My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Cirugía Oral y Maxilofacial
On-line version ISSN 2173-9161Print version ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 n.6 Madrid Nov./Dec. 2009
What would your diagnosis be?
¿Cuál es su diagnóstico?
Male patient, 50 years-old. No relevant prior medical history or surgeries. Four months before going to the emergency room the patient started experiencing pain in the left hemi facial section and was diagnosed with neuralgia of the V pair (being treated with carbamazepine). Two months later he starts hypoesthesia of the ipsilateral inferior alveolar nerve and it is removed from the left wisdom teeth (periapical cyst). The reason he went to the emergency room (four months after diagnosing the trigeminal nerve neuralgia) is left peripheral facial paralysis associated with hypoesthesia of the right inferior alveolar nerve.
The Physical exam reveals evidence of complete left facial paralysis and a sub mandible tumor about 2x2 cm in size. The sub maxilla gland is normal upon palpation and has proper saliva drainage through the Wharton duct. We test the hypoesthesia of both inferior alveolar nerves using palpation; the rest of the neurological exploration is insignificant. There are no signs of trismus, dysphagia or dyspnoea. There is no fever, celulitis or pain related to an infection with an odontogenic cause. The mouth floor is not indurated and the tonsils have not been displaced.
The analysis doesn't show significant changes.
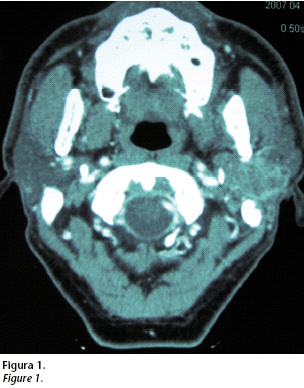
A multi cut CT is carried out with intravenous contrast, where we observe a deep lobe mass in the left parotid gland about 3x3x4 cm in size. This tumor has poorly defined borders, heterogeneous attenuation and peripheral luster. It is touching the ramus and the mandible chondyle. It occupies pharyngeal space and is located touching the inferior slope of the rock (Fig. 1).
Duct carcinoma over the pleomorphic adenoma of the parotid gland
Carcinoma ductal sobre adenoma pleomorfo de parótida
I. Navarro Cuéllar1, J. González Martín-Moro3, J.M. Múñoz Caro2, L. Pingarrón Martín1, J.L. del Castillo Pardo de Vera2, D.M. Benito5, M. Burgueño García4
1 Médico residente. Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario La Paz. Madrid. España
2 Médico adjunto. Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario La Paz. Madrid. España
3 Médico adjunto. Servicio de Cirugía Oral y Maxilofacial. Hospital General de Ciudad Real. España
4 Jefe de Servicio. Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario La Paz.Madrid. España
5 Médico residente. Servicio de Anatomía Patológica. Hospital Universitario La Paz. Madrid. España
Malignant salivary gland tumors make up about 1-3% of all head and neck cancers and 0.3% of all malignant tumors.1 The parotid gland, just like in benign tumors of the salivary gland, is the most common site.
Certain clinical signs can be lead us towards an area of malignancy of a parotid tumor: a mass with stony consistency, attached to deep levels and painful upon palpation (possibly nervous affectation) expansive growth and rapid evolution (it could also be a Warthin tumor) and a polinodular morphology (also common in pleomorphic adenoma relapses). However, facial paralysis, cervical adenopathies and cutaneous spread lead us to the most dependable diagnosis. Parotid tumors of the deep lobe are often diagnosed late because they were not obvious and don't have any other symptoms. In fact, nervous affectation can be the start of malignant tumors that poorly fit the prognostic.
