My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.19 n.59 Murcia Jul. 2020 Epub Aug 10, 2020
https://dx.doi.org/10.6018/eglobal.402691
Originals
Acquisition of Palliative Care Knowledge Through a Transversal Approach in Nursing Studies
1 Unidad de Hospitalización Oncológica, Consorcio Hospitalario Provincial de Castellón, Castellón España.
2 Unidad Predepartamental de Enfermería, Universitat Jaume I, Castellón. España. afolch@uji.es
3 Unidad de Oncohematología, Hospital Universitario General de Castellón, Castellón. España.
The inclusion of palliative care content in university curricula has been gradual. Due to the recent incorporation of palliative care as a subject, an evaluation is necessary in order improve the education of our future health professionals. The objective of this study was thus to assess palliative care knowledge in nursing students at Jaume I University after the transversal inclusion of palliative care content throughout the program, culminating in a subject of an obligatory nature.
Method:
This observational cross-sectional study was undertaken over the 2017/2018 academic year using the Palliative Care Quiz for Nursing. A descriptive and comparative analysis of the quantitative and qualitative global variables was performed with respect to correct/incorrect responses. Statistical significance was set at p <0.05.
Results:
The sample included 155 participants, with a mean age of 22.21±6.61 years. Females (n=124) were predominant in the sample (80%). The domain which received the highest number of correct responses was related to the control of pain and symptoms (69.1%) and the domain which received the highest number of incorrect responses was related to philosophy and principles (46.9%). Academic year and prior palliative care experience explained 16% of the variance in knowledge.
Conclusions
Through our results, we observed that palliative care education, implemented in a transversal manner and with the completion of compulsory subject in the fourth year, was effective in nursing students, with 63% achieving good scores with respect to palliative care knowledge.
Key words: Nursing Students; Palliative Care; Education; Nursing Care
INTRODUCTION
In recent decades the number of patients with chronic and degenerative diseases has increased1. These diseases are characterized by an irreversible progression which can occur at different rates, leading to a terminal stage with a high demand for care1. It is necessary to adapt health care to this patient profile2. Assistance in this context is based on offering the best quality of life during the patient´s lifetime. This is known as palliative care (PC)3.
Due to medical advancements, the capacity to artificially extend the lifespan of the patient has been improved. However, with this increase in longevity there is also a reduction in quality of life4). In addition, healthcare teams face an ethical dilemma in decision-making with respect to the therapeutic possibilities that can be offered to the patient. This makes the training of health personnel with respect to PC indispensable, as has been endorsed by the World Health Organization (WHO) through the PC strategy4, and by the main scientific societies5.
Despite an awareness of the importance of PC in society, the inclusion of PC content in health curricula at the university level has been gradual5)(6)(7)(8)(9. A certain level of heterogeneity and variability between different countries has also been observed10)(11)(12, and the current model of teaching and practice is considered insufficient13. Although the situation is changing, the necessary attention is still not being given to issues related to death and the process of dying14.
Nurses have a significant presence in the context of palliative care. They also present with some of the greatest deficits in training as compared to professionals from other fields such as medicine10. In Spain, PC training is included in the undergraduate programs of all nursing faculties15. However, this training is provided heterogeneously at the undergraduate and postgraduate levels and in continued education courses, with variability in the number of hours and content. It is important to assess whether, through this training, the necessary knowledge is being provided in order to address deficiencies.
Since the introduction of undergraduate nursing studies at Jaume I University (UJI) in 2012, there has been a great commitment to the implementation of education on palliative care. With a novel and innovative curriculum, PC knowledge is imparted in a transversal manner through theory sessions and clinical practice in healthcare settings, culminating in a palliative care subject for nursing students in the fourth year of the program.
Taking into account the aforementioned and given the relatively recent introduction of nursing studies at the UJI, there is a need to assess the level of knowledge that is acquired by graduates through this transversal approach. In this manner, deficiencies in terms of knowledge acquisition with respect to PC can be identified and resolved, making for better healthcare professionals.
