My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.20 n.63 Murcia Jul. 2021 Epub Aug 02, 2021
https://dx.doi.org/10.6018/eglobal.448771
Originals
Knowledge and vulnerability of participants in the Syphilis Tent: university extension action
1 Profesor Adjunto de la Facultad de Enfermería de la Universidad Federal del Estado de Rio de Janeiro (UERJ). Doctora en Enfermería y Biociencias por la Universidad Federal del Estado de Rio de Janeiro (UNIRIO). Brasil. marcelle_sfg@hotmail.com
2 Enfermera por la Universidad Federal del Estado de Rio de Janeiro . Brasil.
3 Discente de enfermería y Bolsista del Programa Institucional de Bolsas de Iniciación Científica (PIBIC) UNIRIO. Brasil.
4a Máster en Enfermería por la UNIRIO. Discente del curso de doctorado del Programa de Posgraduación de Enfermería y Biociencias (PPGENFBIO) da UNIRIO. Profesora de Enfermería en la FAETEC. Brasil.
4bProfesora de Enfermería en la Universidad Estácio de Sá. Brasil.
5 Máster en Dermatología por la UNIRIO. Discente del curso de doctorado del PPGENFBIO de UNIRIO. Profesor Adjunto de Dermatología de la UNIRIO. Brasil.
6 Doctora en Enfermería con Estancia Pos-Doctoral en la Universidad Federal de Bahia. Profesora Titular de la Escuela de Enfermería Alfredo Pinto/UNIRIO. Brasil.
Introducion:
Study aims to describe and evaluate the socioeconomic profile, risk factors, sexual practices and the knowledge of the participants of the university extension activity Syphilis Tent about this infection.
Method:
Descriptive-transversal research, with 1000 participants, between october 2016 and december 2019, at the University Campusand University Hospital of the State of Rio de Janeiro. To collect the data, a semi-structured questionnaire was used, applied at the time of the educational activity.
Results:
Most participants were women (72%), white (41%), young adults (55%), single (51%), incomplete higher education (37%) and income below three minimum wages (48%), heterosexual (86%), sexually active (75%) and single sexual partner (88%). The most prevalent risk factors were the non / sporadic use of condoms (64%) and the consumption of alcoholic beverages (43%). The positivity of the population tested for syphilis (n = 150) was 9.3% and 9.1% of the participants correctly answered the forms of transmission of the infection.
Conclusion:
It was possible to identify the vulnerabilities to syphilis and adjust educational and care practices so that they result in significant learning and greater resilience for the population.
Key words: Syphilis; Health Vulnerability; Health Education; Counseling; Public Health Nursing
INTRODUCTION
Syphilis is an infection caused by Treponema palidum, which can attack the integumentary, lymphatic, cardiovascular, skeletal, and neurologic (neurosyphilis) systems, among others, according to its clinical evolution. The bacteria can also be transmitted through transplacental transmission from pregnant women who were not treated, or were poorly treated, to the fetus (congenital syphilis), which can lead to abortion, premature birth, malformations, and ophthalmic, auditive, and neurologic complications1.
The World Health Organisation (WHO) conveys that syphilis global prevalence is estimated at 0,5%, with regional numbers varying from 0,1 to 0,16%. Brazil has been undergoing a syphilis epidemic, in 2018, 158.051 cases of acquired syphilis, 62.599 cases of syphilis in pregnant women, 26.219 cases of congenital syphilis, and 241 deaths by congenital syphilis were notified through the Information System on Diseases of Compulsory Declaration (SINAN). The majority of the notified cases came from the Southeast region, Rio de Janeiro being one of the states with numbers above the national average2.
It is also believed that the cases are under-reported, considering that the individuals aren’t able to recognize the infection since no symptoms necessarily manifest themselves, or they could even disappear without treatment.
Given the importance and magnitude of syphilis in Brazil, it was projected, in 2016, an educational, itinerant activity named Syphilis Tent (Portuguese: Tenda da Sífilis), in which the regular nursing and medicine undergraduate students, and the students in the scientific initiation program, oriented by professors specialized in women’s health and by graduate students of an university in Rio de Janeiro, inform the target population regarding syphilis, its prevention, transmission, diagnosis, and treatment; distribute and teach how to use female and male condoms; showcase images which link the infection to the different life cycles; perform counseling pre and post Rapid Syphilis Test, and offer diagnostic testing.
Such action was projected to inform and counsel the population regarding syphilis, aiming to minimize its risks and vulnerabilities, and perform diagnostic testing and early treatments. The core of Syphilis Tent is that to treat it, it is necessary to correctly inform the population about the infection.
