My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.15 n.42 Murcia Apr. 2016
REVISIONES
Nursing interventions for patients with erectile dysfunction after radical prostatectomy: integrative review
Intervenções de enfermagem para pacientes com disfunção erétil após prostatectomia radical: revisão integrativa
Intervenciones de enfermería para pacientes con disfunción eréctil después de prostatectomía radical: una revisión integral
Appoloni Eduardo, Aline Helena*; Napoleão, Anamaria Alves** and Carvalho, Emilia Campos de*
*Escola de Enfermagem de Ribeirão Preto - Universidade de São Paulo EERP-USP. E-mail: aline-12@hotmail.com
**Universidade Federal de São Carlos - UFSCar. Brasil.
ABSTRACT
This study aimed to identify nursing interventions for patients undergoing radical prostatectomy. This is an integrative review, guided by the question "What are the nursing interventions directed to patients with erectile dysfunction after radical prostatectomy?", held on the databases PubMed, Web of Science, CINAHL, SCOPUS, Cochrane Library, LILACS and on the list of references of selected articles. The final sample was comprised of 10 papers; 43 nursing interventions were identified and grouped in 10 categories. The nursing interventions for patients with erectile dysfunction after radical prostatectomy focused on the education regarding the nature of erectile dysfunction, treatment and sexuality; besides strengthening the involvement of partners during the process of coping with and treating the dysfunction. These interventions may be useful so that nurses can act during the follow-up of these patients, providing better quality of life and well-being.
Key words: erectile dysfunction; prostatectomy; nursing care; nursing intervention.
RESUMO
Este estudo teve o objetivo de identificar intervenções de enfermagem para pacientes submetidos a prostatectomia radical. Trata-se de uma revisão integrativa norteada pela questão "Quais são as intervenções de enfermagem direcionadas aos pacientes com disfunção erétil após prostatectomia radical?", realizada nas bases PubMed, Web of Science, CINAHL, SCOPUS, Biblioteca Cochrane, LILACS e na lista de referências a partir dos artigos selecionados. Compuseram a amostra final 10 artigos e 43 intervenções de enfermagem foram identificadas e agrupadas em 10 categorias. As intervenções de enfermagem para pacientes com disfunção erétil após prostatectomia radical concentraram-se na educação acerca da natureza da disfunção erétil, tratamento e sexualidade; além de fortalecerem o envolvimento das esposas durante o processo de enfrentamento e tratamento da disfunção. Estas intervenções poderão ser úteis para que enfermeiros possam atuar durante o acompanhamento destes pacientes, proporcionando melhora da qualidade de vida e bem-estar.
Palavras chave: disfunção erétil; prostatectomia: cuidado de enfermagem; intervenção de enfermagem.
RESUMEN
Este estudio tuvo como objetivo identificar las intervenciones de enfermería en pacientes sometidos a prostatectomía radical. Se trata de una revisión integradora guiada por la pregunta "¿Cuáles son las intervenciones de enfermería dirigidas a pacientes con disfunción eréctil después de una prostatectomía radical?" buscado en PubMed, Web of Science, CINAHL, Scopus, Cochrane Library, LILACS y en la lista de las referencias de los artículos seleccionados. Compusieron la muestra final 10 artículos y 43 intervenciones de enfermería fueron identificadas y agrupadas en 10 categorías. Las intervenciones de enfermería para pacientes con disfunción eréctil después de prostatectomía radical se centraron en la educación sobre la naturaleza de la disfunción eréctil, el tratamiento y la sexualidad; además de fortalecer el compromiso de las esposas durante el proceso de abordaje y tratamiento de la disfunción. Estas intervenciones puedan ser útiles para que las enfermeras pueden actuar durante el seguimiento de estos pacientes, proporcionando una mejor calidad de vida y bienestar.
Palabras clave: disfunción erécti; prostatectomía; cuidados de enfermería; intervención de enfermería.
