My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.17 n.52 Murcia Oct. 2018 Epub Oct 01, 2018
https://dx.doi.org/10.6018/eglobal.17.4.306111
Originals
Effectiveness of the brass index in discharge Planning by case management nurses
1Enfermera. Hospital Universitario Virgen de la Victoria de Málaga. Málaga. España. ccruzadoalvarez@gmail.com
2Profesor/a de la Facultad de Ciencias de la Salud de la Universidad de Málaga. Málaga. España.
3Enfermera Gestora de Casos. Hospital Universitario Virgen de la Victoria de Málaga. Málaga.España.
Classifying patients according to complexity and frailty during hospitalization allows efficient planning of the scope of care required by the patient at discharge. The aim of this study was to measure the screening validity of the Blaylock Risk Assessment Screening Score and its effectiveness in discharge planning.
Methods:
In 370 patients we analyzed the variables hospital stay, destination at discharge, use of healthcare resources and mortality.
Results:
Analysis of the relationship between mortality and the BRASS-Sp index with regard to gender and number of days of stay yielded a hazard ratio of 1.73 (95% CI 1.22-2.46; p=0.002) for male gender and 2.08 (95% CI 1.43-3.04; p<0.001) for the BRASS-Sp score. Patients who continued in case management in Primary Care had a mean BRASS-Sp of 20.97 (standard deviation 6.11), while in the other patients the mean was 19.35 (standard deviation 5.60), p=0.02.
Conclusions:
The BRASS-Sp proved easy-to-use with verified content validity that is effective for screening hospitalized patients by case management nurses.
Keywords: Patient Discharge; Planning; Blaylock Risk Assessment Screening Score; BRASS; Care Management
INTRODUCTION
The improvement of care coordination is a priority for many health systems, especially in the care of complex and fragile patients in which multiple professionals and services participate. The studies carried out in our environment show coordination problems related to inefficiency in the management of resources, loss of continuity in the care processes and decrease in the attention provided. In practice, these problems translate into inappropriate referrals, inadequate use of emergencies and lack of follow-up to patients after being hospitalized 1)(2)(3).
The historical evolution of the health systems, caused a differentiation of the levels of care that were configured as independent plots, with different objectives and interests. In 2002, as of Decree 137/2002 of Support for Andalusian Families, the Case Management model emerged in Andalusia. In both primary and inpatient care, the case management service was assigned to nurses. The goal of these case management nurses is to help the patient and family to navigate the health system efficiently, avoiding duplication and / or discontinuity of care 4)(5)(6).
The management of cases in the hospital usually starts from an episode of hospitalization, and is oriented to internal coordination and primary care for advance planning of discharge. In the opposite direction, in primary care the approach is aimed at improving the resolution capacity, continuity and coordination, the goal is to avoid hospital admissions and promote the maintenance of the person in the community 7).
Hospitalization increases the risk of the patient as a result of a loss of autonomy that leads to greater dependence, especially in the elderly and women 8 . Discharge planning is a nursing intervention, aimed at preventing complications in the transfer of the hospital either to the home or to another institution 9).
To ensure success in the transition between levels of care, it is necessary to detect early on patients who may benefit from specialized discharge planning services by hospital case management nurses (HCMN). We found different validated instruments to identify vulnerable patients, the criteria of fragility that the authors identify are grouped into four categories: medical, functional, mental and sociodemographic 10).
The Blaylock Risk Assessment Screening Score (BRASS) is a tool validated in different countries and in different contexts as a good predictive tool to detect patients who need to be institutionalized at discharge and who are at risk of prolonged stays 11) - (12) - (13) - (14) - (15 . Anese 16 also found that the BRASS index was a good instrument for the classification of hospitalized patients at risk levels at hospital discharge.
The general objective of this work is to assess the effectiveness of the Spanish translation of the BRASS index (BRASS_Sp) in the discharge planning by nurses managing hospital cases.
The specific objectives are:
• Analyze the characteristics of patients included in case management and their caregivers.
• Analyze the relationship between the level of risk, according to the BRASS_Sp index and: mortality, follow-up modality upon discharge and use of health services.
MATERIAL AND METHOD
The design used in this study is a quantitative, longitudinal retrospective design.