It is reinforced that the lack of knowledge is an important element of vulnerability to syphilis. Other personal factors are illiteracy, feeling of invulnerability, biological characteristics (immunosuppression history), subjective (values and beliefs), behavioral, and affective aspects, including use of drugs and alcohol, and unprotected sexual practices, which imply exposure and susceptibility to the disease3.
In this sense, schools, healthcare services, and universities have a fundamental role in the extensionist activities, performing joint actions to fulfill gaps and reduce vulnerabilities in the healthcare and prevention fields through dialogues and sharing of knowledge and support, favoring learning4.
Knowing the target audience whose educational acts are destined to is fundamental for actual learning to occur. The knowledge taught has to be related to knowledge that is already present in the life of the individual. When that knowledge starts making sense to the subjects, there is a higher possibility of changing behaviors and of diminishing vulnerability levels5.
In this context, this research’s objectives are: to describe and evaluate the socioeconomic profiles, the risk factors, the sexual practices, and the knowledge regarding the infection of all participants in the extensionist activity “Syphilis Tent”.
MATERIAL AND METHOD
This investigation is a cutout from the institutional research study “Syphilis in the life cycle: interfaces between health and education” (Portuguese: “Sífilis no ciclo da vida: interfaces entre a saúde e a educação”), conducted in the city of Rio de Janeiro. It is a descriptive, retrospective study, with a quantitative approach, finished in the period of time from october, 2016, until december, 2019, in the Nursing School in Rectorate Campus of the Federal University of the State of Rio de Janeiro (UNIRIO), and in the main hall of the Universitary Hospital Gafrée and Guinle (HUGG) building, pioneer in the field of treatments of Sexually Transmitted Infections (STI) since 1928, specially syphilis.
This study’s population was conveniently non probabilistic, composed of 1000 participants from the Syphilis Tent: students and professors of the healthcare field, users of healthcare services, outsourced employees, and public servants who, apriori, were invited to participate in this educational act, and oriented regarding the objectives of this research and their autonomous participation. Afterwards, they signed a Informed Consent Form, or, being the guardians, authorized underaged participants to take part in the research through it, and, thus, the collecting-data step began.
A newly created questionnaire with closed-ended questions was utilized as an instrument to collect data, and was organized with variables distributed in four different axes: sociodemographic profile, sexual practices, risk factors, and knowledge concerning syphilis. The collected data was stored, organized, and categorized into spreadsheets in the software Microsoft Office Excel Professional Plus 2016, and, subsequently, analyzed according to descriptive statistics, observing the absolute frequency and the percentage frequency, and presented throughout Tables.
To meet the demands established by Resolution n.º 466/2012, of the National Health Council - which manages the norms of researches involving human beings -, the present study was approved by the Ethics and Research Committee (CEP) of the Federal University of the State of Rio de Janeiro, with the Opinion n.º 2.213.742, n.º CAAE-70669517.9.0000.5285.
RESULTS
Socioeconomic profile
The participants of Syphilis Tent were characterized according to sex, age range, race/color (declared), educational level, individual income, and conjugal status. The majority of the investigated group is composed of women (72%), young adults in the age range from 18 to 44 years old (54,6%), white (40,9%), and single (50,9%). Most of them had individual income equal to or less than three minimum wages (R$937,00, its value at the time) (47,8%) and incomplete higher education (37%) (Table 1).
Table 1. Socioeconomic profile of the participants in Syphilis Tent. Rio de Janeiro-RJ, 2020.