Introduction
We estimate that in the years 2014 and 2015 prostate is the most frequent type of cancer in Brazilian population, with 69,000 new cases, excluding non-melanoma skin cancers. The data correspond to the occurrence of around 70 cases for each 100,000 men. However, if diagnosed and treated early, it presents good prognosis and high survival rate for the treated patient.(1)
Treatment for prostate cancer is based on the tumor's grade and stage, on the patient's life expectancy, on the patient and doctor's preferences, varying from radical prostatectomy, radiotherapy, brachytherapy, hormonal therapy and watchful waiting.(2-4) Radical prostatectomy (RP) is an effective therapeutic option for the treatment of clinically localized prostate cancer in early stages and for patients who have a life expectancy of around 10 years.(2,4-6) Long-term monitoring of patients undergoing this surgical approach showed progression-free survival rate of around 80% in the first five years after surgery and of 69% in 10 years.(4)
The main disadvantage of an RP is the occurrence of complications such as urinary incontinence and erectile dysfunction that significantly affect the quality of life of patients.(5-8) The onset of these complications during the postoperative of radical prostatectomies is correlated to patients' reports on regretting having undergone the procedure.(9)
Recent studies indicate the occurrence of urinary incontinence of around 70% and erectile dysfunction of 68%.(10,11)
Erectile dysfunction refers to the persistent inability to have and/or maintain a penile erection for satisfactory sexual intercourse.(12) The development of erectile dysfunction after RP is related to injuries to nerve bundles, arterial injuries and smooth muscle lesion6,10,13 It is noteworthy that the regression of erectile dysfunction after RP depends on the degree of reversibility of these lesions.(10)
When complete recovery of erectile dysfunction occurs, it is slow and has time as a decisive factor; authors state that recovery happens around 18 months after surgery.(6,8,13) Therefore, it is important to have close monitoring of patients who are in recovery from erectile dysfunction caused by radical prostatectomy. It is also important to implement strategies to establish early sexual rehabilitation, since responses to drug treatment and improvements of the psychological state contribute to spontaneous recovery from erectile dysfunction.(13)
Many are the efforts and studies that promote the complete recovery of erectile function today. The main current forms of treatment are grounded on oral therapy (phosphodiesterase type 5 inhibitors), intracavernous injections (vasoactive substances), intraurethral injections, vacuum erection devices, penile extenders, combined treatments, experimental treatments and surgeries.(7,10,13)
Incorporating these treatment modalities by themselves in rehabilitation may bring unsatisfactory results, since this stage requires strict guidance of patients and their partners on the treatment and its effects, as well as motivation, knowledge, confidence and involvement of both during rehabilitation.(7) Therefore, multidisciplinary monitoring of the couple, educational programs and guideline development are essential to the rehabilitation of the erectile function and to overcome the effects of this complication in the patients' lives.
Care and strategies for the treatment of erectile dysfunction are extremely necessary, because the sexuality related disorders are responsible for changes in quality of life, self-esteem, general health and psychological conditions of both the patients and their partners.(7)
Nurses should consider incorporating interventions for the rehabilitation of the erectile function during the follow-up or discharge of postoperative patients. These interventions may provide positive effects to this population, since it may fill possible gaps in the patients' hospital treatment and daily life.(14,15)
The identification of nursing diagnoses related to alterations of the erectile function directs individualized care focused on the specific needs of patients who undergo prostate surgery. In the classification of nursing diagnoses of NANDA-International, Inc., this condition is represented by the diagnosis Sexual dysfunction (00059).(16) The Nursing Intervention Classification (NIC) proposes Sexual Counseling as the main intervention for the diagnosis. It refers to the "use of an interactive helping process focusing on the need to make adjustments in sexual practice or to enhance coping with a sexual event/disordef."(17) the activities presented in this intervention are not directly aimed at specific problems of erectile dysfunction, thus it is important to identify specific nursing actions for this complication of RP.
Therefore, this study aims to identify in scientific literature the nursing actions for patients with erectile dysfunction after radical prostatectomy.
Material and method
This is an integrative literature review to access the available evidence in the nursing literature regarding specific actions for patients with erectile dysfunction after RP. This review model is a research method that summarizes the evidence of a particular subject in order to obtain general conclusions about it. The review was developed in two distinct phases: elaboration of the research question, sampling, analysis of studies, evaluation of primary studies, analysis and synthesis of the review results, and presentation of the review.(18)
This review was developed while supported by the following question: "What are the nursing interventions to patients with erectile dysfunction after radical prostatectomy?"
The papers research was conducted online, in May 2015, on the electronic databases PubMed (National Library of Medicine and National Institutes of Health), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, Scopus, Cochrane Library, and Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS). We also conducted manual research in articles from the list of references of the papers selected in the review.
We used the following controlled descriptors from the U.S. National Library of Medicine's (NLM) MeSH for the studies survey: erectile dysfunction, prostatectomy, nursing care, and nursing intervention. The Boolean operators AND and OR were employed as they allow the realization of combinations among the descriptors during the search for the studies - AND for restrictive combinations and OR for additive combinations. The descriptors related to nursing care were grouped using the operator OR; e.g. nursing care OR nursing intervention. The Boolean operator AND was used between the descriptors erectile dysfunction, prostatectomy, and grouping the other descriptors.