MAIN OBJECTIVE
To assess palliative care knowledge levels in nursing students at Jaume I University using the Spanish version of the Palliative Care Quiz for Nurses (PCQN) over the 2017/2018 academic year.
SPECIFIC OBJECTIVE
To identify palliative care knowledge in three domains (principles, psychosocial aspects, and pain and symptom control) and the relationship with sociodemographic variables, academic year, and prior palliative care experience.
METHODOLOGY
Design
Observational, cross-sectional study, with blinded data analysis, using a self-administered questionnaire over the 2017/2018 academic year, in the months of February to March 2018.
Context
Educational, with first-, second-, third-, and fourth-year undergraduate nursing students at Jaume I University.
Population and Sample
All students enrolled in any academic year of the four-year nursing program were selected, with an overall study population of 240 students.
In order to select the sample from the study population, the sample size was calculated using the Epidat 4.1 computer program. The sample size was calculated using a proportion of n=240 students, assuming a confidence level of 95% and a margin of error of 5%. A global sample of 148 individuals was obtained, with 37 students per academic year.
Inclusion criteria
Enrolment in the Nursing Degree program at Jaume I University, in any of its four corresponding academic years.
Exclusion criteria
Not signing the informed consent form or not being present in the classroom on the day of the assessment.
Variables
Primary variable
Knowledge on PC: This was assessed using the Palliative Care Quiz for Nurses Questionnaire, which consists of 20 items of a dichotomous nature (true or false). The English version has been validated in Spanish in nursing students, with a Cronbach´s alpha of 0.6715.
The 20 items are structured with respect to the three domains of PC that healthcare personnel must know about: the philosophy and principles of PC (four questions: 1, 9, 12, and 17); pain and symptom control (13 questions: 2, 3, 4, 6, 7, 8, 10, 13, 14, 15, 16, 18, and 20); and psychosocial aspects of PC (three questions: 5, 11, and 19). See Table 2 15.
For data interpretation, the following values were established based on the midpoint of the possible results for each of the three aspects or domains of PC:
Philosophy and principles (4 items)
Yes > 2 correct responses
No < 2 correct responses
Pain control (13 questions)
Yes > 6 correct responses
No < 6 correct responses
Psychosocial aspects (three items)
Yes > 2 correct responses
No 0-1 correct responses
Secondary variables
Sociodemographic: age and sex (male/female). Academic year: first, second, third, and fourth. Fourth-year students were those who had taken the compulsory PC subject that forms part of the Jaume I University curriculum. These students were considered to have acquired the necessary knowledge for competency in PC. Students who had not completed PC training but who were taking subjects corresponding to various academic years were considered to belong in the academic year of the class they were taking on the day of the survey. Palliative care experience (yes/no): First-year students were excluded from answering this question, given that clinical practice within the Jaume I University nursing curriculum begins during the second year of study.
Data Collection
For data collection, an ad hoc questionnaire was prepared containing the variables under study. To obtain the data, one teacher for each academic year was contacted via email, and permission was requested in order to administer the questionnaires during teaching hours. In each of the classes a brief explanation about the objective of the study was given, as well as basic instructions for completion of the questionnaire. The questionnaire, information sheet, and informed consent form were distributed, and questions were subsequently answered during the completion and collection of the questionnaire and consent forms.
Statistical analysis
A descriptive analysis of the characteristics of the population (sociodemographic information, academic year, and experience in PC during clinical practice) was undertaken, as well as a description of results by question and categorization (yes/no) in domains based on the established values. Results were presented as percentages and means (x) ± standard deviation (SD). A comparative analysis of the domains with respect to the studied variables (sociodemographic information, academic year, and experience in PC during clinical practice) was also undertaken using the Chi-squared and Fisher´s exact tests. For the generation of a linear regression model using the introduction method, all variables which had reached statistical significance (<0.05) in the Chi-squared test and Fisher´s exact test were selected. For interpretation purposes all p-values were presented, setting statistical significance at p <0.05. For the statistical study, the SPSS v.23 software package for Windows was used.