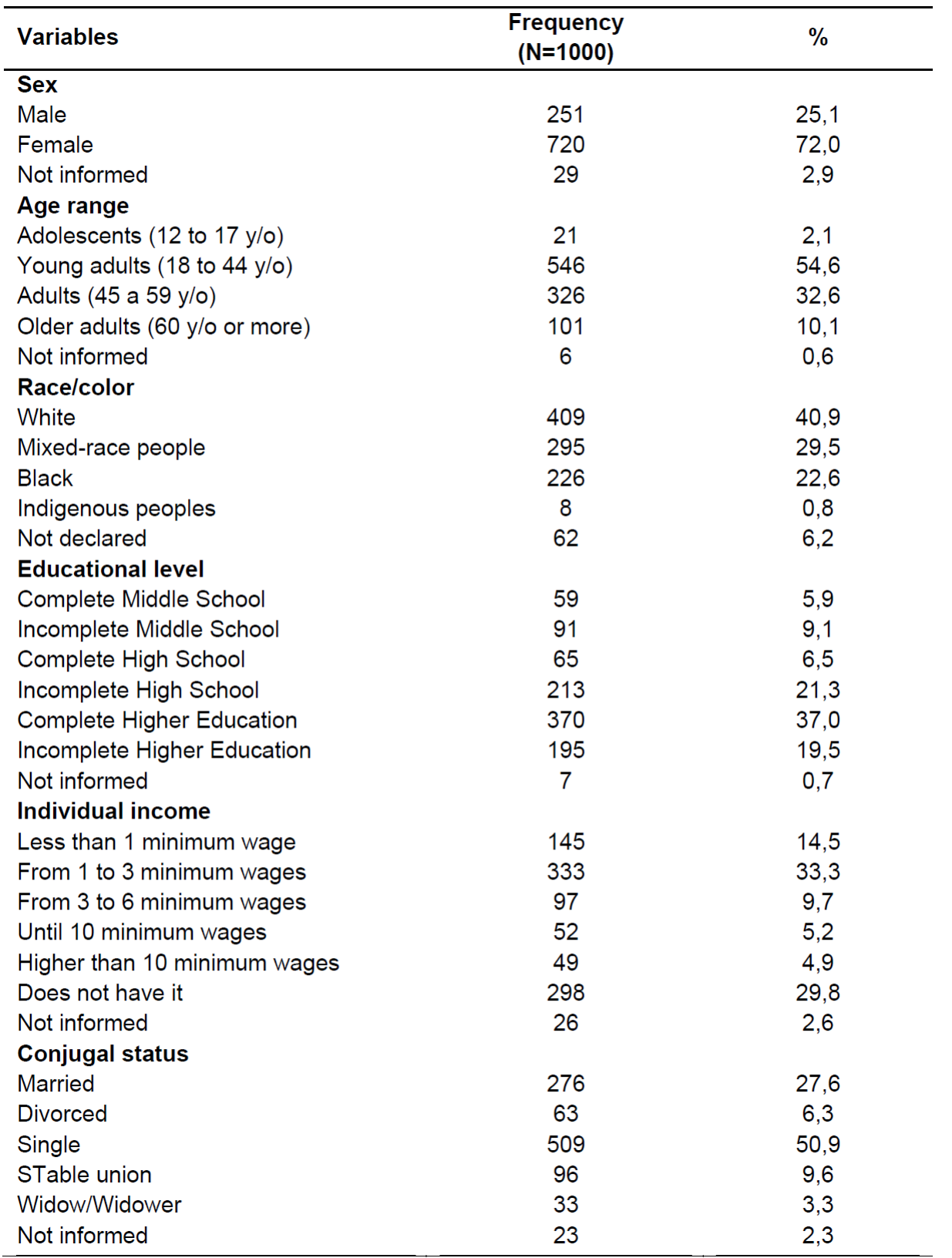
Source: Research data, Rio de Janeiro-RJ, 2020.
Risk factors, behaviours, and sexual practices
The majority of participants is heterosexual (86,2%), sexually active (75%), and with a single sexual partner (88%). Among the behaviours and sexual practices that can put them in risk of contact with syphilis, stands out: the non use/ sporadic use of condoms in sexual practices (64%) and the consumption of alcoholic beverages (42,7%). The use of illicit drugs was declared by 5,4% of the participants, and among the named drugs are marijuana, cocaine, methylenedioxymethamphetamine (ecstasy), and the combination of ether, chloroform, and ethyl chloride (“lança-perfume”).
It was ascertained that 10,4% of the interviewed people have previous history of some STI, the most mentioned by them being Human Papillomavirus infection (HPV) (20,2%), syphilis (19,2%), gonorrhea (17,3%), herpes (11,5%), among others.
It is reinforced that 53% of the participants had never done a laboratory examination to diagnose syphilis. Nonetheless, 46,2% got tested for syphilis during their life cycle; among those, 18,4% had been submitted to the Rapid Test, 31,4% to the nontreponemal test, Venereal Disease Research Laboratory (VDRL), and 31% to the treponemal test, Fluorescent treponema anti body absorption (FTA-abs). Table 2 presents the data regarding the risk factors related to syphilis, behaviours, and sexual practices of the participant population.
Table 2. Risk factors and sexual practices of participants in Syphilis Tent. Rio de Janeiro-RJ, 2020.

Source: Research data, Rio de Janeiro-RJ, 2020.