Articles that presented possible nursing interventions to patients with erectile dysfunction after radical prostatectomy were included. The articles that discussed results from care or treatment protocols, reviews, books, theses, and dissertations were excluded. We could not stipulate the year limit of publication or also the language in which they were written.
We read the titles and abstracts from each electronic base, according to the search strategies; if the summary was not available, we searched for the full article to continue the study. When the article met the established criteria, it was selected for the sample of analyzed articles.
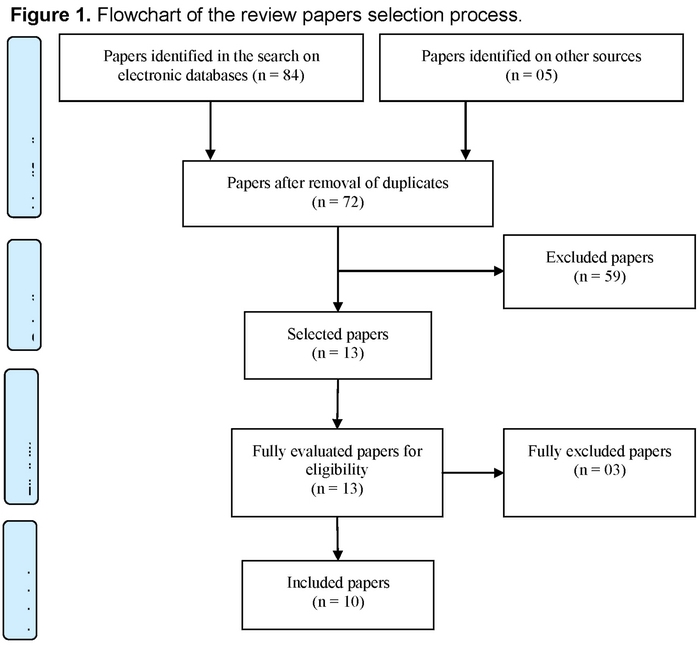
We found 84 research papers on the electronic databases: 48 from PubMed, 18 from Web of Science, 6 from Cochrane Library, 5 from CINAHL, 5 from SCOPUS, and 2 from LILACS. It is noteworthy that 5 papers were included in the review from the search in the list of references of the selected papers. This way, 89 papers were identified.
After removal of published papers (17), we were left with 72 that had their tiles and abstracts analyzed. Fifty-two were excluded at this stage for various reasons -because they were review studies (25), studies that explored the experience of patients and couples who experienced erectile dysfunction after radical prostatectomy (10), studies that focused on quality of life after rd (05), studies that described the main complications after Rd surgery (05), interventions that were not specifically related to nursing (04), interventions for urinary incontinence (03), description of frequency of erectile dysfunction after surgery (04), editorial (01), and interventions for erectile dysfunction after radiotherapy (02).
The remaining 13 papers were fully analyzed and 3 of them were excluded for not describing the intervention for rehabilitation of erectile dysfunction (03). The paper selection process is illustrated in Figure 1, which was adapted from PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guideline.(19)
The selected papers were fully accessed for data extraction. We then proceeded to read and register data in a form built on MS Word, considering the paper's identification (reference, information about the first author and subject area, idiom and country where the study was conducted), study objective, methodological details (type of study, sampling strategies, data collection, sample size, method of data analysis), results and appointments on interventions for erectile dysfunction and main conclusions. In addition, we evaluated the levels of evidence for each study(20) and the quality of clinical trials specifically randomized using the Jadad scale(21).
The Jadad scale allows the analysis of methodological quality of clinical trials; a point is assigned to each of these features in the study: randomization, blinding and description of exclusions and losses of the sample; if randomization and blinding are considered adequate, another point is summed up; if they are considered inadequate, a point is subtracted from each item. The Jadad scale varies from 0 to 5, the scores that are ≥ 3 represent adequate methodological quality of the studies.(21)
The synthesis of review results was established descriptively, since we adopted results from various research outlines. This approach made it possible to categorize the intervention themes and their directions (specific to patients or couples).
Results
The 10 papers we analyzed were published in English language, in foreign journals - nine of them in the USA(22-30) and one in Europe(31). Most researches were conducted in the USA (07)(25-31), followed by Taiwan(22), Spain(23) and Italy(24), with one publication each. Nurses were the first authors in six papers(22,23,26,27,29,30), psychologists were the first authors in three papers (25,28,31), and a doctor is the first author in one paper(24). However, in all studies the identified interventions were performed by nurses. The publication period of the papers varied from the years 2001 and 2012.
Regarding the analyzed studies' methodological outline, six of them were randomized controlled clinical trials(22,24,26-28,31), one of them was a qualitative study(29), two of them were descriptive studies(23,25), and one of them was an experience report of experts in the area of urological nursing(30).