Ethical aspects
The study was approved by the Bioethics Committee at Jaume I University, and was carried out in accordance with the specific norms of the Declaration of Helsinki and ethical principles of biomedical research. The personal data of subjects participating in the study were processed in accordance with the provisions of Organic Law 15/1999 of December 13 on Protection of Personal Data, and Law 41/2002 of November 14 on the Regulation of Patient Autonomy and Rights and Obligations Regarding Clinical Information and Documentation. The anonymity of the participants and confidentiality of data were guaranteed. The data will not be accessible to individuals outside of the study. All students were informed and signed an informed consent form in order to be part of the study.
RESULTS
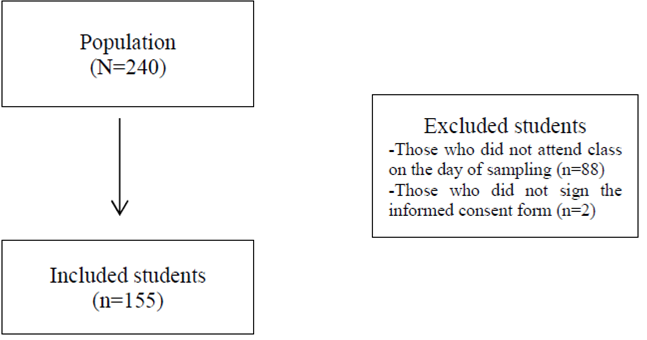
The study population was composed of 240 students. After applying the exclusion criteria 155 participants remained due to some students not being present in class during administration of the questionnaires (n=83) or not signing the informed consent form (n=2). See Figure 1.
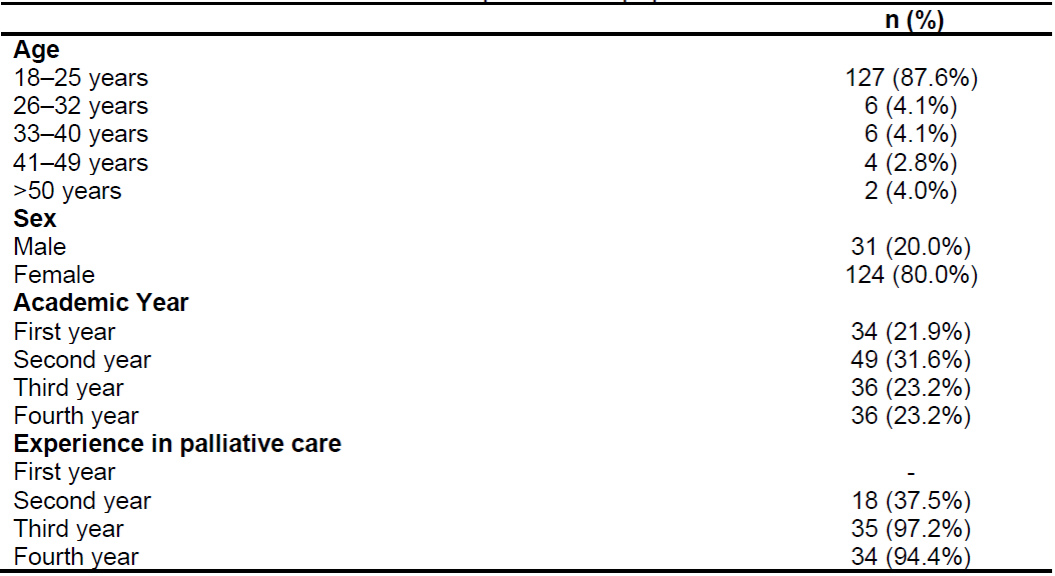
The mean age of the 155 selected students was 22.2±6 years, with most participants aged between 18 and 25 years (n=127, 87.6%). In terms of sex, 80% (n=124) of participants were women. With regard to academic year, second-year students comprised the largest group, representing 31.6% (n=49) of the sample. In the 2017/2018 academic year, third-year students were the group most likely to have had experience in palliative care (n=35, 97.2%). See Table 1.