SUBJECTS
All the patients included in case management were studied in the Virgen de la Victoria Hospital of Malaga between January 31, 2009 and April 30, 2011. The average age of the patients was 72.6 years (SD 14.05), being the minimum age of 21 years and the maximum of 102 years; 191 (51.6%) were women. The total number of patients was 370, in all of them the BRASS index was used as a qualimetric tool for discharge planning. To assess the effectiveness of the BRASS index in discharge planning, foreign patients with private health insurance and patients from other communities were excluded because they did not have a medical history in Diraya. Patients hospitalized for oncological /palliative processes were also excluded, understanding that they were an element of confusion, leaving a sample of 341 patients.
INSTRUMENT
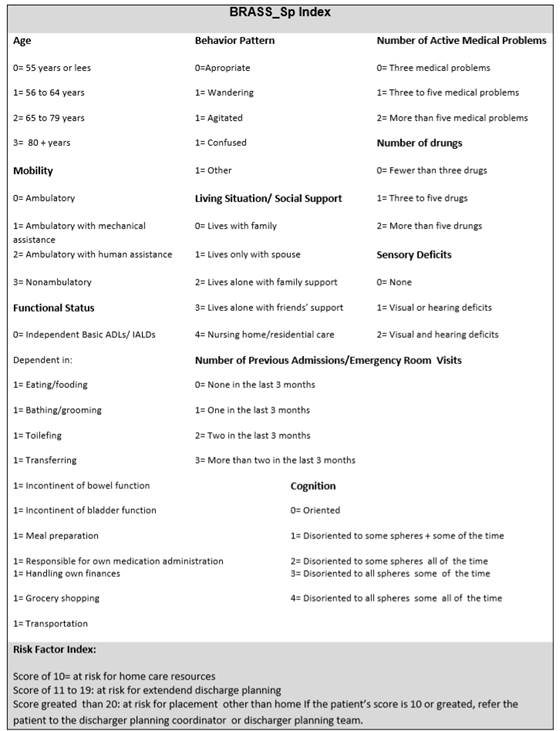
Translation and back-translation of the original version was carried out by bilingual translators with experience in research topics (Image 1 ). The reliability coefficient of the scale was estimated using Cronbach's alpha, whose result was 0.66. In the internal consistency analysis, the highest correlation was between "functional status" and "mobility" and the lowest correlation with "life situation". This tool had previously been used by the HCMN.
The BRASS-Sp index consists of 10 items that establish a score between 0 and 40. The elements that are measured in the questionnaire are: age, social support, cognitive status, functional status, behavior pattern, comorbidity, polypharmacy, hospitalization / stays in recent emergencies, sensory deficit and mobility. Regarding functional status, it measures the patient's ability to perform eight basic and five instrumental activities of daily life.
Based on the score obtained, the patient is classified into three risk groups. Scores greater than 10, suggest that the patient needs coordinated discharge planning to avoid complications at home and / or readmissions.
PROCESS
The patients were referred to the HCMN by the nurse or the referring physician of the patient, if they considered that they were complex patients with high need for care at discharge. The HCMN established the necessary coordination mechanisms and planned the technical needs of the caregiver early. During the study period, the score of the BRASS_Sp index was included in the HCMN care continuity reports.
To assess the validity of the screening and the effectiveness of discharge planning, the outcome variables were studied retrospectively: mortality, followup modality upon discharge, use of health resources: readmissions and emergency attendance. The unique patient health history data available in Diraya was collected.
DATA ANALYSIS
For the analysis of the data, the basic statistics of centralization were used (arithmetic mean, standard deviation [SD] and 95% confidence interval [95% CI]). Depending on the nature of the variables, chi-square test, Student's t test or its corresponding non-parametric tests were used when the distributions did not meet the normality criteria, such as the Mann-Whitney test and the Wilcoxon test. Pearson and Spearman correlations have also been performed according to the normality of distributions. Multivariate regression models were constructed with those variables that in the bivariate analysis showed a significant relationship pattern through Kaplan-Meier curves and proportional hazards analysis through Cox regression.
Although this is a retrospective study, which does not pose risks to the health of the participants, authorization was requested from the Provincial Ethics and Research Commission of Malaga to access the unique digital history of the patients. This Committee authorized this investigation on December 20, 2016.
