therapeutic arsenal is used that includes different types of grafts and the growth factors that are to be found in these grafts, which are used in platelet concentrations for local use, or as commercial preparations based on recombinant types.1-3
Platelet-rich plasma (PRP) consists in a platelet concentrate with an autologous origin that, when in contact with substances that activate the coagulation process, forms a fibrin mesh with a gelatinous consistency that contains different cellular elements (platelet gel). There is a two-fold interest in using platelet gel. On the one hand it provides great stability for filling a bone defect, as it acts as an excellent carrier of bone grafts, especially for bone chip grafts, and it offers the possibility of generating a fibrin mesh that can be sutured and that helps to maintain the stability of the graft. On the other hand, blood cells, especially PRP platelets, are a source of mediating substances that are able to accelerate or improve the regenerative processes.4,5 Among these substances, various growth factors stand out such as TGF-b, PDGF, VEGF, EGF and IGF. Various studies have shown the activity of these substances for stimulating angiogenesis, for the induction of chemotaxis, proliferation and differentiation of progenitor cells and in collagen synthesis.6-8
Ever since the description of the clinical application of PRP, various protocols have been used for obtaining this, depending on what it was needed for. In the initial work by Marx, PRP was obtained by means of aphaeresis techniques. 4 This type of processing, which was commonplace in transfusion platelets, achieves considerable concentration of volume, but it is limited because specific conditions are required of the extracting center and of the patient. As the indications for the use of PRP have been widened to regeneration techniques of small sized bone defects, which are habitual in the field of oral and maxillofacial surgery, the methods for obtaining this have become simplified, and they have been adapted to smaller quantities of peripheral blood extracted by venous puncture in small volume tubes.1,5,9,10,11 This blood is subjected to successive centrifugation that permits concentrating the platelets to the desired amount. In this way the concentrate is prepared with greater ease and speed, and at a lesser cost, with a minimum discomfort for the patient. Both procedures take into account a series of variables that can influence the quality and biological activity of the final product, which are not currently well defined. Among these variables the different centrifugation steps stand out, as these influence the concentration as well as the degree of platelet activation. It has been demonstrated that premature platelet activation carries a loss factor, and the platelets are eliminated or degraded before reaching the area that they should act upon.12, 13 Therefore, in order to guarantee optimal results when using PRP, it is necessary for the concentrates used to contain a suitable number of platelets and for these platelets to have been maintained until used in conditions that guarantee the preservation of their functional capacity.
The object of this study was to determine the quality of platelet-rich plasma obtained with the double centrifugation tube method. With this aim, we analyze cell concentration in the final product as well as in the activated state, and the functional reserve of the platelets contained in this PRP.
Material and method
Obtaining samples
For preparing each sample of PRP in the study, blood was obtained from a series of healthy voluntary donors as well as from the patients who were to undergo a surgical bone regeneration procedure. The total amount of blood extracted from each donor was 50 ml in 5 ml tubes that contained citrate as an anticoagulant (Venoject, TERUMO Europe, Leuven, Belgium). This blood was processed following the tube preparation method for PRP. The procedure contemplates first a slow centrifugation (200g X 10 mins) after which the supernatant plasma is removed together with the first mm layer of red and white blood cells, followed by a second centrifugation of greater intensity (700g X 15 mins) that permits separating a fraction of platelet-poor plasma (PPP) that corresponds to the upper portion, with a variable volume depending on the cell concentration in the final product that is desired, and the remaining fraction of plateletrich plasma (PRP).
The preparation of the samples was carried out in a laminar flow cabinet in order to avoid contamination. The cell count of the total blood sample and of the PRP was carried out automatically (Ac-T5 diff AL,Beckman Coulter, CA).
Flow cytometry technique for the analysis of
platelet activation
Staining with specific antibodies was carried out of the different study samples together with fluorochromes versus CD61 and CD62 molecules. CD61 is a molecule that is expressed normally on the surface of platelets and it allows specifying the platelet population. CD62 analysis (P-selectin) is an activation marker of these cell elements because this molecule, which is present in the · granules of the platelets, is expressed on their surfaces on being activated. Double staining was carried out and saturating concentrations of anti-CD61 conjugated with phycoerythrin (Caltag, Burlingame, CA) were added to the samples together with anti-CD62 conjugated with phycoerythrin (Caltag, Burlingame, CA), which was incubated in the dark for 20 minutes at 22ºC. After incubation, 1 ml of paraformaldehyde 1% solution was added to each tube.