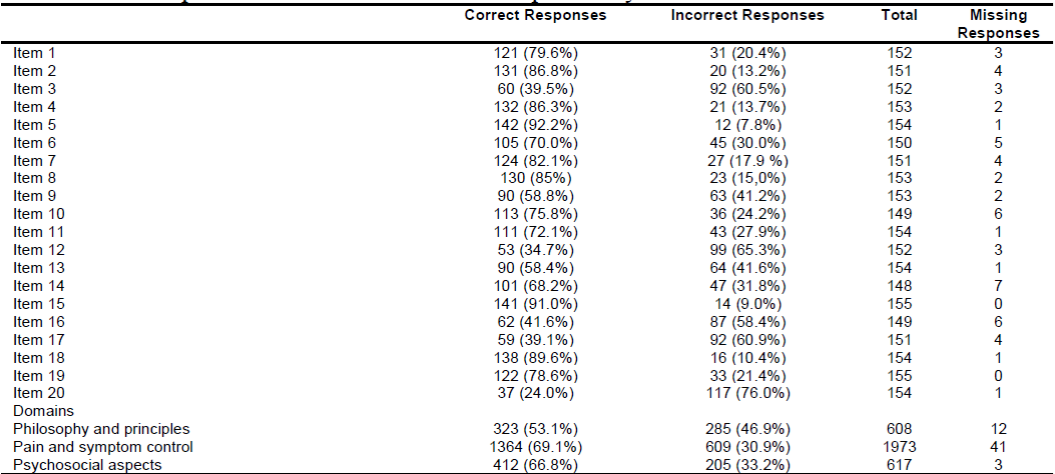
The items that received the highest numbers of correct responses were item 5 "It is crucial for family members to remain at the bedside until death occurs" (n=142, 92.2%), and item 15 "Suffering and physical pain are synonymous" (n=141, 91.0%). In contrast, the items which received the highest numbers of incorrect responses were item 20 "The pain threshold is reduced by anxiety or fatigue" (n=117, 76.0%) and item 12 "the philosophy of PC is compatible that of active treatment" (n=99, 65.3%).
Items relating to the domain of pain and symptom control received the highest number of correct responses (n=1364, 69.1%), whereas items related to the philosophy and principles of PC received the highest number of incorrect responses (n=285, 46.9%). See Table 2.
Table 2. Description of correct and incorrect responses by items and domains.
Item 1. Palliative care is appropriate only in situations where there is evidence of a downhill trajectory or deterioration.
Item 2. Morphine is the standard used to compare the analgesic effect of other opioids.
Item 3. The extent of the disease determines the method of pain management.
Item 4. Adjuvant therapies are important in managing pain.
Item 5. It is crucial for family members to remain at the bedside until death occurs.
Item 6. During the last days of life, drowsiness associated with electrolyte imbalance can decrease the need for sedation.
Item 7. Drug addiction is a major problem when morphine is used on a long-term basis for the management of pain.
Item 8. Individuals taking opioids should also follow a bowel regime.
Item 9. The provision of palliative care requires emotional detachment.
Item 10. During the terminal stages of an illness, drugs that can cause respiratory depression are appropriate for the treatment of severe dyspnea.
Item 11. Men generally reconcile their grief faster than women.
Item 12. The philosophy of palliative care is compatible with that of active treatment.
Item 13. The use of placebos is appropriate in the treatment in some types of pain.
Item 14. In high doses, codeine causes more nausea and vomiting than morphine.
Item 15. Suffering and physical pain are synonymous.