RESULTS
The results of the descriptive analysis are collected in Tables 1 and 2 .
The scores of the BRASS_Sp index showed an asymmetric distribution that varied between 2 and 37 with an average of 19.9 (SD 6.31). The average number of days of admission was 30.7 (SD 38.4), the average number of days of inclusion in case management was 13.3 (SD 27.5).
Table 1 Characteristics of the patients in the sample
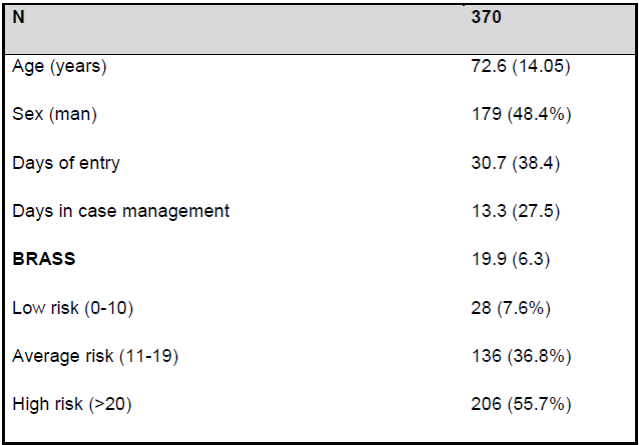
The quantities represent frequencies (%) or medium (DE)
Table 2 Characteristics of the patients in the simple
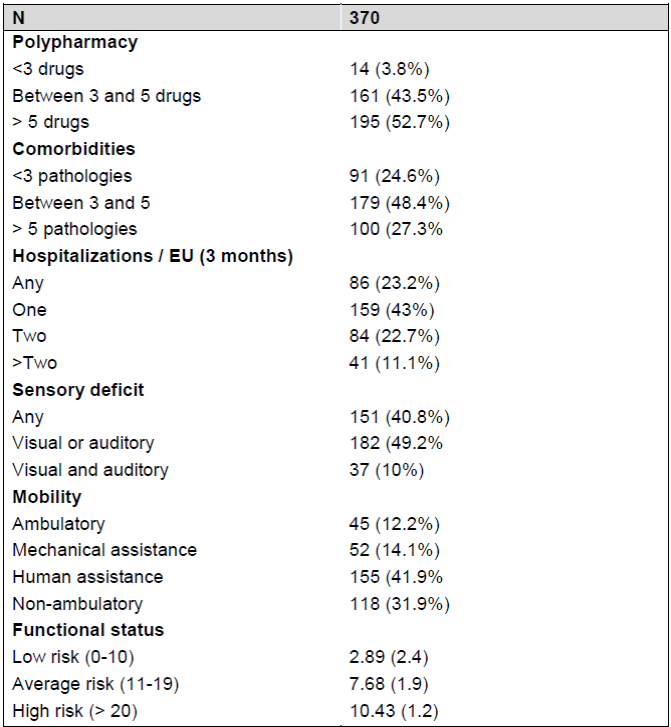
The quantities represent frequencies (%) or medium (DE)
52.7% of patients (195) took more than 5 drugs, 48.4% (179) had between 3-5 pathologies and 43% (159) had gone to the emergency room / hospitalization at least once in the last three months. 41.9% (155) needed human help for ambulation, 49% (182) had some sensory deficit (visual or auditory).
Regarding the functional level, in the patients with low risk the average score was 2.89 (SD 2.40), in the moderate risk was 7.68 (SD 1.91) and high risk 10.43 (SD 1.27). The difference was statistically significant p <0.001.
Regarding the main caregiver, 42.7% were children (158), 28.1% were spouses (104), some family member was 7.6% (28), friends 3.5% (13) and had a formal caregiver 3.5% (13). 11.6% (43) of the patients studied lacked a caregiver.
We identified a group of patients called "very fragile-complex" who would be those who died during admission or who needed to be institutionalized at hospital discharge. Among the very fragile-complex the average score of the BRASSS_Sp index was 21.76 (SD 6.35), while in the others it was 19.59 (SD 6.31). The difference was statistically significant (p = 0.01).