The level of evidence identified in the studies varied from II (evidence from well-designed randomized controlled trials), VI (evidence from descriptive or qualitative studies) and VII (expert committee reports).(20) Thus, six studies showed level of evidence II, three studies show level of evidence VI, and one shows a level of evidence VII. Two of the clinical trials studies presented a Jadad score of 5, and two studies presented score 3, which features studies of good methodological quality; two studies showed Jadad score of 1, which means that it has compromised methodological quality.(21)
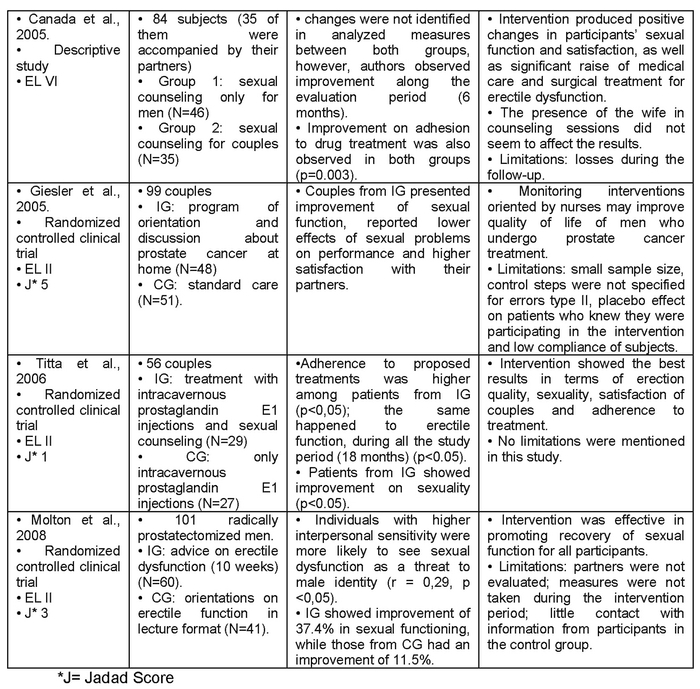
Chart I illustrates the main information from the analyzed papers in this review, regarding methodological issues, interventions for erectile dysfunction applied in each study, main results, conclusions, and limitations.