In the case of a clinically palpable parotid tumor, aspiration perforation with a fine needle (APFN) continues to be, for many authors, the first complete test necessary for diagnosis. However, APFN has it limits when compared to other histological analysis techniques, like "frozen section" when determining histological lineage for both malignant and benign tumors.14
The second diagnostic tool used when dealing with a suspicious malignant tumor of the parotid gland has to be an image test. In general benign masses have well defined borders and a homogenous luster, while malignant masses can have irregular borders (which can be associated with a mixed tumor, especially if it is polinodular) and a heterogeneous luster. The nuclear magnetic resonance, NMR is the chosen test. With the NMR we can get more enhancements of the soft tissues allowing us to more accurately establish the limits of the tumor and their possible infiltration. Compared to the computed tomography (CT) the NMR has sensitivity to determine the borders almost 80% while the CT offers only 63%. When sensitivity is considered to establish local infiltration, it is 89% for NMR and 65% for CT. However, the CT is still a fundamental diagnostic tool in evaluating bone affectation.2
The diagnosis of the deep lobe masses in the parotid include benign lesions like the lymph epithelial cysts found in HIV+ patients, Sjögren syndrome, benign tumors (pleomorpho adenoma, Warthin tumor, oncocitoma, etc.) primary malignant tumors, metastasis, and lymph proliferate syndromes.13
Biological behavior, as well as prognostic of parotid malignant tumors varies based on their histological lineage. Mucoepidernoid carcinoma is usually the most common followed by acinar cell carcinomas, Aden carcinoma (in various forms), cystic adenoid carcinoma (cylindroma) and pleomorpho carcinoma. However, in the United Kingdom, exadenoma pleomorpho carcinoma is more common, in some series, than the mucoepidernoid carcinoma.3
Mixed ex-tumor carcinoma is a pleomorpho adenoma in which a malignant neoplasia develops over its epithelial component. Its origin can be an untreated and malignant pleomorpho adenoma (malignization interval can be up to 20 years) or malignization of a recurring tumor.3 The relapse rate of the pleomorpho adenoma is between 4-45% depending on the surgical technique used (parotidectomy vs. tumorectomy) and its malignant transformation can be up to 12%.4 To diagnose and define it a pleomorpho adenoma should be surrounded by tumor tissue with malignant characteristics. In cases with long development and in those were carcinoma completely substituted the adenoma the presence of hyaline is characteristic of pleomorpho adenoma degeneration.5
Ex pleomorpho adenoma carcinoma usually affects people between the ages of 60-70 without a clear preference of men or women. Normally it appears as a painless, slow growing mass then suddenly after years of development it begins to grow rapidly. The malignant lesion is usually included in the benign and has irregular borders and an infiltrated pattern.6
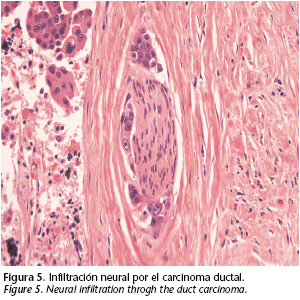
Ductal carcinoma of the salivary gland was first described in 1968 by Kleinsasser8 establishing more than 80% in the parotid gland. Histologically it has a carcinomatous component between the ducts and another one that is infiltrative. The one between the ducts has different growth patterns like solid, cribiform and papillary while the infiltrative component is a desmoplasic stroma. Up to 30% of patients can have intra tumor calcification. An over statement of the oncoprotein c-erb-2 is associated to poor prognostic (favoring proliferation, migration and cellular differentiation).7 P53 mutation and over expression of the HER-2 protein are immunohistologically typical of this type of tumor.8 There are studies that suggest that Trastuzumab hormonal therapy (blocking the tumor growth factors) is effective in those tumors like mammary and salivary duct carcinoma, with over expression of the oncoprotein HER2.9
Facial paralysis (40%), pain, perineural invasion (70%), cervical ganglion affectation (60%) and long term metastasis development are common clinical discoveries of parotid gland duct carcinoma. The recurrence rate is about 40%.
In this type of tumor the total partoidectomy and the cervical emptying, radiotherapy, postoperative chemotherapy and systematic and hormone therapy (if necessary) should be the chosen therapy. For neck N0, cervical emptying is justified.
There are studies that confirm that postoperative radiotherapy when treating ex pleomorpho adenoma carcinomas in patients with pN0 necks, improves the local control from 49-75%. Radiotherapy varies between 45 and 71 Gy in line with cervical propagation of illness and global survival rate varies from 16% for N+ to 67% for N0.11
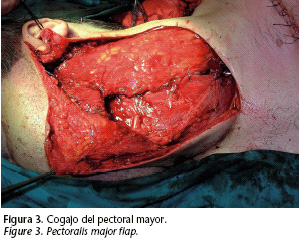
There are many reconstructive possibilities described in the literature: muscular or local cutaneous flaps, regional muscular- cutaneous flaps because they are large pectoral and wide dorsal and the free micro vascularized flaps: facial-cutaneous scapular, rectal abdominal flap, lateral arm flap, anterior lateral flap of thigh, latissimus dorsi.12
In the case of our patient a PAAF was carried out resulting in a carcinoma undifferentiated of large cells. The follow up study was done with a chest abdominal CT because in the majority of occasions dissemination of this type of tumor is of the lungs or mediastinum. This CT didn't provide images that suggest metastasis. The cervical-facial CT shows tumors in the deep lobe of the parotid with the previously described characteristics. For example, a sub mandible mass 3x3 cm in size with heterogeneous attenuation and areas of necrosis in the interior that are suggestive of adenopathies in pathological ranges and in intimate contact between both carotids, internal jugular and sternocleideomastoid (Fig. 2).
The patient was treated using a left radical parotidectomy associated with ipsilateral radical cervical emptying. An intra operative biopsy of the facial nerve was sent to be evaluated for intracranial extension via the perineural. The result was "nervous tissue with no signs of tumor infiltration". Considering the bad prognostic of the patient, reconstruction was performed with a muscular flap from the major pectoral that provides volume and protects the large veins (Fig. 3). The intervention was completed with suspension of the modiolus and a cantopexia to minimize the after effects of facial paralysis.
