My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.16 n.48 Murcia Oct. 2017 Epub Dec 14, 2020
https://dx.doi.org/10.6018/eglobal.16.4.267721
Originales
Postoperative pain in women undergoing caesarean section
1Nurse. Doctorate in Nursing. Federal University of Goiás. Brazil.
2Nursing student. Federal University of Goiás. Brazil.
3Nurse. Master in Nursing. Federal University of Goiás. Brazil.
4Nurse. Master student in Nursing. Federal University of Goiás. Brazil.
5Nurse. PhD in Nursing. Associate Professor at the Federal University of Goiás. Brazil.
Methods
Cross-sectional study. A total of 1062 post-cesarean section women were interviewed in immediates pre- and post-operative. Pain intensity and quality were evaluated through the Numerical Rating Scale (0-10) and McGill Pain Questionnaire-SF. The variables were explored by descriptive measures and the incidence of postoperative pain calculated with a 95% confidence interval.
Results
The incidence of pain was 92,7% (IC 95%: 90,9 - 94,2). The average level of pain intensity at the time of worst pain was 6,6 (dp=2,2). The descriptors more frequently chosen were “aching” (91.6%) “tender” (70.0%) and “throbbing” (56.1%).
Conclusions
High-intensity postoperative pain is a reality for post-cesarean section women, showing the importance of pain assessment for implementation of curative and preventive actions to reduce losses in the recovery of women.
Key words Pain; Postoperative pain; Cesarean section
INTRODUCTION
Postoperative pain frequently has nociceptive characteristics, that is, it derives from tissue or organ lesions, whose nociceptive stimuli are perceived as painful1. In case of direct nerve lesion, or even strain or compression, neuropathic pain can also be present2.
Although postoperative pain is a physiological event, the improper relief of this experience may entail greater risks for people’s health. The harmful effects include neuroendocrine changes, involving responses of the hypophysis and adrenal glands, which can cause negative repercussions in different organic systems, such as the cardiovascular, respiratory and gastrointestinal, besides effects in the central nervous system3. Highly intensive postoperative pain is also a predictor of chronic pain4)(5)(6.
In this scenario, very frequent surgeries like cesarean sections demand additional attention, considering that they rank among the most common surgeries among women of fertile age7. In addition, this procedure takes place at a time of considerable hormonal and emotional changes related to the pregnancy and arrival of the baby8, which can negatively influence the postoperative pain, in view of the multidimensional nature of this experience9.
Additional losses for the post-cesarean section women include commitment of the capacity to take care of their babies, breastfeed effectively and interact with their infant during the postpartum10. In addition, researchers appoint that cesarean sections represent the main cause of chronic pain among women11.
Estimates show immediate postoperative pain incidence rates after cesarean sections amounting to 77.4%5 and 100%12, with the pain being of high intensity13. Research on the women’s perceived quality of this pain is poor. Nevertheless, there is evidence that the most frequently used words to describe it belong to the sensory-discriminative dimension of the painful experience12.
In view of the continuing increase in cesarean section rates identified around the world and the need to expand the knowledge on the occurrence and characteristics of this experience in the immediate postoperative period, this study was developed to estimate the incidence, intensity and quality of postoperative pain in women submitted to cesarean section.
MATERIAL AND METHOD
This is a cross-sectional analysis of data from a prospective longitudinal study, developed at a private health institution that is a partner of the Unified Health System (SUS). This medium-sized hospital (45 beds) executes, on average, 120 elective cesarean sections per month, about 70% of which are funded by the SUS. The institution is located in the Brazilian Midwest, in a major city with about 1,412,000 inhabitants14.
The convenience sample consisted of 1062 women aged 14 years or older, submitted to cesarean sections, conscious and oriented at the time of the data collection. Women were excluded if submitted to emergency surgery, diagnosed with a malign disease, persistent hemodynamic instability, under chronic use of opioids, in labor and in intense pain that made it impossible for them to answer the observers’ questions, unable to see, hear or talk and victims of postoperative problems, such as hemorrhage, cardiorespiratory arrest and death of the infant.
The research variables were postoperative pain occurrence, intensity and quality. “Postoperative pain” was considered as proposed by the American Society of Anesthesiologists15, that is, pain in surgical patients after the procedure, due to tissue lesion and the manipulation of organs and structures.
The pain intensity was measured with the help of an 11-point Numerical Pain Rating Scale (NPRS), a one-dimensional, ordinal tool that permits measuring the pain intensity through scores representing the amount of pain felt (0 (zero) = no pain; 1, 2, 3 and 4 = mild pain; 5 and 6 = moderate pain; 7, 8 and 9 = severe pain and 10 (ten) = worst possible pain). As people use figures since childhood, the advantage of the NPRS is that the participants are familiar with it. This scale has been widely used in hospitals and/or clinics for rapid, non-invasive and valid information about acute or chronic pain16.