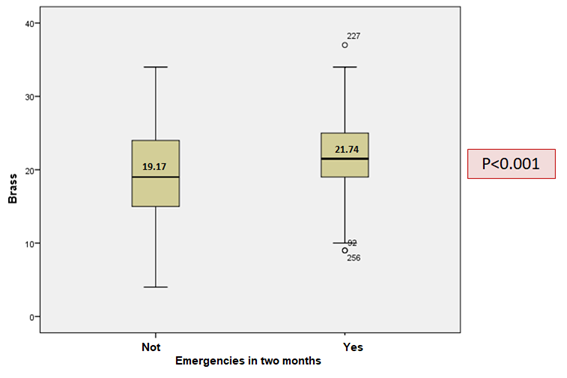
Of the total of 301 patients discharged, they went to the emergency department during the first two months after discharge 108 patients (35.8%). Of which 9.3% (10), they needed to be hospitalized. The average of the BRASS-Sp index in the patients who went to the emergency room was 21.74 (SD 5.23), while in those who did not attend it was 19.17 (SD 6.05). The difference was statistically significant (p <0.001) (Graph 1 ).
We did not find a relationship between a higher score of BRASS_Sp and hospital readmission for any cause at one month or six months after discharge.
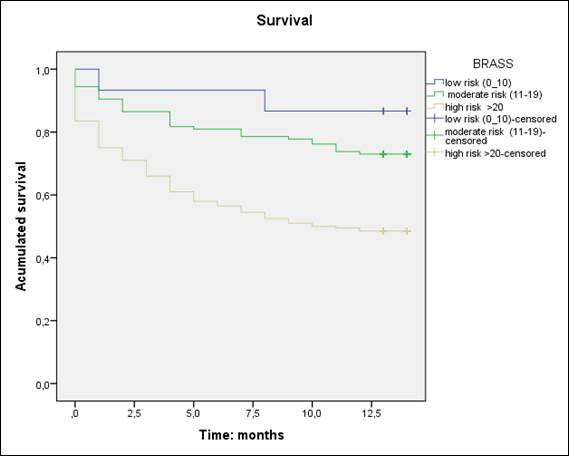
When we analyzed the relationship between mortality and BRASS_Sp index in relation to sex and number of days of admission we found an HR = 1.73 (95% CI from 1.22 to 2.46) with a p = 0.002 for male and a HR = 2.08 (95% CI 1.43 to 3.04) with p <0.001 for the BRASS index score (Graph 2 ).
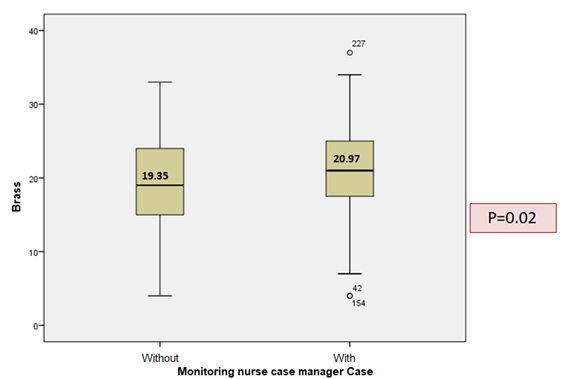
The patients who, after discharge, continued to manage cases in Primary Care, obtained an average of the BRASS_Sp index of 20.97 (SD 6.11), while in the others the average was of 19.35 (SD 5.60). The difference was statistically significant (p = 0.02) (Graph 3 ).
DISCUSSION
The sample of the present study corresponds to patients located in the upper part of the Kaiser pyramid, which are the target population of the HCMN 7). It presents a fragile population, with advanced age and functional deterioration. What justifies that the score in the BRASS-Sp index shows a high value with respect to other published studies 12) - (13) - (14).
The mean number of days of hospitalization was similar to that published for high-risk patients 14) - (15) - (16). There is a gap between days of inclusion in case management and hospitalization, which suggests that a significant proportion of patients were referred to case management due to functional deterioration during admission.
Regarding the main caregiver, we observed a clear gender bias; In the case that the caregiver was the spouse, 79 (21.4%) were wives, compared to 25 (6.8%) who were husbands; in the case that the caregiver was a descendant 125 (33.8%) were daughters compared to 33 (8.9%) who were children. Our results coincide with that published by García-Calvente 17 , who argues that the typical profile of people who assume the role of primary caregiver in Spain is that of a woman, responsible for domestic tasks, direct family (usually mother, daughter or wife) and who lives with the person they care for.