In half of the papers(5), only the patients were the focus of nursing interventions(22,27,28,31); in the other papers, interventions were directed to the couple, that is, interventions involved the wives or partners in the studies(24-26,29,30).
In three of the analyzed papers, the definition of erectile dysfunction adopted was described(22,24). That definition was common for all three works.
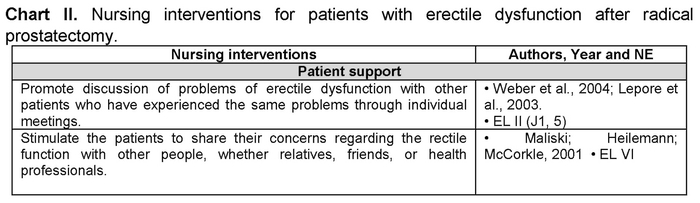
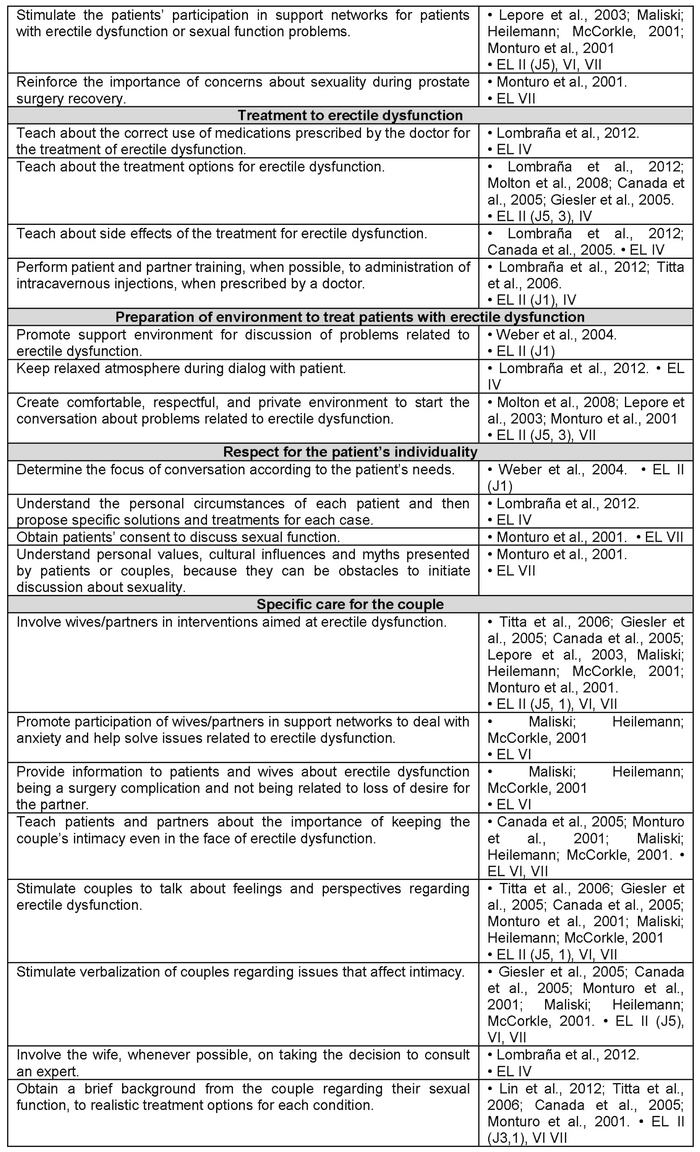
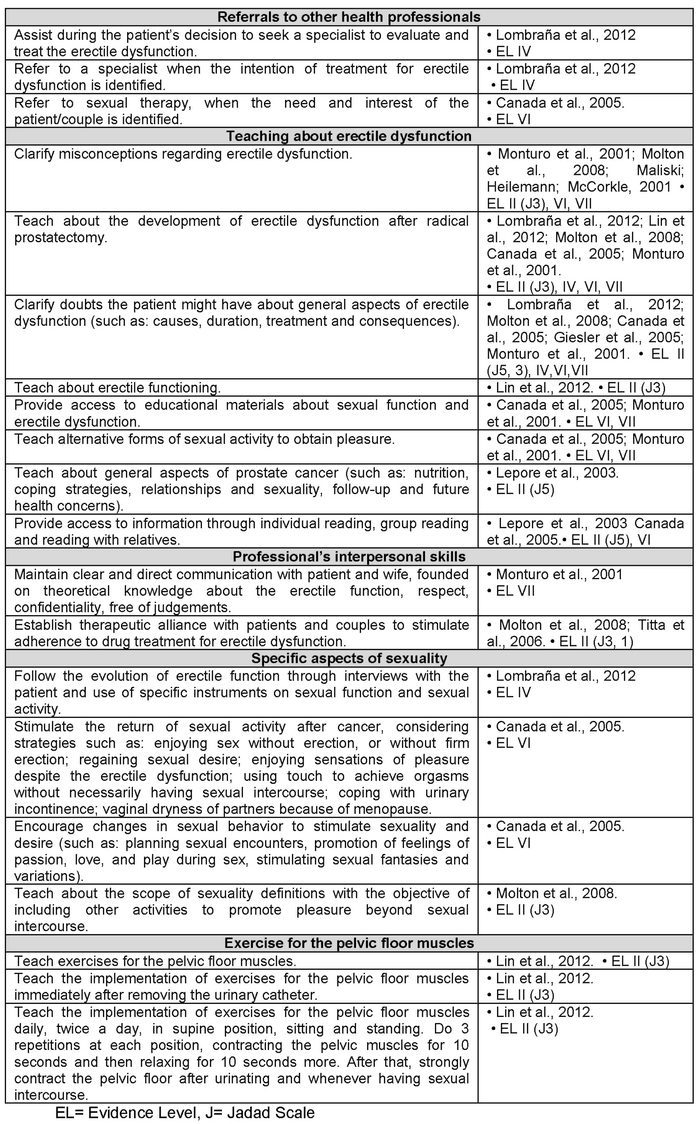
In total, 43 nursing interventions were identified in the study sample and grouped according to common themes, in categories aimed both at the patient and the couple, and predominantly directed to support and teaching. The interventions grouped in the respective themes are shown in Chart II.