Knowledge concerning syphilis transmission
Only 9,1% of participants in Syphilis Tent answered correctly how the infection is transmitted.
The participants answered wrongly that are “not” ways of transmission: the contact with syphilitic injuries (45,5%); the transmission from the pregnant mother to her child, through the placenta (23,9%); sharing needles for the usage of drugs (49,1%), blood transfusion (39,7%); anal sex (22,2%); vaginal sex (8,9%); and oral sex (30,3%). They also answered that syphilis can be transmitted through: a handshake (3,8%); a kiss on the cheek (14,7%); breast milk (24,9%), and can be passed from the mother to her child as a hereditary disease (16,5%).
Testing for syphilis
150 Rapid Syphilis Tests were performed by licensed professionals during the activities of Syphilis Tent. The tested population’s (n=150) positivity rate was of 9,33%, it being 11 men and 3 women who were diagnosed positively.
All the participants who received the positive results also received post-test support and counseling, and were directioned to treatment, both individual and of their sexual partner(s), in HUGG’s Dermatology Ambulatory, and it proceeded with the fulfilling of the notification file in the vigent system.
DISCUSSION
Syphilis maintains itself as a stigma among the public health issues, affecting health and life of people all over the world, specially due to the lack of diagnosis and adequate treatments for syphilis cases, resulting in morbidity and mortality for children with congenital syphilis. An elaboration of public healthcare policies that vise improving the attention to health is necessary 2,6.
Brazil’s Ministry of Health has been adopting strategies to control syphilis in the country, such as: centralized buying and distributing of diagnosis and treatment inputs (Rapid Tests, benzathine, and crystalline penicillin); development of instruments which disseminate strategic information to managers; instrumentalization of situation rooms in all states; execution of the National Prevention Campaign; development of studies and researches regarding confronting syphilis in SUS (Sistema Único de Saúde)2.
Thus, an amplification of educational activities to control and prevent this disease has proved to be necessary. A study conducted in Basic Health Units (UBS, Unidade Básica de Saúde) in Paraná, between 2013 and 2015, showed there has been a reduction in the vertical transmission index, and in syphilis mortality rate, after an educational activity with the unit professional 7.
The majority of Syphilis Tent’s target audience were young adults, mostly women. In 2018, in Brazil, most of the acquired syphilis notifications occurred in individuals between 20 and 29 years old (35,1%), and women in this same age range reached 24,4% of the total of notified cases, meanwhile men represented only 16,1%2. Therefore, it is a population with higher vulnerability to syphilis and other STI.
That vulnerability is characterized in a dynamic of mutual interdependence which represent multidimensional values - biological, existential, and social. A situation of vulnerability limits the relational capacities of affirmation in the world, including the individual, social, and programmatic forms, resulting in fragilization 8. It is inferred that all individuals are vulnerable to syphilis, yet in distinct proportions, considering their social, economic, and cultural conditions. Women are perceived as more vulnerable to syphilis infection due to gender, cultural, and social issues (machismo) 9.
Regarding the sociodemographic factors which permeate syphilis in women, it is necessary to highlight illiteracy, low-income, conjugal status (sTable or transitory union); those factors are not limited to poverty situations 10,11. Other aspects include the age of first sexual activity, the number of sexual partners, the nonusage of condoms, and the use of psychoactive and illicit drugs 10.
In this perspective, it is necessary that in the healthcare services, specially in Primary Healthcare (ABS), is done an evaluation of women’s vulnerability to syphilis and STI, addressing five markers: the lack of openness to discuss aspects related to prevention in their relationship; the lack of perception of vulnerability; the disregard for vulnerability; the difficulty to recognize themselves as a subject with sexual and reproductive rights; and the actions of healthcare professionals, which limit women’s access to prevention12.
One of the facts that corroborate a higher notification of young women with syphilis is their use of healthcare services. Research shows that female users aged between 26 and 49 years old are the ones who seek medical assistance the most, the search for services being 1,9 times higher when compared to male users’. This is mostly due to the idea that a woman has more fragilities when compared to men, assuming we discuss healthcare with a relational perspective on gender. Nonetheless, it is necessary to comprehend that some factors hinder the masculine insertion into the healthcare unities, such as the institution’s service hours versus the man’s work schedule, the fact that they do not perceive themselves with the disease, and the idea, constructed by gender relations, of viewing men as a fortress, among other factors13.
As a result of the greater presence of women in the healthcare spaces, it was understood that could have been one of the factors that led to the female predominance in the activity proposed by Syphilis Tent. Nevertheless, the necessity of planning strategies to involve men in the educational actions and in the healthcare services, favoring the decrease of syphilis transmission, is known to be necessary.