Item 16. Pethidine hydrochloride is not an effective pain reliever in the control of chronic pain.
Item 17. The accumulation of losses renders burnout ineviTable for those who seek work in palliative care.
Item 18. Manifestations of chronic pain are different from those of acute pain.
Item 19. The loss of a distant or contentious relationship is easier to resolve than the loss of one that is close or intimate.
Item 20. The pain threshold is lowered by anxiety or fatigue
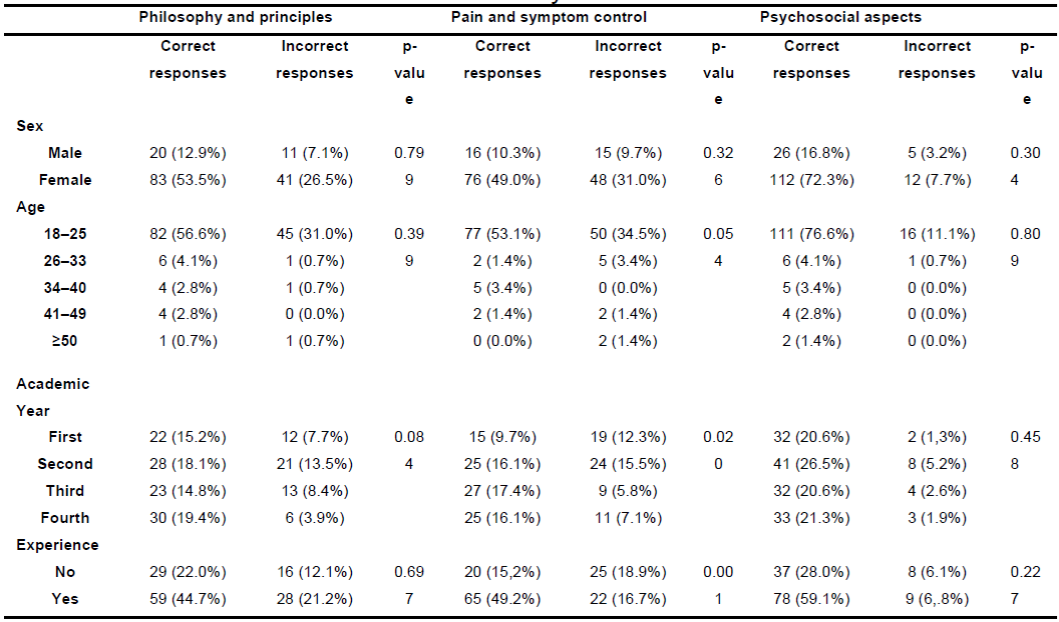
With regard to the bivariate analysis, both sexes presented the greatest number of correct answers in the domain related to psychosocial aspects (16.8% vs. 72.3%) and the greatest number of errors in the domain related to pain control and symptoms (9.7% vs. 31.0%), with no significant differences. In terms of age, students aged between 18 and 25 years more often responded correctly to items on psychosocial aspects (76.6%); however, this group showed a greater number of errors with respect to knowledge of pain and symptom control methods (34.5%), with close to significant differences in the knowledge of pain control methods depending on age range (p=0.054).
In terms of academic year, all students obtained the greatest number of correct responses in relation to psychosocial aspects, most notably second-year students (26.5% of correct responses). However, these students also responded incorrectly most often in relation to statements regarding pain and symptom control (15.5%), with significant differences (p=0.020).
Another of the aspects analyzed was clinical experience with palliative patients, which was found to improve knowledge on psychosocial aspects (59.1%) and significantly improve knowledge on pain and symptom control measures (49.2%) p=0.001. See data in Table 3.