The anatomopathological announcement was: "Ductal carcinoma amply invasive over pleomorpho adenoma, identifying the presence of neural and vascular infiltration. Margins free of tumor affectation. Radical cervical emptying without the presence of a tumor" (Figs. 4 and 5). The immunohistochemical to detect HER-2 was negative. Therefore the sub mandible mass described in the CAT suggested adenopathy in pathological ranges turns out being the actual tumor that extended to the sub mandible space.
The patient has been treated by the radiotherapy oncology department (60 Gy more over impression with 5 Gy). Months later in a follow-up study with body CT we found disease dispersed in the lung mediastinum, brain, meninges and bone (ribs and vertebrates). It has been treated by the medical oncology department (cysplatin 60 mg/m2, epirubisin 60 mg/m2 and cyclophosphamide 600 mg/m2) and palliative radiotherapy administered in the brain, meninges and column. A medular compression syndrome has been designed that has paraparesis and monoplegia of the right leg.
In conclusion ductal carcinoma of the parotid gland is a tumor that has an unfavorable prognostic (lymphatic dissemination and early hematogene) in which early diagnosis and multidisciplinary treatment surgery, radiotherapy and chemotherapy are key to getting the best prognostic in patients.
![]() Correspondence:
Correspondence:
Ignacio Navarro Cuéllar
Servicio de Cirugía Oral y Maxilofacial.
Hospital Universitario La Paz
Paseo de la Castellana 264,
28046 Madrid. España
E-mail: nnavcu@hotmail.com
References
1. Bhattacharyya N, Fried MP. Determinants of Survival in Parotid Gland Carcinoma: a Population Based Study. American Journal of Otolaryngology 2005;26:39-44. [ Links ]
2. Raine C, Saliba K, Chippindale AJ, Mclean NR. Radiological Imaging in Primary Parotid Malignancy. British Journal of Plastic Surgery 2003;56:637-47. [ Links ]
3. Reza Nouarai SA, Hope KL, Nelly CG, Mclein NR, Soames JV. Carcinoma Ex Benign Pleomorphic Adenoma of the Parotid Gland. Plast Reconstr Surg 2005;116: 1206. [ Links ]
4. Zbären P, Tschumi I, Nuyens M, Stauffer E. Recurrent Pleomorphic Adenoma of the Parotid Gland. The American Journal of Surgery 2005;189:203-7. [ Links ]
5. Cawson RA, Gleeson MJ, Everson JW. Pathology and Surgery of the Salivary Glands. Oxford: ISIS Medical Media 1997. [ Links ]
6. Barrios JM, Soler F, Guerra B, Navarro Cuéllar C.Tumores malignos de las glándulas salivares. Tratado de Cirugía Oral y Maxilofacial (vol. II). Navarro C, García-Marín F, Ochandiano S. Ed Arán, 2004. [ Links ]
7. Etges A, Pinto DS, Kowalski LP, Soares FA. Salivary duct carcinoma: immunohistochemical profile of an aggressive salivary gland tumour. J Clin Pathol 2003;56: 914-8. [ Links ]
8. Jaenhe M, Roeser K, Jaekel T, Schepers J, Albert N, Löning T. Clinical and Immunohistologic Typing of Salivary Duct Carcinoma. Cancer 2005;103:2526-33. [ Links ]
9. Nabili V, Tan JW, Bhuta S, Sercarz JA, Head CS. Salivary Duct Carcinoma: A Clinical And Histologic Review With Implications For Trastuzumab Therapy. Head and Neck 2007;29:907-12. [ Links ]
10. Sefik A, Fan C, Barnes L, Myers EN. Salivary Dcut Carcinoma. Otolaryngol Head Neck Surg 2003;129:720-5. [ Links ]
11. Chen AM, García J, Bucci MK, Quivey JM, Eisele DW. The Role of Postoperative Radiation Therapy in Carcinoma Ex Pleomorphic Adenoma of the Parotid Gland. Int J Radiation Oncology Biol Phys 2007;67:138-43. [ Links ]
12. Teknos TN, Nussenbaum B, Bradford CR, Prince ME, El-Kashlan H, Chepeha DB. Reconstruction of Complex Parotidectomy Defects Using the Lateral Arm Free Tissue Transfer. Otolaryngol Head and Neck Surg 2003;129:183-91. [ Links ]
13. Ric Harnsberger H. Parotid Space. Serie radiológia clínica. Los 100 diagnósticos principales en cabeza y cuello. Harnberger, Hudgins, Wiggins, Davidson. Ed Elsevier. [ Links ]
14. Zbären P, Guélat D, Loosli H, Stauffer E. Parotid tumors: Fine needle aspiration and/or frozen section. Otolaryngology, Head and Neck Surgery 2008;139:81-5. [ Links ]











 text in
text in