To assess the postoperative pain quality, the short form of the McGill Pain Questionnaire (MPQ-SF)17 has been used, translated and adapted for use in Brazil18, consisting of 15 pain descriptors, eleven (11) of which describe the sensory-discriminative dimension of this experience and four the affective-motivational dimension. The descriptors are quantified on a four-point scale, in which 0 = none, 1 = leve, 2 = mild and 3 = severe.
The sociodemographic variables, such as age, marital status, education, paid job, socioeconomic situation (assessed based on the Brazilian Economic Classification Criterion of the Brazilian Market Research Associations19) and the surgical and clinical variables, such as the type of anesthesia, anesthetic drug used and intraoperative analgesia were presented to characterize the sample only.
The data were collected by nine trained observers in the immediate preoperative and postoperative periods, after personal introduction, when information was provided about the research objectives. All participants signed the Free and Informed Consent (IC) or the Informed Assent Form. The patients were contacted at the ward or apartments where they were hospitalized.
The data were subject to descriptive analysis. The categorical variables were presented in absolute and relative frequencies. The quantitative variables were summarized as means, standard deviation, medians, interquartile intervals (Q1, Q3), minima and maxima. The estimated incidence of postoperative pain was presented with a 95% confidence interval (CI:95%). The postoperative pain intensity was presented in categories (none=0, mild=1,2,3 and 4, moderate=5.6, strong=7,8,9, worst possible=10), and the pain descriptors according to how frequently (%) they were chosen.
Approval for the project was obtained from the Ethics Committee of Universidade Federal de Goiás, protocol number 421.825.
RESULTS
Among the 1062 participants, women between 20 and 35 years of age are prevalent, with an average age of 2.52 years (sd=5.7), married and who finished secondary education. The majority has a paid job, belongs to socioeconomic class C and receives health care through the SUS (Table 1).
Table 1 Socioeconomic and demographic characteristics of post-cesarean section women in Goiânia, GO, Brazil, 2015

As for the characteristics of the anesthetic-surgical technique, all women were submitted to spinal anesthesia, with administration of 0.5% bupivacaine heavy and intrathecal morphine. Little more than half of the women (50.3%) received another analgesic than the opioid drug in the intraoperative period. The administration of a simple analgesic drug was the most frequent practice among the associations (41.1%). A small part of the women had tubal sterilization together with the cesarean section (8.9%) (Table 2), and the median duration of the surgery was 30.0 minutes (Q1=30.0; Q3=40.0; MIN=14; MAX=90).
Table 2 Characteristics of intraoperative analgesia and tubal sterilization in post-cesarean section women in Goiânia, GO, Brazil, 2015

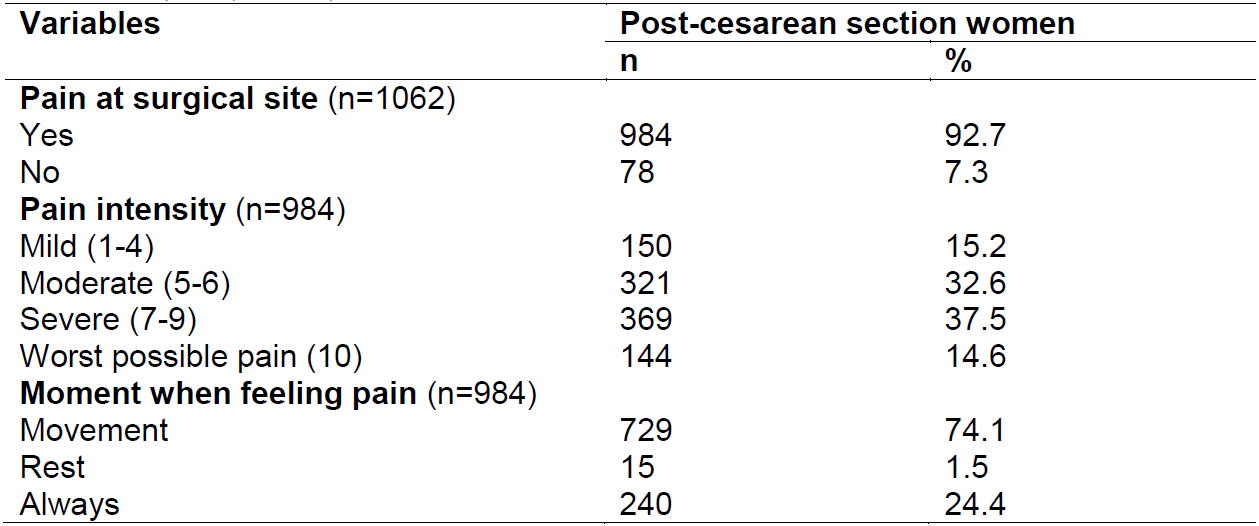
The incidence of immediate postoperative pain corresponded to 92.7% (95% CI: 90.9 - 94.2). The main referred pain intensity at the worst moment (“strongest” pain) was 6.6 (sd=2.2) and the “weakest” pain 3.3 (sd=2.0), triggered by movements. Only 22.5% mentioned mild pain or absence of pain (Table 3).