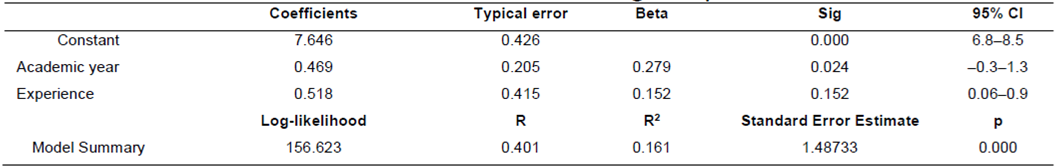
To better understand the aspects that affect overall knowledge of PC, a predictive model (p=0.000) was developed that was able to explain 16% of the variance. It was found that the more advanced the academic year, the greater the knowledge score obtained, with a statistically significant relationship (p=0.024). Prior experience with palliative care patients also featured in the model, and although the relationship not significant, it was observed that the greater the prior experience in PC, the higher the level of knowledge (p=0.152). See data in Table 4.
DISCUSSION
For the continuous improvement of our future health professionals, the implementation and evaluation of teaching methods is fundamental. The transversal inclusion of PC content for nursing students, culminating in a compulsory subject in the fourth year of the program, was observed to be effective in this study, as 63% of students showed a good success rate with respect to knowledge on the subject. In comparison, in a study by the University of Valencia a success rate of 42.1% was reported16.
Thus, the analysis carried out with respect to each of the domains showed that students scored best with respect to pain and symptom management (69.1%), followed by psychosocial aspects (66.8%), and philosophy and ethical principles (53.1%), although the highest number of correct responses was obtained for an item on life philosophy related to family, where the students considered it essential for family members to remain at the bedside until the death of the patient, placing importance on the family in PC. This finding contradicts those of other studies which reported that students did not take family into account in the context of palliative care17.
Notably, no relationship between PC knowledge and age and sex was found, coinciding with the results of Pastrana et al.10 in medical and nursing students. These results are in conflict with those of other studies which suggest that female sex18)(19)(20 and younger age20 are factors related to reduced knowledge on palliative care due to the fear that these individuals experience. This is possibly related to other variables which do show a relationship, such as experience with palliative care patients, where results showed that greater fear was associated with less experience18. In the case of academic year, in conflict with our results not all studies have found that level of knowledge is related to the year of study and experience, with some authors reporting that knowledge of PC was not linked to the experience of having seen a family member, patient, or other person die19)(20. Several studies have found that general knowledge improvement with respect to PC favors the control of symptoms (especially pain), and improves the management of opioids and refractory symptoms during the clinical practice of both medical and nursing students12)(21)(22)(23. Improved PC knowledge and skills also enhance communication with dying patients and their families, as well as self-esteem24.
These results have limitations due the small sample size, and there is a need to use data from other nursing faculties to obtain more conclusive results.
CONCLUSIONS
The knowledge levels of nursing students at Jaume I University in the 2017/2018 academic year were assessed using the Palliative Care Quiz for Nursing (PCQN) instrument, with 63% achieving good scores in this regard. The domain with the highest number of correct responses was related to pain and symptom control (69.1%) and the domain with the highest number of errors was related to philosophy and principles (46.9%).
Knowledge on palliative care was not related to philosophy, ethical principles, or psychosocial aspects; however, a greater level of knowledge on palliative care was related to better pain and symptom management. Academic year and prior palliative care experience explained 16% of the variance in knowledge.