The activation control was carried out by stimulating an aliquot of PRP that had previously been diluted at 1:10 in PBS with thrombin at a concentration of 1 U/ml final (Sigma Chemicals, St.Louis, MO), in the presence of 2 mM Gly-Pro-Arg-Pro (GPRP, Sigma Chemicals, St. Louis, MO). This peptide is an inhibitor of fibrin polymerization and of platelet aggregates that stops clot formation as the platelets are activated. After adding the activator to the samples, these were incubated at 37ºC for 15 minutes and the staining protocol mentioned was continued. The samples were finally analyzed in a FACScan flow cytometer (Becton Dickinson, San José, CA) using the Cell Quest program (Becton Dickinson, San José, CA). The degree of platelet activation was analyzed at different times: total blood before processing, just separated PRP, PRP kept for 24 hours at 22ºC, and PRP stimulated with thrombin.
Results
PRP repair and platelet count
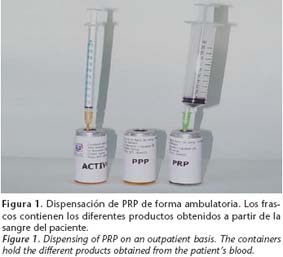
The laboratory-prepared PRP is dispensed to the clinician on an outpatient basis in sterile vials that contain the different fractions obtained from the patients blood. One vial contains platelet-rich plasma, another contains the fraction corresponding to the platelet-poor plasma, and a third contains the activating solution that consists in the patients very own serum enriched with calcium chloride with a final concentration of 2.3% (Fig. 1). For obtaining the platelet gel, only the PRP and the activating solution have to be recovered. This is done using graduated syringes and they are mixed at a 10:1 proportion (0.1 ml of activating solution to every ml of PRP).
Throughout the duration of this study, samples
from 45 patients were collected and a cell count was made of the whole blood and
of the PRP aliquot. The analysis of these samples revealed a platelet
concentration of 364 ± 177% in PRP with regard to the whole blood values.
Analysis of the degree of platelet activation
As has been discussed previously, platelet activation during the process for obtaining PRP, results in the release of growth factors towards the supernatant and as a result its early loss. Therefore, we consider studying this factor important as an influential parameter on the quality of PRP.
The degree of platelet activation was analyzed in the PRP samples of 8 donors at different times: whole blood, recently obtained PRP and PRP kept for 24 hours at 22ºC. For studying the state of the functional reserve of the platelets, activation was induced with thrombin of the concentrates.
The samples were read on the flow cytometer using a logarithm amplification signal of the four parameters (size, roughness, FL1, FL2) that control the acquisition. The region corresponding to the platelet population was delimited for later analysis, according to the size and roughness characteristics (Fig. 2A). The expression of the CD61 marker in more than 95% of the cells selected confirmed that the population included was composed essentially by platelets (Fig. 2B).
Once the platelet population had been analyzed, CD62 expression was then analyzed. The fluorescence pattern observed allows us to identify the percentage of platelets that show an intensity of the F12 expression marker above the control level of the technique, and that results in the activation state. Figure 3 shows the different fluorescence patterns that are observed depending on if the platelets are resting or active. In recently prepared PRP (Fig. 3A) and at 24 hours (Fig. 3B), the number of activated platelets is scarce. This situation is in contrast with the significant increase in the intensity of the FL2 signal in the samples stimulated with thrombin (Fig. 3C).
The analysis as a whole of all the samples generated from the same donor is represented in figure 4. The histogram shows the curves corresponding to the activation of platelets in peripheral blood, fresh PRP and PRP at 24 hours that are practically superimposed. The graft also reflects the significant increase in the expression of the platelet activation marker in response to thrombin stimulation.
The mean percentage of activated platelets
present in each sample, calculated from the analysis of 8 donors is represented
in figure 5. The percentage in platelets with CD62 expression in peripheral
blood before being processed was 2,7 ± 3,0%. After the centrifugation processes,
in the fresh PRP, the mean was 3,6 ± 2,7%. At this point, the activation of the
concentrate after the addition of thrombin showed an increase in CD62 expression
that reached 96,2 ± 1,8% of the platelets. PRP analysis at 24 hours of
incubation at room temperature showed a percentage of activated platelets of
16,1 ± 9,8%. As occurred with fresh PRP, the addition of thrombin carried a
total increase of activated platelets of 96,2 ± 0,7%.