Table 3 Characteristics of postoperative pain among post-cesarean section women in Goiânia, GO, Brazil, 2015
The words the women chose most frequently to characterize the pain were: “aching” (91.6%), “tender” (70.0%) and “throbbing” (56.1%), and the descriptors that prevailed after quantifying the intensity of the feeling the descriptor expressed as severe were: “aching” (32.6%), “tender” (17.0%) and tiring-exhausting (10.9%). The descriptors that indicated a moderate quantity of the feeling expressed were “aching” (38.4%), “tender” (25.9%) and “tugging” (22.3%).
DISCUSSION
In this study, it was evidenced that postoperative pain remains very frequent after cesarean section. In addition, a minority referred mild pain, a clinically unacceptable fact in view of the knowledge advances on the painful experience and its relief. Similarly, in other surgical scenarios, estimates appointed postoperative incidence rates of 100% in this population8)(20)(21.
We know that mechanical and/or thermal nociceptive stimuli produce tissue lesions during the surgery, resulting in the accumulation of algogenic substances in the free nerve endings. After these have been sensitized, the neuronal membrane is depolarized and the painful information is carried to the suprasegmentary structures that process the pain cognitive and consciously22. The inflammatory process also takes place, releasing substances that promote an exaggerated response to the painful stimuli in the surgical injury (primary hyperalgesia) and the surrounding region (secondary hyperalgesia)23.
Although the occurrence of postoperative pain is a physiological and therefore “expected” event in the immediate postoperative period, the proper relief of this experience can be guaranteed through the use of more advanced anesthetic-surgical techniques, the availability of new drugs and the application of basic knowledge on postoperative pain24.
In addition, pain relief is a human right and the health professionals should assume the commitment to comply with the ethical principles, including the patients’ autonomy on their therapeutic plan; the principle of beneficence, focused on antiethical conducts in response to the demands of patients in pain; the principle of non-maleficence, involving dilemmas regarding the risk-benefit of using opioids and the application of unnecessary painful procedures; and the principle of justice, which regulates the care practices and determines on the equalitarian distribution in the access to pain treatment25.
Concerning the postoperative pain intensity, in a prospective study involving 65 women, aimed at investigating the relation between experimental pain intensity and pain after cesarean birth, assessed at different moment during the first 48 hours after the surgery, using the 11-point NPRS, it was evidenced that the mean scores attributed to the intensity of this experience 12 hours after the end of the surgical procedure was 6.1820, similar to this research, in which, although the women received multimodal intraoperative analgesia, the postoperative pain intensity reached clinically important levels, similar to other studies8)(21.
High postoperative pain intensity after cesarean section was also found in a sample of 60 women investigated by Sousa et al.12, where the incidence of postoperative pain corresponded to 100%, with an average intensity of 6.9 (sd=2.1), assessed by means of the NPS. Limitations in the capacity to sit and get up were also found, pointing towards a possible constraint in the activities related to initial care for the infant, including breastfeeding.
In this study, although we did not intend to investigate losses in the women’s daily activities due to the postoperative pain, evidences have appointed higher pain frequencies when moving, in line with the findings by Sousa et al.12. In addition, the intensity of this pain scored higher than four (4) on the NPRS (0-10), a level considered unacceptable26, alerting to the potential losses in the accomplishment of daily activities.
An additional loss comes with the fact that the improper relief of highly intense pain in the immediate postoperative period represents one of the strongest predictors of chronic postoperative pain in women submitted to cesarean section5)(6.
When asked about the words that characterized the postoperative pain, the most frequently chosen descriptors were: “aching”, “tender” and “throbbing”, in the sensory group of the MPQ-SF. Sousa et al.12 also evidenced that the words the post-cesarean section women chose more frequently belonged to the sensory group - “tight” (62.5%); “grasping” (60%) and “straining” (57.5%).