REFERENCIAS
1. Ruiz-Íñiguez R, Bravo Sobrino N, Peña Ibáñez F, Navarro Siguero N, Seco Martínez A, Carralero Montero A. Intervención enfermera sobre la calidad de vida en personas con cuidados paliativos domiciliarios: revisión sistemática. Med Paliativa [Internet]. 2017 Apr 1 [cited 2018 Dec 4];24(2):72-82. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1134248X15000221 [ Links ]
2. Gortmaker SL, Sappenfield W. Chronic Childhood Disorders: Prevalence and Impact. Pediatr Clin North Am [Internet]. 1984;31(1):3-18. Available from: http://www.sciencedirect.com/science/article/pii/S0031395516345321 [ Links ]
3. Nagore-Ancona F, De Los Santos-Rodríguez M, Pech-George R, Esperón-Hernández R, Fernández-Pérez R, Aguilar-Franco L. Evaluación de la competencia en cuidados paliativos en estudiantes de medicina Evaluation of palliative care competency in medical students [Internet]. Vol. 20, 133 www.fundacioneducacionmedica.org FEM. 2017 [cited 2018 Dec 4]. Available from: www.fundacioneducacionmedica.org [ Links ]
4. Stjernsward J, Foley KM, Ferris FD. The public health strategy for palliative care. J Pain Symptom Manage [Internet]. 2007 May;33(5):486-93. Available from: https://www.jpsmjournal.com/article/S0885-3924(07)00122-4/fulltext [ Links ]
5. Boceta Osuna J. Grupo de trabajo SECPAL sobre formación médica en medicina paliativa en la universidad española. Med Paliativa [Internet]. 2016 Apr 1 [cited 2018 Dec 4];23(2):53-4. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1134248X16000082 [ Links ]
6. Cruz-Quintana F, García-Caro MP. SOS___ dejadme morir?: ayudando a aceptar la muerte / F. Cruz Quintana, M.P. García Caro. Pirámides. Madrid; 2007. [ Links ]
7. Ignorosa-Nava CA, González-Juárez L. Cuidados paliativos para una muerte digna. Estudio de un caso. Enfermería Univ [Internet]. 2014 Jul 1 [cited 2018 Dec 4];11(3):110-6. Available from: https://www.sciencedirect.com/science/article/pii/S1665706314726740 [ Links ]
8. Bermejo JC, Villacieros M, Hassoun H. Actitudes hacia el cuidado de pacientes al final de la vida y miedo a la muerte en una muestra de estudiantes sociosanitarios. Med Paliativa [Internet]. 2018 Jul [cited 2018 Dec 4];25(3):168-74. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1134248X18300065 [ Links ]
9. Vaquero Cruzado JA, Centeno Cortés C. Panorama actual de la enseñanza de medicina paliativa en la universidad española. Med Paliativa [Internet]. 2014;21:3-8. Available from: http://www.elsevier.es/es/linksolver/ft/pii/S1134248X13000517 [ Links ]
10. Pastrana T, de Lima L, Wenk R. Estudio multicéntrico sobre la comodidad y el interés en cuidados paliativos en estudiantes de pregrado en Colombia. Med Paliativa [Internet]. 2015 Oct 1 [cited 2018 Dec 4];22(4):136-45. Available from: https://www.sciencedirect.com/science/article/pii/S1134248X1400130X [ Links ]
11. Ilse B, Hildebrandt J, Posselt J, Laske A, Dietz I, Borasio GD, et al. Palliative Care teaching in Germany - concepts and future developments. GMS Z Med Ausbild. 2012;29(3):Doc 47. [ Links ]
12. Carmona Espinazo F, López Sáez JB, Torres Recio MJ, Lorenzo Peñuelas A. El reto de comenzar a impartir cuidados paliativos en una facultad de medicina. ¿Es útil esta materia para los futuros médicos? Med Paliativa [Internet]. 2018 Jan [cited 2018 Dec 4];25(1):1-6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1134248X17300459 [ Links ]
13. Marti-Garcia C, Garcia-Caro MP, Schmidt-Riovalle J, Fernández-Alcántara M, Montoya-Juárez R, Cruz-Quintana F. Formación en cuidados paliativos y efecto en la evaluación emocional de imágenes de muerte. Med Paliativa [Internet]. 2016 Apr 1 [cited 2018 Dec 4];23(2):72-8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1134248X14000251 [ Links ]