To evaluate the validity of the screening of the BRASS_Sp index, we explored the association between the score obtained in the questionnaire and the clinical results observed. We found a relationship between risk level in the BRASS_Sp index and the results: mortality, emergency attendance and follow-up modality in Primary Care.
We found that the patients with the highest score of the BRASS_Sp index presented higher mortality per year. This data coincides with that published by Dagani 12 , who found a relationship between risk level according to the BRASS index and mortality at six months after discharge. Patients who died during admission or were institutionalized at discharge also had a high risk level. The identification of the final trajectory of life is complex in non-oncological patients, because most diseases present with more or less severe decompensation followed by periods of clinical stability 18) - (19 . In general, this final stage is related to comorbidity, but the prognosis of patients also depends on the situation of fragility and functional status, aspects assessed with the BRASS-Sp index 20) - (21).
Mistiaen 14 , found that the patients with the highest score in the BRASS index had worse functional and health status after discharge and that they went to the emergency department more. In our study, patients who went to the emergency room within two months after discharge were also at high risk according to the BRASS_Sp index. This data can be justified because, in addition to functional impairment, the BRASS_Sp index assesses factors that have proven to be predictors of complications in the community.
Finally, we found that patients who continued in case management in Primary Care after hospital discharge had a higher score in the BRASS_Sp index. This corresponds to patients with high complexity of care, who in the Andalusian Health System are included in the portfolio of services of case management nurses 7 .
Study Limitations
The most important limitation of this study is the absence of a control group, since it would have allowed us to draw conclusions about the predictive validity of the BRASS-Sp index and to determine its agreement with other tests of assessment of daily life activities.
The internal consistency of the instrument, although similar to other published studies, is at a weak level of reliability 13) - (14 . We consider, like Panella 22 , that it is necessary to modify the items that show a lower degree of correlation.
CONCLUSIONS
In conclusion, our data suggest that the BRASS_Sp index may be a useful tool for the screening of hospitalized patients, in order to identify those who are at greater risk and need discharge planning. The general vision that this tool provides of the patient, allows the HCMN to plan the care in the inter-level transfer in an individualized way.
The BRASS_Sp index, in addition to the functional capacity of the patient, assesses aspects related to comorbidity, polypharmacy and social situation. This information is essential to guide and develop a functional recovery plan for the patient, so that future investigations that analyze the results of incorporating the BRASS_Sp index into clinical practice in the hospitalization units would be interesting. Early detection of fragile or vulnerable patients can have positive effects.
REFERENCIAS
1. Terraza Núñez R, Vargas Lorenzo I, Vázquez Navarrete ML. La coordinación entre niveles asistenciales: una sistematización de sus instrumentos y medidas. Gaceta Sanitaria. 2006;20(6):485-95. [ Links ]
2. Martín Martínez MAM, Carmona R, Mayor EE, Blázquez MR, Santamera AS. Factores asociados a reingresos hospitalarios en pacientes de edad avanzada. Atención primaria: Publicación oficial de la Sociedad Española de Familia y Comunitaria. 2011;43(3):117-24. [ Links ]
3. Nguyen OK, Makam AN, Clark C, Zhang S, Xie B, Velasco F, et al. Predicting all-cause readmissions using electronic health record data from the entire hospitalization: Model development and comparison. J Hosp Med.2016;11(7):473-80. [ Links ]
4. Morales-Asencio J.M. Gestión de casos y cronicidad compleja: conceptos,modelos, evidencias e incertidumbres. Enferm Clin. 2014;24(1):23-34. [ Links ]