It is interesting to highlight that many of those women are notified during pregnancy, when a prenatal care visit is taking place, since testing for syphilis is obligatory. Thus, studies show that cases of gestational syphilis occur more frequently in the age range between 20 and 39 years old, those being identified by the performance of tests recommended during prenatal appointments14,15,16.
Women in fertile ages, including adolescents and young adults, must be part of the target audience of educational activities regarding prevention of acquired syphilis and congenital syphilis, favoring the adoption of safe sexual practices, and, consequently, avoiding undesired pregnancy, the infection’s contagion, and transmission to the child. The educational practices destined to this group also need to include their sexual partners.
Research points out that women in reproductive age had higher representativity in positive Rapid Syphilis Tests, and reinforces that, in addition to identifying the risks of contamination and propagation of the disease, and of vertical transmission, it is necessary to sinalize the increasing maternal mortality risk 13.
A systematic reviewing study concerning the factors related to treponema pallidum’s transmission, and to the nursing assistance to pregnant women with syphilis, verified the existence of a variety of problems that affect not only the diagnosis, but also the treatment of gestational syphilis, among them: failures or absences during the performance of prenatal care, pregnant women’s limited knowledge regarding the disease, partners not seeking treatment, and the healthcare professionals’ limited knowledge regarding the disease17.
The group formed by young black women represented 13,8% of all the cases of acquired and gestational syphilis notified in Brazil in 20182. Therefore, when this young, black, and female population gets approached with the offered means, they could, through acquired knowledge, establish new standpoints concerning their own prevention.
Despite the fact that the majority of participants identified as white, the number of mixed-raced people combined to the number of black people exceeds the group that, according to the 2019’s epidemiological bulletin, includes the majority of people with acquired syphilis notification (47,1%), followed by 36,8% of mixed-race people, and 10,3% of black people2. That quantitative presents the infection’s universal nature, showcasing that all races and social classes are susceptible to syphilis.
Nonetheless, illiteracy and low economic and financial power are elements of social vulnerability to syphilis3. Considering this assertion, it could be affirmed that the biggest part of this study’s population is vulnerable to syphilis due to social issues, especially the low individual income of participants.
Evidences suggest that illiteracy, used as a socioeconomic variable, is associated to a higher prevalence of certain STI and to involvement in risky behaviour, for example, the low level of knowledge regarding preventive methods and the imprecise use of condoms, which showcases the link between those factors and syphilis occurrence 18.
Illiteracy interferes in the individual’s knowledge, in the perception of health problems, in the capacity to assimilate information, in the ways of acting and responding to health situations, and in the adherence to the treatment 19).
that Syphilis Tent is an itinerant activity, and that it happened in university campuses, the target audience was formed of professors, students in the health, humanitarian, and technological areas, public servants and outsourced employees, workers, healthcare services’ users, among others. The majority had complete or incomplete higher education, yet it could be noticed that, despite the educational level, the knowledge regarding syphilis transmission was rudimentary, highlighting gaps in knowledge and substantiating the relevance of educational practices in health.
It must be mentioned that the lack of knowledge concerning syphilis is not limited to the population lacking technical information. Study works conducted in academia shows that academics in the healthcare field have partial knowledge regarding syphilis, and that it is necessary to implement more effective educational strategies, since that knowledge is essential to fight this infection20.
That said, it is known that mere information does not guarantee preventive attitudes due to the existence of other individual, social, and institutional factors. It is also known that the interest in knowledge concerning the disease is more common after the infection than for its prevention, the internet being a popular way to search for information21.
The numbers regarding the infection’s transmission through anal and oral sex found in the research, which corroborated an international study, conducted with young adults with different nationalities that also considered that those sexual practices were not putting them into risk of contracting the STI22.
Many are the motives for the population to continue not knowing how the transmission occurs and how to prevent syphilis. The majority of people with the disease frequently is not aware of the infection, which can be transmitted not only through sex, but also through placental ways to the fetus during gestation, and which could lead to serious consequences 23.
This lack of knowledge arises from the incomprehension of possible clinical manifestations and from not knowing how to prevent and transmit the disease, and, concomitantly, subjective and cultural factors, which hinder early diagnosis and treatment. Thus, activities that focus on the creation of conditions for the individuals to be able to opine critically on those vulnerable contexts become significant 5.