Part of the studies described nursing interventions implemented in samples comprising patients who underwent radical prostatectomy (six papers)(22,23,27,29-31); in the other papers, samples were comprised of patients who underwent surgery but also other types of treatment, such as radiotherapy, brachytherapy, joint radiation and brachytherapy, and cryotherapy(26,28); radical prostatectomy with radiotherapy(25). In one study patients who underwent cystectomy were also included in the sample.(24)
Discussion
Erectile dysfunction triggered by RP is a frequent problem for the patients who have undergone this type of prostate cancer treatment. The maintenance of sexual function is an important aspect of quality of life and well-being for men and couples. The RP is currently being conducted in even younger patients who wish to keep their sexual activities. Because of that, care aimed at contributing to this function is necessary and require special attention.(7,32)
The United States Institute of Medicine recommends that strategies aimed at complications related to cancer treatment to be a priority for health professionals, since a large portion of treated patients has high life expectancy.(32) The analyzed studies present the relevance and benefits of those interventions for patients with erectile dysfunction, since the studied interventions are somehow effective in improving sexual satisfaction, erectile function and sexual function.(22,24-29,31)
This analysis provides a survey of 43 nursing interventions for patients with erectile dysfunction who had underwent RP. These interventions were grouped in 10 categories, according to the biological, psychosocial, educational and behavioral aspects of the condition and according to the nurses who will address these intimate and delicate issues such as sexuality. Thus, we consider that the aspects of the identified interventions meet the dimensions of human sexuality, which is a multidimensional, complex phenomenon that includes biological, psychological, interpersonal and behavioral dimensions.(30)
Much of the identified interventions are aimed at results in the psychosocial dimensions of erectile dysfunction, such as social support, self-efficacy(27), depressive symptoms(26,27), sexual satisfaction(23,27,28), knowledge(23,28), quality of life related to health(25,26,28), stress(25) and interpersonal sensitivity(31): This feature supports the review conducted by Latini et al.(32), in regard to the intervention focus. The researchers analyzed studies about interventions for erectile dysfunction, since the interventions aiming at psychosocial outcomes were unanimous.
The psychosocial interventions are of great importance for the rehabilitation of patients with prostate cancer in general, since they have a positive effect in the form of addressing problems experienced by patients due to prostate cancer treatment, such as sexual dysfunction.(15)
Interventions focused on the physical dimensions of erectile dysfunction were also identified in this study, as they involve aspects related to restoring the sexual function, response to treatment and treatment adherence.(22,24,25,31)
Interventions focused on education of patient and partner were in some way proposed in all of the analyzed studies; the themes of these educational interventions involved general aspects of erectile dysfunction (causes, relation with surgery, treatment)(22-26,30,31), general aspects of sexuality(28,30,31), general aspects of prostate cancer(25,28,31); and clarification of misconceptions regarding erectile dysfunction(29,31).
Educational interventions aimed at restoring erectile function were identified in a systematic review as an effective strategy for the discomfort caused by RP in patients' sexual function, since these interventions, when successful, proved to be able to provide improved physical consequences after surgery and on the quality of life of patients and partners.(15)
A relevant aspect identified in the analyzed studies concerns the inception and duration of interventions for erectile function. Interventions that started early (around a month after surgery), during the postoperative period, produced positive, statistically significant effect on sexual function, when compared to their control groups.(22,24,26,28,31) We identified that the time of intervention and the monitoring of patients who participated in the studies was long, around 12 months after the start of intervention. However, the best effects on erectile dysfunction occurred after the fourth month.(22,24,26,27)
Exact time for the start of nursing interventions aimed at erectile dysfunction is not established in the literature. We note the same for the duration of these interventions throughout the postoperative period. However, the analysis of papers that comprised the sample of this review suggested that when the interventions started early after surgery, it was possible to obtain better effects on the sexual function, satisfaction and erectile dysfunction.
The required duration of interventions for erectile dysfunction should take the evidences pointing to the delay in recovery of erectile function after RP (18 months)(6) and the start of drug treatment into consideration. Studies that follow the evolution of erectile function in patients who underwent surgery reinforce the importance of implementing these interventions in long-term, since most patients showed some level of sexual dysfunction or sexual dissatisfaction two years after surgery.(33,34)
Another important aspect identified in the analyzed studies that deserves to be considered is the involvement of partners or wives of patients who underwent radical prostatectomy. Four of the ten papers in the sample involved the patients' partners in the tested interventions(24-26,29); this way, it was possible to bring up eight nursing interventions specifically for couples.
It is known that RP has an impact on the sexuality and sexual function levels of couples.(9,24) thus, partners have a strong influence on the patients' ability to cope and adapt to the disease, to prostate cancer treatment and to erectile dysfunction, besides influencing patients to adhere to treatment.(9) An educational intervention, developed during four meetings, directed to couples whose men had undergone prostate cancer treatment, presented significant adherence to erectile dysfunction treatment.(25)
Although the importance of partners/wives in coping with erectile dysfunction is well understood in the literature, we emphasize that they also need emotional support and education on the issues involving prostate cancer, RP and its complications(29). In order for wives and partners to exercise this important support role, they also need to understand the situations their partners are going through.(9,29)
Wives and partners experience a considerable stress load during prostate cancer treatment, initially in fear for the life and health of their partners, but also for exercising the role of caretakers during the entire postoperative period, and for sometimes feeling rejected by their husbands/partners during erectile dysfunction. Because of that, interventions aimed at these wives/partners are also fundamental. Davison et al. (9) point to the need of consulting wives/partners on the desire of participating in specific activities for the treatment of erectile dysfunction with their husbands/partners.