Discussion
All blood manipulation processes entail certain changes in the ultrastructure of blood cells that can result in lesions that affect how they function. Although these lesions are largely reversible, the changes that take place in the platelets during their processing and storage, act as useful parameters for predicting the clinical effectiveness of the concentrates. 14
The analysis of the prepared PRP, according to the protocol for successive tube centrifugation, gives a result of concentrate enrichment that is between 3 and 4 times the recount of the platelets present in peripheral blood. This quantity of platelets is sufficient for achieving the local application objectives of this preparation, which is different from using platelets for transfusions. PRP obtained in this fashion allows the formation of a clot with an excellent consistency for transporting different types of bone grafts and biomaterials. This involves a supplementary supply to the middle of the lesion of a series of growth factors that act as mediators of the regenerative processes.
While some authors defend the idea that the biological activity of PRP derived from the supply of growth factors requires a quantity of between 0,9-1x106 platelets/µl in the normal volume of concentrate (6-10 ml), 1 there does not appear to be any conclusive study to demonstrate this. The number of platelets necessary for obtaining an adequate amount of each of the factors produced by the platelets has not been defined, in the same way that the number of cells contained in the concentrate is the only way of establishing the quantity of the factors released. Weibrich and Kleis compared two PRP preparation systems in their studies, through an analysis of platelet efficiency obtained with each system and the quantification of the principal growth factors contained in the final product. These authors conclude that, while there is a significant association between the number of platelets and the concentration of TGF-b, this association is not significant for the other factors analyzed (PDGF, IGF), and the number of platelets on their own cannot be used for predicting the quantity of growth factors that will be produced. The work by Zimmerman and cols.13 also had similar results in the analysis of the factors present in platelet concentrations obtained by different techniques. The authors stress the differences in the activation state of the platelets as one of the factors that contribute to this variability. Dugrillon and cols12 studied the platelet recount and the content in TGF-b1 of the PRP subjected to different centrifugation strengths. This work clearly showed that intensities of over 800 g produced greater platelet efficiency, but the quantity of TGF-b contained in the final product is reduced. This descent in the quantity of factors is a consequence of platelet activation on being subjected to important mechanical forces, with the resulting release into the medium of the granule contents, which is prematurely lost on removing the surplus fraction of plasma. As a result, the effectiveness of PRP is not only related to the fact that it contains a particular platelet concentration, but it is also related to the importance of guaranteeing that the platelets remain in tact until they are used.
In our study, the degree of platelet integrity in PRP is analyzed by studying the activation state and functional reserve. The measurement of CD62 expression and the response to stimulation with thrombin are the parameters frequently used for analyzing platelet concentrations, not only in local application but also for transfusional usage.14,16-18 The figure of 2,7% of platelet activation in extracted blood through venous puncture is in accord with previously published figures.19 In our case, the percentage of activated platelets in fresh PRP was between 3-5% and 16% after being stored for 24 hours. These figures are within the range described in other publications that analyze the concentration of platelets for hematological use, in which the percentage of activated platelets is between 7%19 and 25% after 24 hours.14 From a functional point of view, good results have been observed with concentrates containing a reported 20-30% of activated platelets.20
Another indicator of platelet viability in PRP is the positive response observed after thrombin stimulation, which results in a correct content release of intracellular deposits. The expression of membrane P-selectin is accompanied in physiological conditions by the release and expression of other molecules contained in the reservoirs, among which the different growth factors are found.21
Lastly, with regard to the storage period of platelet concentrates, it should be pointed out that blood derivatives, processed in an open circuit, should not be used after 6 hours of their preparation. The PRP obtained through double tube centrifugation should meet this recommendation. Thus, since platelets, analyzed in PRP after 24 hours, have been found in good condition, it would appear that this guarantees a sufficient margin as to their good condition and their functional reserve, which are required in usual conditions of the application period.