Syphilis is strongly linked to the morality stigma, since it is a disease associated with sexual practices, and to avoid it, it implicates a transformation in life habits and in sexual behaviour. It is, noticeably, a social disease linked to health and biological states, which significantly impact the diagnosis and treatment of syphilis 9.
The relational patterns between the sexual partners interfere in the use of male condoms, especially when there are rigid patterns of masculine and feminine behaviour and disturbances in dialogue, with power relations stopping women from suggesting to the partner the use of male condoms, or from denying to have sexual intercourse without utilizing it. Those gender relations must be identified and considered when planning actions to prevent STI24.
In this study, it was highlighted as risky and vulnerable behaviour of the participants informed regarding syphilis and other STI: the sporadic use of or not using condoms during sexual relations. It is underlined that the majority of the participants had only one sexual partner, and was sexually active.
It is known that there is a higher difficulty in maintaining the use of condoms in the context of relationships considered sTable, which seems to contribute to unprotected sexual intercourse, and is linked to the perception of higher levels of affection and trust in the partner, relativizing preventive measures, and hindering the perception of their own condition of vulnerability to STI. There still exists the perception that condoms are infidelity and distrust symbols, and must be used only in relations with unknown partners10,25,26.
The male condom is an artifact used since primitive times, and with the advent of AIDS, it has become the main protection artifact against STI/HIV. Currently, male (external) and female (internal and usable during vaginal and anal intercourse) condoms are avaliable to the population. The consistent use of condoms continues to be the most effective barrier against the sexual transmission of HIV/STI. Male condoms have proved to be efficient, with around 80% to 90% of efficiency. Nonetheless, studies regarding female condoms are still not conclusive when it comes to its effectiveness percentage, though it can be affirmed that the use of both kinds of condoms amplified protection against STI 27.
It is necessary to recognize the affective-normative setbacks, which implicate in not adhering to the regular use of condoms for prevention, and, hence, elaborate more efficient strategies directed towards a specific population 26. Some barriers deserve the spotlight, for instance, precarious accessibility, religious and gender norms, stigma, and lack of will to use condoms28.
When the idea of not using condoms is discussed by sTable or sporadic partnerships, it is identifiable that, when there is stability, testimonies of not liking to use them and trusting the partner are given by men and women who have only one partner; when it comes to sporadic partnerships, the testimonies of not liking condoms and not having them are identifiable. In both situations, “not liking to use it” could be linked to the myth that claims there will certainly be a pleasure loss. The biggest barrier is the lack of acceptance to use of condoms, mostly manifested by men, resulting in its negotiation hindered 25.
The reasons to not utilize condoms during sexual relations are complex, as they part from the dramaticity of human life and its relationships, for example, from the decision regarding the type of sexual practice, from the gender relations, and from the avaliable resources. For prevention to occur, the user needs to acknowledge the necessity of using condoms according to their own knowledge. Those behaviours implicate in a bigger exposure to syphilis and its infection. Searching for strategies to change those behaviours is a huge challenge for healthcare teams.
Other risk factors which deserved to be highlighted in Syphilis Tent’s participants’ profiles were the consumption of alcoholic beverages and the use of illicit drugs, even if they were mentioned by the minority of users.
The use of drugs, licit or illicit, raises the vulnerability to STI, as the users’ capacity to discern risk is lower when in an euphoric state, resulting in risky sexual practices. Despite being considered an element of individual vulnerability, drug use is potentialized by the context of social vulnerability, socioeconomic conditions, and cultural patterns in which the population is inserted 3.
this perspective, it is fundamental that the educational activities aiming to prevent syphilis infection include themes related to elitism and drug addiction, highlighting the importance of safe sexual practices and of having their own materials to use, for example, syringes and needles, and not sharing them, as well as being routinely tested for syphilis and other STI.
Education can act to diminish vulnerability through activities that enable individuals to formulate critical opinion towards their own social conditions. When the subjects start to see reality as something liable to change, education starts having a fundamental importance to promote change and, consequently, a reduction in vulnerability levels5.
A study, which took place in a Ceará-CE county, regarding older adults’ knowledge about syphilis, has indicated that, after executing workshops with that population, there was a considerable increase in their knowledge. Still, it was reinforced that the individuals’ cultural characteristics must be taken into consideration when elaborating educational programs concerning prevention 29.
It must be stressed the importance of educational actions to be linked to Test and Counselling Centers (CTA) to increase the performance of Rapid Syphilis Tests, favouring the early diagnosis and helping to control the transmission. Thus, the target audience will have access to testing and to information regarding the infection.