14. Weber M, Schmiedel S, Nauck F, Alt-Epping B. Knowledge and attitude of final - year medical students in Germany towards palliative care - an interinstitutional questionnaire-based study. BMC Palliat Care [Internet]. 2011;10:19. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3235960/pdf/1472-684X-10-19.pdf [ Links ]
15. Wenk R, de Lima L, Mutto E, Berenguel M del R, Centeno C. Encuentro sobre educación de cuidado paliativo en Latinoamérica. Recomendaciones sobre enseñanza en el pregrado y en el primer nivel de atención de salud. Med Paliativa [Internet]. 2016 Jan 1 [cited 2018 Dec 4];23(1):42-8. Available from: https://www.sciencedirect.com/science/article/pii/S1134248X14000287 [ Links ]
16. Chover-Sierra E, Martínez-Sabater A, Lapeña-Moñux Y, Asociado P. Conocimientos en cuidados paliativos de los profesionales de enfermería de un hospital español. Rev Lat Am Enfermagem [Internet]. 2017 [cited 2018 Dec 10];25(e2847). Available from: www.eerp.usp.br/rlae [ Links ]
17. Fortín Magaña MA, Portillo Santamaría K, Gómez Casanovas J, López Saca M. Enseñanza de los cuidados paliativos en las escuelas de medicina de El Salvador. Educ Médica [Internet]. 2018; Available from: http://www.sciencedirect.com/science/article/pii/S1575181317301808 [ Links ]
18. Robbins RA. Death competency: A study of hospice volunteers. Death Stud [Internet]. 1992 Nov [cited 2018 Dec 10];16(6):557-69. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10122686 [ Links ]
19. Boceta Osuna J, Galán González-Serna JM, Gamboa Antiñolo FM, Muniain Ezcurra MÁ. Factores sociodemográficos que influyen en la ansiedad ante la muerte en estudiantes de medicina. Educ Médica [Internet]. 2017 Jul 1 [cited 2018 Dec 4];18(3):179-87. Available from: https://www.sciencedirect.com/science/article/pii/S157518131630105X [ Links ]
20. Morillo-Martín MS, Galán González-Serna JM, Arroyo Rodríguez A, Romero Serrano R. Factores sociodemográficos que influyen sobre la ansiedad ante la muerte en estudiantes de Enfermería. Med Paliativa [Internet]. 2016 Jul 1 [cited 2018 Dec 4];23(3):113-21. Available from: https://www.sciencedirect.com/science/article/pii/S1134248X14000263 [ Links ]
21. Sanz-Rubiales A, Del Valle ML, González C, Hernansanz S, García C, Sánchez T, et al. Formación en el uso de opioides: ¿repercute en la práctica diaria? [Internet]. Vol. 8, Rev. Soc. Esp. Dolor. 2001 [cited 2018 Dec 10]. Available from: http://revista.sedolor.es/pdf/2001_07_02.pdf [ Links ]
22. Sánchez-Sánchez RM, Pernía J V, Calatrava J. Tratamiento del dolor en los estudios de enfermería. Rev Soc Esp Dolor [Internet]. 2005 [cited 2018 Dec 10];12:81-5. Available from: http://scielo.isciii.es/pdf/dolor/v12n2/original2.pdf [ Links ]
23. Florez SP, Tovar MB, Leon MX, Villegas K, Villamizar D del P, Granados CE. Caracterización del conocimiento en cuidado paliativo pediátrico y percepción debarreras por parte de los pediatras y residentes de pediatría. Med Paliativa [Internet]. 2015 Oct [cited 2018 Dec 4];22(4):127-35. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1134248X14000469 [ Links ]
24. Schulz C, Möller MF, Seidler D, Schnell MW. Evaluating an evidence-based curriculum in undergraduate palliative care education: piloting a phase II exploratory trial for a complex intervention. BMC Med Educ [Internet]. 2013;13(1):1. Available from: https://doi.org/10.1186/1472-6920-13-1 [ Links ]
Received: November 11, 2019; Accepted: February 18, 2020











 text in
text in