Introduction
The United States National Academy of Medicine (formerly known as the Institute of Medicine) has released three Consensus Reports reviewing the evidence for the prevention of mental disorders and the promotion of healthy mental, emotional, and behavioral development. Their latest report (National Academies of Sciences, Engineering, and Medicine, 2019) points out that traditional treatment interventions have not reduced the incidence or prevalence of depression. Methods to scale up the implementation of current knowledge are needed to do so.
In this commentary, we describe evidence that half the cases of major depression can be prevented with psychological approaches. We describe several digital approaches developed at the Institute for International Internet Interventions for Health (i4Health) that can be used to make these psychological interventions available to all who need them. We conclude by suggesting that the prevention of perinatal depression should be our first priority.
Major Depression Can Be Prevented
Major depressive episodes can now be prevented using psychological mood management methods. These methods were initially developed for the treatment of clinical depression. It has become clear that these methods can also be used to manage subthreshold symptoms, so individuals do not cross threshold into a clinical episode. Systematic reviews show that major depression can be prevented using current psychological preventive interventions. In a recent meta-analysis, Cuijpers et al. (2021) found that the overall incidence of depression can be decreased by 19% via such interventions. However, a closer look reveals that approximately 20% of all randomized controlled trials reviewed (n = 50, 50 pairwise comparisons) yielded a reduction in incidence of at least 50% (range: 51-99%). This evidence suggests that specific psychological interventions have the potential to prevent depression in over half of cases. A systematic review conducted by the U.S. Preventive Services Task Force (USPSTF) demonstrated that two programs, the Reach Out, Stand strong, Essentials for new mothers (ROSE) Program and the Mothers and Babies Course [Curso Mamás y Bebés] had evidence for preventing 50% or more of new cases of postpartum depression (PPD) (O’Connor et al., 2019) and should be considered as preventive interventions for those at highest risk for perinatal depression.
Though clearly effective, psychological interventions administered in person cannot reach even the majority of people who could benefit from them. Internet-based interventions have the potential to increase access to populations worldwide. A recent meta-analysis of online psychological and psychoeducational depression prevention interventions (based on cognitive behavior therapy) found a small but significant effect in reducing depressive symptoms (Rigabert et al., 2020). Online self-guided treatment and prevention interventions should be implemented widely to treat and prevent depression locally and worldwide. At i4Health we are attempting to do just that.
The Institute for International Internet Interventions for Health
The mission of Palo Alto University’s Institute for International Internet Interventions for Health (i4Health) is to develop, evaluate, and disseminate digital health interventions worldwide at no charge to all who want to use them. Our efforts include large-scale online screening studies; full-length web-based psychological interventions focused on smoking cessation, mood management, and prevention of postpartum depression; digital micro-interventions; and the use of texting and chatbots (see Table 1). We encourage our colleagues to harness the combined power of psychology and technology to serve as many people as possible.
Worldwide Screening for Depression
A large multilingual, multinational online investigation conducted by our team has revealed a high prevalence of depression among individuals searching for depression information online (Leykin et al., 2012). Unfortunately, the majority of those screening positive for depression in that study were not receiving any kind of professional help. The level of untreated and undertreated depression in the larger community is likely even higher. Many individuals suffering from depression lack mental health literacy necessary to realize the cause of their suffering and, for many, help for depression may be unavailable in their community or inaccessible due to financial or other reasons.
Full-length Web-based Psychological Interventions
Interventions that are unsupported (no human contact) and self-guided are especially beneficial for the global community because they are highly scalable and cost-effective. At i4health we have developed a self-guided unsupported intervention for treatment of depression, the Depression Management Course (a multi-lesson, multi-week intervention based on Cognitive Behavioral Therapy) that has been shown to reduce depression levels and increase self-efficacy of depression management, with effects being evident at 7-month follow-up (Leykin et al., 2014).
The Mothers and Babies Online Course (eMB) is an internet adaptation of the Mothers and Babies Course [Curso Mamás y Bebés] that was examined as a prevention intervention among English- and Spanish-speaking pregnant women in a pilot randomized controlled trial (eMB vs. an information-only control condition). The eMB intervention did not reach statistical significance but trended in the direction of improved depression outcomes among those who were at highest depression risk and who engaged in the online intervention (Barrera et al., 2015). We are currently testing a new version of the eMB, which we hope will increase its effectiveness.