In this review, we pointed out the aspects related to the preparation and specific skills of nurses who are going to address patients with erectile dysfunction. The interventions related to sexuality are important for patients who will be assisted by nurses, although they are not significantly addressed or taught in nursing school. It is important that nurses have sound theoretical knowledge on sexual function and erectile dysfunction, self-confidence, communication skills and respect to deal with couples and patients' issues on sexual dysfunction.(30)
Conclusions
Final analysis of this review's studies sample allowed us to identify 43 nursing interventions for patients with erectile dysfunction after radical prostatectomy. These interventions were grouped in ten categories, according to common themes. Among the analyzed interventions in each study, it was possible to point their positive effects on the patients' general sexual function, erectile dysfunction and sexual satisfaction; they also satisfactorily contribute to the adherence to erectile dysfunction treatment, marital relationships and the patients' adaptation to the new situation.
Given the complexity involving the effect of erectile dysfunction in the patients and their partners' lives, the care should not only aim at the dysfunction's curative aspects, but also at sexuality as a whole, knowledge about sexual function and respect for the patient. The analyzed papers described nursing interventions that possibly meet that complexity perceived by the intervention themes that emerged from the analysis of each study.
The development of this integrative review allowed us to gather fundamental interventions for nurses to monitor patients with erectile dysfunction. With the early detection of prostatic carcinoma, whose treatment of choice is the radical prostatectomy, a large number of sexually active, young adult patients are exposed to the development of erectile dysfunction. Thus, these interventions may be useful for nurses to act during the monitoring of these patients, providing better quality of life and well-being.
This review was limited by the identification of a small number of studies with high evidence level - only six of them were randomized controlled clinical studies, and only two among them showed maximum score in Jadad scale. Moreover, it was not possible to identify any systematic review with meta-analysis about nursing interventions for patients with erectile dysfunction after radical prostatectomy until now. These gaps suggest the need for further development of studies to test specific interventions for this situation.
Received: June 26, 2015;
Accepted: August 4, 2015
References
1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Estimativa 2014: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2014. [ Links ]
2. Amorim GLCC, Cruz GMG, Veloso DFM, Kartabil JD,Vieira JC, Alves PR. Comparative analysis of radical prostatectomy techniques using perineal or suprapubic approach in the treatment of localized prostate cancer. Einstein, 2010 Jun;8(2PT1):200-4. [ Links ]
3. Presti JC. Prostate biopsy: current status and limitations. Rev Urol. 2007 Summer; 9(3):93-8. [ Links ]
4. Speight JL, Roach MIII. Advances in the treatment of localized prostate cancer: the role of anatomic and functional imaging in men managed with radiotherapy. J Clin Oncol. 2007 Mar; 25(8):987-95. [ Links ]
5. Li M, Mei W, Wang P, et al. Propofol reduces early postoperative pain after gynecological laparoscopy. Acta Anaesthesiol Scan. 2014 Mar; 56(3):358-75. [ Links ]
6. Barreira JVN. Tratamento da disfunção erétil após prostatectomia radical. (Dissertação). Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto, Porto, Portugal, 2013. [ Links ]
7. Liu S. Penile rehabilitation following radical prostatectomy. Urol Sci. 2010 Jun; 21(1):19-22. [ Links ]
8. Walsh PC. Radical prostatectomy for localized prostate cancer provides durable cancer control with excellent quality of life: a structured debate. J Urol. 2000 Jun; 163(6):1802-7. [ Links ]
9. Davison BJ, Matthew A, Elliott S, Breckon E, Griffin S. Assessing couples' preferences for postoperative sexual rehabilitation before radical prostatectomy. BJU Int. 2012 Nov; 110(10):1529-35. [ Links ]
10. Mazzola C, Mulhall JP. Penile rehabilitation after prostate cancer treatment: outcomes and practical algorithm. Urol Clin North Am. 2011 May; 38(2): 105-18. [ Links ]