It has been observed, in this study, that the majority of participants had never seeked laboratory examination to diagnose syphilis and, consequently, do not know their serologic status. It was ascertained that the VDRL was the most performed test, even though Rapid Tests are simple to execute, easy, and fast to read, besides having the equivalent performance of laboratory tests. The positivity rate of participants who got tested with Rapid Syphilis Tests during the educational action was of 9,33%.
The results of studies originated from a campaign of active search for syphilis cases in Belém have pointed the tested population’s positivity rate to be of 6,35%, representing a slightly raise when compared to the national prevalence, which varies between 1,5 to 5,0%, with elevated rates among groups with higher risk and vulnerabilities levels 13. In the present study, syphilis incidence was even higher.
The users, every so often, do not know their own serologic status due to the lack of accessibility to healthcare units and to the nonexistence of an adequate health network, remaining without a diagnosis. Thus, counseling and active search with domiciliary testing are recommended for a better coverage of the population 30.
Nevertheless, it must be considered that the majority of individuals who get tested for syphilis are referred for testing in case of suspicion, during prenatal investigations, and/or when the person identifies as an element in the key population25.
A lack of propagandas and campaigns encouraging testing for syphilis, as well as studies which identify the motives that lead the population to search for this service can be noticed. Taking a general look, it can be perceived, when acting on it, that first there is testing and identification of HIV, and syphilis starts to be investigated as an extra issue.
The results of the active search campaign regarding syphilis cases have shown effectiveness in diagnosis, strengthening the precepts of healthcare promotion and of prevention of harm that results in maternal and fetal mortality. It is highlighted that STI-tracking campaigns are important to protect lives, as they result in changes in individual and collective health conditions. Nonetheless, for the users’ adherence to occur, there must be strategic planning, with participation and commitment from professionals involved, in all different sectors 13.
Thus, the amplification of educational actions which inform the population regarding syphilis, and identify its risks and vulnerabilities, is recommended, as well as the performance of counseling and the provision of Rapid Tests and treatment for the positive cases.
CONCLUSIONS
Knowing the socioeconomic profile, evaluating behaviours and sexual practices, as well as the target audience of Syphilis Tent’s knowledge regarding syphilis, has permitted the identification of those individual’s vulnerability to syphilis, and that, thus, they need to be oriented concerning syphilis preventive, tramissive, and treatment methods, as well as feel they are essential pieces in the fight against syphilis, spreading acquired knowledge to their social circles.
The characterization of subjects in educational actions regarding STI also permits the professionals to examine their educative and assistance practices, and, consequently, there can be significant learning, proliferating resilience among the population.
REFERENCIAS
1. Workowski KA, Bolan GA. Sexually Transmitted Diseases Treatment Guidelines. MMWR Recomm Rep[internet] 2015 Jun [cited 2020 Jun 1]; 64(3):45-49. Available from: http://www.cdc.gov/mmwr/pdf/rr/rr6403.pdf [ Links ]
2. Brasil. Ministério de Saúde (MS). Boletim Epidemiológico de Sífilis 2018. Brasília: MS; 2019. [ Links ]
3. Ayres JR, Paiva V, Junior IF. Conceitos e práticas de prevenção: dahistória natural da doença ao quadro da vulnerabilidade e direitoshumanos. In: Paiva V, Ayres JR, Buchalla CM.Vulnerabilidade e direitoshumanos. Curitiba: Editora Juruá; 2012. 71-94p. [ Links ]
4. Santos NRZ, Silva PG, Garcia CAX, Bohrer R. Formação de Universitários Multiplicadores: Ações extensionistas no cenário escolar e comunitário no município de São Gabriel, RS. Rai. Rum. [internet] 2014 Jun [citado 2020 Jun 1]; 2 (2): 69-75. Disponível em: http://www.seer.unirio.br/index.php/raizeserumos/article/view/5561/5047 [ Links ]