Micro Interventions for Depression
In addition to testing full length treatments, we have studied the effect of brief, unsupported internet interventions for depressive symptoms also described as “micro interventions”. Micro interventions for depression are usually single session interventions that last a few minutes and aim to produce small effects on mood. Studies on micro interventions have several advantages. First, developing and testing a brief intervention can be done in a short period of time, providing immediate and rapid information that guides the development of subsequent versions of the interventions. Second, they can act as dismantling studies testing efficacy of specific treatment components. Third, users of effective micro interventions may continue to seek out and use similar micro interventions. Results of our studies showed significant advantage of a brief behavioral activation intervention compared to a wait list condition (Bunge et al., 2017), and an improvement in depressive symptoms at a one-week follow-up.
One of depression’s most troubling symptoms is suicidality. Indeed, a concerning level of suicidality, including recent suicide attempts, was found in the aforementioned screening study (Leykin et al., 2012). Our team has piloted an Internet-Based Safety Plan, a self-guided, interactive, and downloadable online resource for individuals struggling with suicidality (Spangler et al., 2020). Though it is common for intervention studies to exclude those at risk for suicidality, given that many may not have any treatment options, addressing suicidality with self-guided online tools may offer hope for Internet users who would otherwise have no resources.
On Texting and Chatbots for Depression
The BabyText Program (Barrera et al., 2020) is a brief text-messaging intervention based on the MB curriculum that provides perinatal women “tips” on how to manage changes in their mood during and after pregnancy. Another digital approach to treat and prevent depression is the use of Chatbots, that is, conversational agents delivered via text messages. Chatbots for mental health can be conceptualized as interactive self-help. Researchers at i4Health have studied how users engaged with a Chatbot’s (Tess) conversations designed for management of depressive symptoms, finding that most U.S. adults users completed a mean of 2.18 conversations with Tess (Dosovitsky et al., 2020). While this number may seem low, it is higher than the mean number of modules completed in studies of most smartphone apps.
A Taxonomy of Digital Interventions
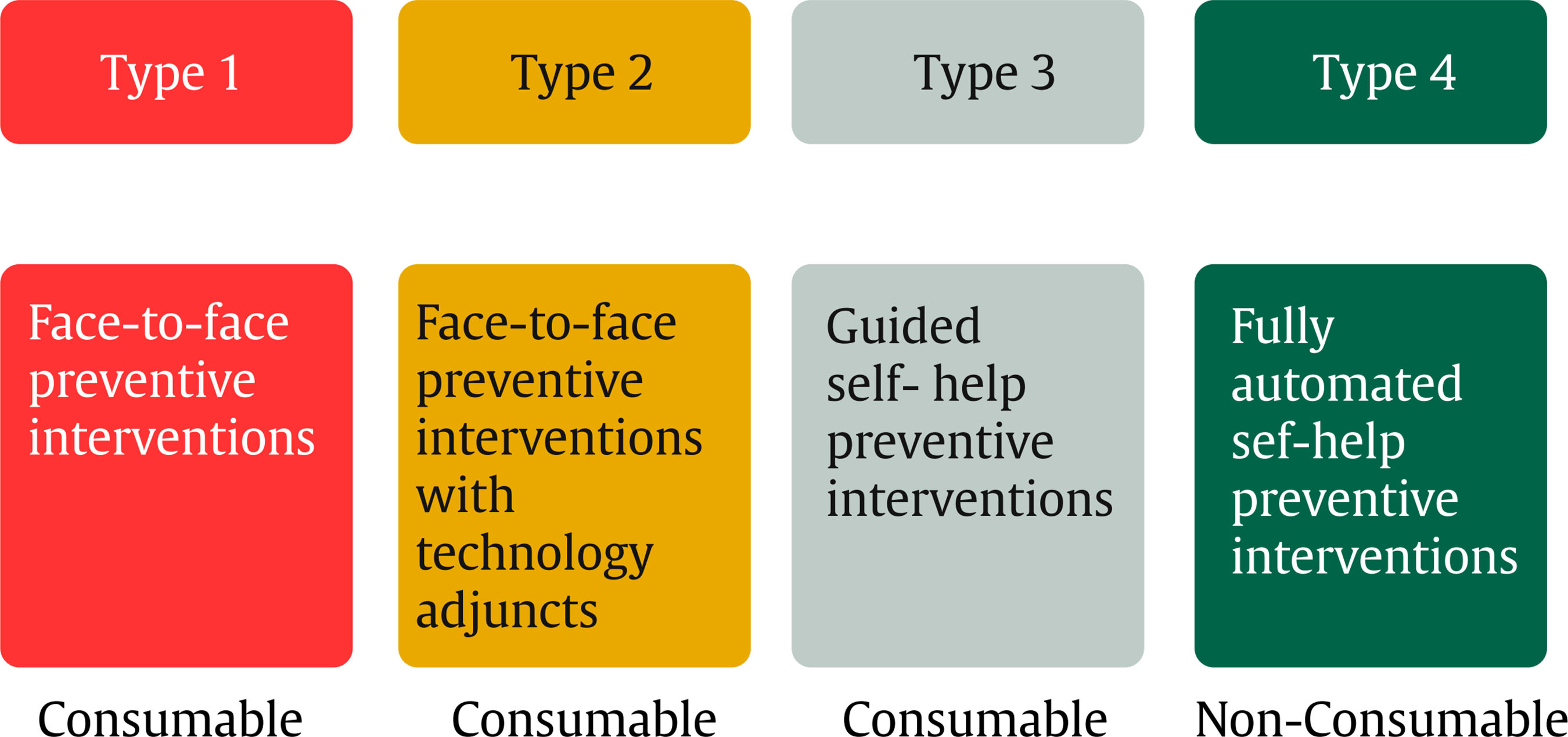