Studies that investigated the quality of the pain in patients submitted to other types of surgeries, using the long27 and short form28 of the McGill Pain Questionnaire, found that the postoperative pain is predominantly described by means of sensory descriptors.
The word “aching”, similar to our findings, ranked among the most used descriptors to describe postoperative pain before the use of analgesic techniques and 30 minutes after this application in a sample of 40 patients submitted to different surgical interventions17.
McDonald and Weiskopf28 appoint that the higher frequency of words in the sensory dimension to describe the postoperative pain can partially be justified by disproportional number of words in each group of the questionnaire.
Nevertheless, we also observed the presence of descriptors from the affective dimension among the pain characteristics, signaling the presence of aspects of tension, fear and neurovegetative responses involved in the painful experience29.
These findings point towards the importance of assessing the painful experience in multiple dimensions. The biopsychosocial approach of pain is necessary, as the surgical procedure is frequently perceived as a very difficult time for the patients and their relatives. In this scenario, the nurses play a fundamental role in perioperative pain monitoring, with a view to the diagnosis, planning, implementation and assessment of processes and outcomes, aiming to achieve the patients’ ready recovery and the reduction of suffering. Therefore, knowing the other person’s subjectivity and understanding their multiple dimensions are necessary.
The reason why many patients still refer highly intense postoperative pain remains unknown, but we believe that multiple factors are involved, including a lack of pain assessment and documentation, absence of specific protocols for postoperative pain management, deficient management of educational programs for health professionals, limited use of effective analgesic techniques and low compliance with available guidelines on pain management30.
CONCLUSIONS
These study results evidenced that postoperative pain is a highly frequent experience among women submitted to cesarean section. The intensity of its manifestations is clinically unacceptable, that is, it can cause harm to mother and child in the immediate postoperative period.
The pain dimension expressed by the descriptors used most frequently to describe the pain after the cesarean section is the sensory-discriminative, although other descriptors in the affective-motivational dimension were also chosen, pointing towards the multidimensional nature of the painful experience, which alerts to the importance of the biopsychosocial approach in the choice of the analgesic therapeutics and preventive care during the perioperative period.
These evidences arouse reflections on the lack of actions to relieve postoperative pain, a fact that appoints the urgent need to remodel the way the health team professionals have managed pain in the surgical context, contributing to the choice, maintenance or replacement of the analgesic therapy and the implementation of care with a view to preventing the occurrence of this type of pain and, consequently, of the losses associated with the subtreatment of this experience.
REFERENCIAS
1. Ward CW. Procedure-specific postoperative pain management. Medsurg Nurs. 2014;23(2):107-10. [ Links ]
2. Loos MJ, Scheltinga MR, Mulders LG, Roumen RM. The Pfannenstiel incision as a source of chronic pain. Obstet Gynecol. 2008;111(4):839-46. [ Links ]
3. IASP. Associação Internacional Para Estudo da Dor. Guia para o Tratamento da Dor em Contextos de Poucos Recursos [internet]. Seatle: IASP Press; 2010 [citado 2016 set 05]. Disponível em: http://www.iasp-pain.org/files/Content/ContentFolders/Publications2/FreeBooks/GuidetoPainManagement_Portuguese.pdf. [ Links ]
4. VanDenKerkhof EG, Peters ML, Bruce J. Chronic pain after surgery: time for standardization? A framework to establish core risk factor and outcome domains for epidemiological studies. Clin J Pain. 2013;29(1):2-8. [ Links ]
5. Sng BL, Sia AT, Quek K, Woo D, Lim Y. Incidence and risk factors for chronic pain after caesarean section under spinal anaesthesia. Anaesth Intensive Care. 2009;37(5):748-52. [ Links ]