11. Schiavina R, Borghesi M, Dababneh H, et al. Survival, continence and potency (SCP) recovery after radical retropubic prostatectomy: a long-term combined evaluation of surgical outcomes. Eur J Surg Oncol. 2014 Dec; 40(12): 1716-23. [ Links ]
12. National institute of health. Impotence: NIH Consensus Development Panel on Impotence. JAMA. 1993 Jul; 270(1): 83-90. [ Links ]
13. Nunes P, Rolo F, Mota A. Prostatectomia radical e actividade sexual. Acta Urológica. 2004 Jan; 21(1): 15-31. [ Links ]
14. Jakobsson J. Assessing recovery after ambulatory anaesthesia, measures of resumption of activities of daily living. Anesthesiology. 2011 Dec; 24(1):p.601-4. [ Links ]
15. Lassen B, Gattinger H, Saxer S. A systematic review of physical impairments following radical prostatectomy: effect of psychoeducational interventions. J Adv Nurs. 2013 Dec; 69(12):2602-12. [ Links ]
16. Herdman TH, Kamitsuru S. NANDA International Nursing Diagnoses: Definitions and Classification, 2015-2017. Oxford: Wiley-Blackwell, 2014. [ Links ]
17. Bulecheck GM, Butcher HK, Dochterman JM. Classificação de intervenções de enfermagem (NIC). Rio de Janeiro: Elsevier, 2010. [ Links ]
18. Galvão CM, Mendes KDS, Silveira RCCP. Revisão integrativa: método de revisão para sintetizar as evidências disponíveis na literatura. In: Brevidelli MM, Sertório SCM. TCC- Trabalho de conclusão de curso: guia prático para docentes e alunos da área da saúde. 4a Ed. São Paulo: Iátria, 2010. p. 105-126. [ Links ]
19. Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009; 6(6):e1000097. [ Links ]
20. Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: a guide to best practice. 2ed. Lippincott Williams & Wilkins: China, 2011. [ Links ]
21. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17(1):1-12. [ Links ]
22. Lin Y, Yu T, Lin VC, Wang H, Lu K. Effects of early pelvic-floor muscle exercise for sexual dysfunction in radical prostatectomy recipients. Cancer Nurs. 2012 Mar; 35(2):106-14. [ Links ]
23. Lombraña M, Izquierdo l, Gomez A, Alcaraz A. Nursing care program for erectile dysfunction after radical prostatectomy. Clin J Oncol Nurs. 2012 Oct;16(5):E178-82. [ Links ]
24. Titta M, Tavolini IM, Moro F, Custernino A, Bassi P. Sexual counseling improved erectile rehabilitation after non-nerve-sparing radical retropubic prostatectomy or cystectomy-results of a randomized prospective study. J Sex Med. 2006 Mar; 3(2):267-73. [ Links ]
25. Canada AL, Neese LE, Sui D, Schover LR. Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer, 2005 Dec; 104(12): 2689-700. [ Links ]
26. Giesler RB, Given B, Given CW, et al. Improving the quality of life of patients with prostate carcinoma: a randomized trial testing the efficacy of a nurse-driven intervention. Cancer, 2005 Aug; 104(4):752-62. [ Links ]
27. Weber BA, Roberts BL, Resnick M, et al. The effect of dyadic intervention on self-efficacy, social support, and depression for men with prostate cancer. Psychooncology, 2004 Jan; 13(1):47-60. [ Links ]
28. Lepore SJ, Helgeson VS, Eton DT, Schulz R. Improving quality of life in men with prostate cancer: a randomized controlled trial of group education interventions. Health Psychol. 2003 Sep; 22(5): 443-52. [ Links ]
29. Maliski SL, Heilemann MV, Mccorkle R. Mastery of postprostatectomy incontinence and impotence: his work, her work, our work. Oncol Nurs Forum, 2001 Jul; 28(6):985-92. [ Links ]
30. Monturo CA, Rogers PD, Coleman M, Robinson JP, Pickett M. Beyond sexual assessment: lessons learned from couples post radical prostatectomy. J Am Acad Nurse Pract. 2001 Nov; 13(11):511-6. [ Links ]
31. Molton IR, Siegel SD, Penedo FJ, et al. Promoting recovery of sexual functioning after radical prostatectomy with group-based stress management: the role of interpersonal sensitivity. J Psychosom Res. 2008 May; 64(5):527-36. [ Links ]
32. Latini DM, Hart SL, Coon DW, Knight SJ. Sexual rehabilitation after localized prostate cancer: current interventions and future directions. Cancer J. 2009 Jan; 15(1): 34-40. [ Links ]
33. Magheli A, Busch J, Leva N, et al. Comparison of surgical technique (Open vs. Laparoscopic) on pathological and long term functional outcomes following radical prostatectomy. BMC Urol. 2014 Feb; 7(14):14-18. [ Links ]
34. Jakobsson L, Fransson P. Patient reported outcome measure (PROM) of quality of life after prostatectomy - results from a 5-year study. Open Nurs J. 2013 Dec; 27(7):165-73. [ Links ]











 text in
text in