We have recommended that Massive Open Online Interventions and Digital Apothecaries to serve as their repositories (Muñoz et al., 2018) be established in order to reduce health disparities worldwide. In our article on digital apothecaries (Muñoz et al., 2018), we propose four types of digital interventions to address disparities in access to evidence-based prevention and treatment interventions (see Figure 1). Types 1 (training providers) and 2 (creating adjuncts to be used by providers) are focused on increasing the availability and effectiveness of psychological interventions administered in person. Type 1 would involve online training resources to increase the number of lay and professional providers who can deliver in-person prevention and treatment interventions. Type 2 involves digital tools that could be used to enhance traditional interventions, such as telehealth or the use of digital tools to increase daily monitoring of mood, thoughts, and behaviors in cognitive-behavioral interventions. Type 3 and 4 refer to self-help interventions. Type 3 (guided self-help interventions) involves the use of human support from coaches or guides. Type 4 (fully automated self-help interventions) have been developed and tested to be used without human support and can therefore be made freely available to anyone in the world.
Note that because Type 4 interventions do not require human support, they are non-consumable. Unlike the other three types, which are limited by the number of providers available, Type 4 interventions can be used repeatedly by an unlimited number of people anytime, anywhere, without losing their therapeutic or preventive power. The marginal cost of Type 4 interventions (the cost of providing the intervention to one more person) eventually approaches, though it never reaches, zero: a website that costs one million dollars to build and test would cost $1000 per person if 1000 people use it, $1 per person if one million people use it, and ten cents per person if ten million people use it.
On the Road to a World Without Depression
It is time to implement prevention and treatment interventions for depression on a global scale. Digital interventions provide us with a feasible method to do so. We recommend that, as a first priority, each nation focuses on preventing the impact of perinatal depression on each successive generation being born from now on (Muñoz, 2019). Imagine if all pregnant women at risk for depression were offered preventive interventions as part of their prenatal care and, as a result, fifty percent of all potential cases of perinatal depression were prevented. For the remaining fifty percent who developed depression, early treatment would be delivered. Would the cohort of babies spared the negative sequelae of maternal depression have lower prevalence of emotional problems than earlier cohorts of children of depressed mothers? If so, this would be an important step on the road toward a world without depression (Muñoz, 2001).