6. Cançado TOB, Omaris M, Ashmawi HA, Torres MLA. Dor crônica pós-cesariana. Influência da técnica anestésico-cirúrgica e da analgesia pós-operatória. Rev Bras Anestesiol. 2012;62(6):762-774. [ Links ]
7. Beiranvand S, Noparast M, Eslamizade N, Saeedikia S. The effects of religion and spirituality on postoperative pain, hemodynamic functioning and anxiety after cesarean section. Acta Med Iran. 2014;52(12):909-15. [ Links ]
8. Pan PH, Coghill R, Houle TT, Seid MH, Lindel WM, Parker RL, et al. Multifactorial preoperative predictors for postcesarean section pain and analgesic requirement. Anesthesiology. 2006;104(3):417-25. [ Links ]
9. IASP. International Association for the Study of Pain [internet]. IASP Taxonomy. 2012 [cited 2016 jun 22]. Disponível em: http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698&navItemNumber=576#Sensitization [ Links ]
10. Gadsden J, Hart S, Santos AC. Post-cesarean delivery analgesia. Anesth Analg. 2005;101(5):62-9. [ Links ]
11. Eisenach JC, Pan P, Smiley RM, Lavand'homme P, Landau R, Houle TT. Resolution of pain after childbirth. Anesthesiology. 2013;118(1):143-51. [ Links ]
12. Sousa L, Pitangui ACR, Gomes FA, Nakano MAS, Ferreira CHJ. Mensuração e características de dor após cesárea e sua relação com limitação de atividades. Acta Paul Enferm. 2009;22(6):741-7. [ Links ]
13. Nikolajsen L, Sorensen HC, Jensen TS, Kehlet H. Chronic pain following caesarean section. Acta Anaesthesiol Scand. 2004;48(1):111-6. [ Links ]
14. IBGE. Instituto Brasileiro de Geografia e Estatística [internet]. Censo Demográfico 2010: População estimada 2014. 2010 [citado 2015 mar 22]. Disponível em: http://cidades.ibge.gov.br/xtras/perfil.php?lang=&codmun=520870. [ Links ]
15. Sociedade Americana de Anestesiologia. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116(2): 248-73. [ Links ]
16. Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17(8):1022-4. [ Links ]
17. Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191-7. [ Links ]
18. Costa LCM, Mahera CG, McAuley JH, Hancock MJ, Oliveira WM, Azevedo DC, et al. The Brazilian-Portuguese versions of the McGill Pain Questionnaire were reproducible, valid, and responsive in patients with musculoskeletal pain. Journal of Clinical Epidemiology. 2011; 64(8):903-12. [ Links ]
19. ABEP. Associação Brasileira de Empresas de Pesquisa. Critério de Classificação Econômica Brasil [internet]. 2013 [citado 2013 jan 21]. Disponível em http://www.abep.org/novo/Content.aspx?ContentID=835>. [ Links ]
20. Buhagiar L, Cassar OA, Brincat MP, Buttigieg GG, Inglott AS, Adami MZ, et al. Predictors of post-caesarean section pain and analgesic consumption. J Anaesthesiol Clin Pharmacol. 2011;27(2):185-91. [ Links ]
21. Karlstrom A, Engstrom-Olofsson R, Norbergh KG, Sjoling M, Hildingsson I. Postoperative pain after cesarean birth affects breastfeeding and infant care. J Obstet Gynecol Neonatal Nurs. 2007;36(5):430-40. [ Links ]
22. Alves Neto O, Costa CMC, Siqueira JTT, Teixeira MJ. Dor: princípio e prática. Porto Alegre: Artmed; 2009. [ Links ]
23. Woolf CJ. Recent advances in the pathophysiology of acute pain. Br J Anaesth. 1989;63(2):139-46. [ Links ]
24. Lovich-Sapola J, Smith CE, Brandt CP. Postoperative pain control. Surg Clin North Am. 2015;95(2):301-18. [ Links ]
25. Santos FDRP, Nunes SFL, Silva JPd, Silva RMO, Viana RP, Pereira VO, et al. Dor em pacientes no pós-operatório de cirurgias torácicas e abdominais. Rev Ciênc Ext [Internet]. 2014 [citado 2015 abril 23]; 10(3):99-107. Disponível em: http://ojs.unesp.br/index.php/revista_proex/article/download/926/1042. [ Links ]
26. Katz J, Poleshuck EL, Andrus CH, Hogan LA, Jung BF, Kulick DI, et al. Risk factors for acute pain and its persistence following breast cancer surgery. Pain. 2005;119:16-25. [ Links ]
27. Fortin JD, Schwartz-Barcott D, Rossi S. The postoperative pain experience: a description based on the McGill Pain Questionnaire. Clin Nurs Res. 1992;1(3):292-304. [ Links ]
28. McDonald DD, Weiskopf CS. Adult patients' postoperative pain descriptions and responses to the Short-Form McGill Pain Questionnaire. Clin Nurs Res. 2001;10(4):442-52. [ Links ]
29. Pimenta CAM, Teixeira MJ. Questionário de dor de McGill: Proposta de adaptação para a língua portuguesa. Rev Esc Enf USP. 1996;30(3):473-83. [ Links ]
30. Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet. 2011;377(9784):2215-25. [ Links ]
Received: September 13, 2016; Accepted: November 06, 2016











 text in
text in 