5. Agencia de Calidad Sanitaria de Andalucía. Manual de competencias profesionales. Enfermero/a Gestor/a de Casos. Agencia de Calidad Sanitaria de Andalucía. Consejería de Igualdad Salud y Políticas Sociales. 2015. [ Links ]
6. Perteguer-Huerta, I. La gestión de casos: haciendo camino. Enfermería Clínica. 2014; 24:159-161. [ Links ]
7. Servicio Andaluz de Salud. Modelo de Gestión de Casos del Servicio Andaluz de Salud: Guía de reorientación de las prácticas profesionales de la Gestión de casos en el Servicio Andaluz de Salud. [Internet] 2017. [citado 20 de noviembre 2017]. Disponible en: https://www.picuida.es/guia-reorientacion-las-practicas-profesionales-la-gestion-casos-servicio-andaluz-salud/ [ Links ]
8. De Saint-Hubert M, Schoevaerdts D, Cornette P, D'Hoore W, Boland B, Swine C. Predicting functional adverse outcomes in hospitalized older patients: a systematic review of screening tools. J Nutr Health Aging. 2010;14(5):394-9. [ Links ]
9. Anthony MK, Hudson-Barr D. A Patient-Centered Model of Carefor Hospital Discharge. Clin Nurs Res. 2004;13(2):117-36. [ Links ]
10. Alonso Galbán P, Soberats S, José F, Navarro D-C, María A, Carrasco García M, et al. Envejecimiento poblacional y fragilidad en el adulto mayor. Revista Cubana de Salud Pública. 2007;33(1):0-0. [ Links ]
11. Blaylock A, Cason CL. Discharge planning predicting patients' needs. J Gerontol Nurs. 1992;18(7):5-10. [ Links ]
12. Dagani J, Ferrari C, Boero ME, Geroldi C, Giobbio GM, Maggi P. A prospective, multidimensional follow-up study of a geriatric hospitalized population: predictors of discharge and well-being. Aging. Clin Exp Res. 2013;25(6):691-701. [ Links ]
13. DalMolin A, Gatta C, Derossi V, Guazzini A, Cocchieri A, Vellone E. Hospital Discharge: Results Froman Italian Multicenter Prospective Study Using Blaylock Risk Assessment Screening Score. Int J Nurs Terminol Knowledge. 2014;25(1):14-21. [ Links ]
14. Mistiaen P, Duijnhouwer E, Prins-Hoekstra A, Ros W, Blaylock A. Predictive validity of the BRASS index in screening patients with post-discharge problems. Blaylock Risk Assessment Screening Score. J Adv Nurs. 1999;30(5):1050-6. [ Links ]
15. Signorini G, Dagani J, Bulgari V, Ferrari C, Girolamo G. Moderate efficiency of clinicians' predictions decreased for blurred clinical conditions and benefits from the use of BRASS index. A longitudinal study on geriatric patients' outcomes. Journal of Clinical Epidemiology. 2016; 69:51-60. [ Links ]
16. Anese F. L'utilizzo della scala brass per la continuita assitenziale: indice predittivo per l'attivazione della cot [Laurea triennale]. 2015. Actualizado el 5 de noviembre de 2017, a partir de http://tesi.cab.unipd.it/50794/ [ Links ]
17. García-Calvente M del M, Mateo-Rodríguez I, Eguiguren AP. El sistema informal de cuidados en clave de desigualdad. GacSanit. 2004;18:132-9. [ Links ]
18. Consejería de Salud. Plan Andaluz de Atención Integrada a Pacientes con Enfermedades Crónicas 2012-2016. [Internet].2012.[consultado 20 noviembre 2017]. Disponible en: http://www.juntadeandalucia.es/export/drupaljda/PlanAtencEECC.pdf [ Links ]
19. Martínez-Sellés M, Vidán MT, López-Palop R, Rexach L, Sánchez E, Datino T. El anciano con cardiopatía terminal. Revista Española de Cardiología.2009; 62(4): 409-421. [ Links ]
20. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, McBurnie MA. Frailty in Older Adults Evidence for a Phenotype. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2001; 56(3):146-157. [ Links ]
21. Martínez García MD, García García I, Schmidt Río-Valle J, Vellido González MD. Características sociosanitarias de los pacientes atendidos por las enfermeras gestoras de casos hospitalarios. Metas de Enfermería. 2013; 16(4):19-26 [ Links ]
22. Panella L, La Porta F, Caselli S, Marchisio S, Tennant A. Predicting the need for institutional care shortly after admission to rehabilitation: Rasch analysis and predictive validity of the BRASS Index. European Journal of Physical and Rehabilitation Medicine. 2012; 48(3):443-454 [ Links ]
Received: October 09, 2017; Accepted: December 19, 2017











 text in
text in