Conclusions
In this work the protocol described for preparing PRP, guarantees that the cell elements are maintained in the best condition until used. The fact that the platelets are activated during the surgical act and not before, avoids the loss of growth factors in the preparation processes of the concentrate, or their premature degradation.
![]() Correspondence:
Correspondence:
Concepción Sáez-Torres Barroso.
Banc de Teixits.
Fundació Banc de Sang i Teixits de les Illes Balears.
C/ Rosselló i Caçador 20.
07004 Palma de Mallorca. Baleares, España
Email: bteixits@bstib.com
Recibido: 11.03.05
Aceptado: 28.05.07
References
1. Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg 2004;62:489-96. [ Links ]
2. Becerra J, Andrades JA, Santamaria JA, Cifuentes M, Guerado E. [Bone regeneration, cell therapy and tissue engineering]. Med Clin (Barc) 2001;116:23-34. [ Links ]
3. Sanchez AR, Sheridan PJ, Kupp LI. Is platelet-rich plasma the perfect enhancement factor? A current review. Int J Oral Maxillofac Implants 2003;18:93-103. [ Links ]
4. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet- rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85:638-46. [ Links ]
5. Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants 1999;14:529-35. [ Links ]
6. Schliephake H. Bone growth factors in maxillofacial skeletal reconstruction. Int J Oral Maxillofac Surg 2002;31:469-84. [ Links ]
7. Weibrich G, Hansen T, Kleis W, Buch R, Hitzler WE. Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone 2004;34:665-71. [ Links ]
8. Soffer E, Ouhayoun JP, Anagnostou F. Fibrin sealants and platelet preparations in bone and periodontal healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:521-8. [ Links ]
9. Sonnleitner D HPSD. A simplified technique for producing plateletrich plasma and platelet concentrate for intraoral bone grafting techniques: a technical note. Int J Oral Maxillofac Implants 2000;15:879-82. [ Links ]
10. Kassolis JD, Rosen PS, Reynolds MA. Alveolar ridge and sinus augmentation utilizing platelet-rich plasma in combination with freezedried bone allograft: case series. J Periodontol 2000;71:1654-61. [ Links ]
11. Rodriguez A, Anastassov GE, Lee H, Buchbinder D, Wettan H. Maxillary sinus augmentation with deproteinated bovine bone and platelet rich plasma with simultaneous insertion of endosseous implants. J Oral Maxillofac Surg 2003;61:157-63. [ Links ]
12. Dugrillon A, Eichler H, Kern S, Kluter H. Autologous concentrated platelet- rich plasma (cPRP) for local application in bone regeneration. Int J Oral Maxillofac Surg 2002;31:615-9. [ Links ]
13. Zimmermann R, Jackubietz R, Jackubietz M, y cols. Different preparation methods to obtain platelet components as a source of growth factors for local application. Transfusion 2001;41:11217-24. [ Links ]
14. Wang C, Mody M, Herst R, Sher G, Freedman J. Flow cytometric analysis of platelet function in stored platelet concentrates. Transfus Sci 1999;20:129-39. [ Links ]
15. Weibrich G, Kleis WK. Curasan PRP kit vs. PCCS PRP system. Collection efficiency and platelet counts of two different methods for the preparation of platelet-rich plasma. Clin Oral Implants Res 2002;13:437-43. [ Links ]
16. Schmitz G, Rothe G, Ruf A, y cols. European Working Group on Clinical Cell Analysis: Consensus protocol for the flow cytometric characterisation of platelet function. Thromb Haemost 1998;79:885-96. [ Links ]
17. Michelson AD. Flow cytometry: a clinical test of platelet function. Blood 1996; 87:4925-36. [ Links ]
18. Eppley BL, Woodell JE, Higgins BS. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg 2004;114:1502-8. [ Links ]
19. Wyant TL, Smith PC, Brown B, Kantor AB. Whole blood microvolume laser scanning cytometry for monitoring resting and activated platelets. Platelets 2001;12:309-18. [ Links ]
20. Holme S, Sweeney JD, Elfath MD. The expression of p-selectin during collection, processing, and storage of platelet concentrates: relationship to loss of in vivo viability. Transfusion 1997;37:12-7. [ Links ]
21. Rendu F, Brohard-Bohn B. The platelet release reaction: granules constituents, secretion and functions. Platelets 2001;12:261-73. [ Links ]











 text in
text in