5. Monteiro PHN, Donato AF. Contribuições teórico-práticas do campo da educação para as ações de prevenção em DST/AIDS. In: Paiva V, Ayres JR, Buchalla CM. Vulnerabilidade e direitoshumanos.Curitiba: Editora Juruá, 2012; 77-111. [ Links ]
6. Cardoso ARP, Araújo MAL, Cavalcante MS, Frota MA, Melo SP. Análise dos casos de sífilis gestacional e congênita nos anos de 2008 a 2010 em Fortaleza, Ceará, Brasil. Ciênc. saúde coletiva [Internet]. 2018 Fev [citado 2020 Jun 10]; 23(2): 563-574. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-81232018000200563&lng=en. [ Links ]
7. Lazarini FM, Barbosa DA. Educational intervention in Primary Care for the prevention of congenital syphilis. Rev. Latino-Am. Enfermagem[internet]. 2017 [cited 2020 Jun 10]; 25: e2845. Available from: http://www.scielo.br/pdf/rlae/v25/pt_0104-1169-rlae-25-02845.pdf. [ Links ]
8. Oviedo RAM, Czeresnia D. O conceito de vulnerabilidade e seu caráter biossocial. Interface (Botucatu) [Internet]. 2015 Jun [citado 2020 Jun 10]; 19(53):237-250. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S141432832015000200237&lng=en. [ Links ]
9. Costa NCCS. Análise da Representação Social do Processo Saúde-Doença da Sífilis Adquirida em mulheres em idade fértil [dissertação]. Manaus (AM): Universidade Federal do Amazonas; 2018. [ Links ]
10. Macêdo VC, Lira PIC, Frias PG, Romanguera LMD, Caires SFF, Ximenes RAA. Fatores de risco para sífilis em mulheres: estudo de caso-controle. RevSaude Publica [Internet]. 2017 [citado 2020 Jun 10]; 51: 78. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102017000100268&lng=en. [ Links ]
11. Dantas LA, Jerônimo SHNM, Teixeira GA, Lopes TRG, Cassiano NA, Carvalho JBL. Perfil epidemiológico de sífilis adquirida diagnosticada e notificada em hospital universitário materno infantil. Enferm. glob. [internet] 2017 abr [citado 2020 Jun 20]; 16 (46): 227-235. Disponível em: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S169561412017000200217&lng=es&nrm=iso&tlng=pt [ Links ]
12. Guanilo MCTU, Takahashi RF, Bertolozzi MR. Avaliação da vulnerabilidade de mulheres às Doenças Sexualmente Transmissíveis - DST e ao HIV: construção e validação de marcadores. Rev. esc. enferm. USP [Internet]. Ago 2014 [citado 2020 Jun 20]; 48 (spe): 152-159, . Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S008062342014000700152&lng=en&nrm=isso [ Links ]
13. Silva EC, Tupinambá MR,Silva FASD, Vieira JR, Borges SCR, Nascimento LS. Resultados de sorologia para casos de sífilis em campanha de município no norte do Brasil. RevPan-AmazSaude [Internet]. 2016 Mar [citado 2020 Jun 20]; 7(1): 39-43. Disponível em: http://scielo.iec.gov.br/scielo.php?script=sci_arttext&pid=S2176-62232016000100005&lng=pt. [ Links ]
14. Cavalcante PAM, Pereira RBL, Castro JGD. Sífilis gestacional e congênita em Palmas, Tocantins, 2007-2014. Epidemiol. Serv. Saúde [Internet]. Jun2017 [citado 2020 Jun 20]; 26(2): 255-264. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S2237-96222017000200255&lng=en. [ Links ]
15. Marques JVS, Alves BM, Marques MVS, Arcanjo FPN, Parente CC, Vasconcelos RL. Perfil epidemiológico da sífilis gestacional, clínica e evolução de 2012 a 2017. SANARE, Sobral[Internet]. jul-dez 2018 [citado 2020 Jun 20]; 17(2):13-20. Disponível em: https://sanare.emnuvens.com.br/sanare/article/view/1257 [ Links ]
16. Favero MLDC, Ribas KAW, Costa MCD, Bonafe SM. Sífilis congênita e gestacional: notificação e assistência pré-natal. Arch Health Sci [Internet]. 2019 [citado 2020 Jun 20]; 26(1):2-8. Disponível em: http://www.cienciasdasaude.famerp.br/index.php/racs/article/view/1137/776 [ Links ]
17. Leite IA, Oliveira JM, Leão MCM, Lopes SF, França AMB. Assistência de enfermagem na sífilis na gravidez: uma revisão integrativa. Ciências Biológicas e da Saúde [Internet]. Nov 2016 [citado 2020 Jun 20]; 3(3): 165-176. Disponível em: https://periodicos.set.edu.br/index.php/fitsbiosaude/article/view/3417/2019 [ Links ]
18. Barros CVL, Galdino JH, Rezza G, Guimarães RA, Ferreira PM, Souza CM, et al. Bio-behavioral survey of syphilis in homeless men in Central Brazil: a cross-sectional study. Cad. Saúde Pública [Internet]. 2018 [cited 2020 Jun 20]; 34(6): e00033317. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2018000605009&lng=en. [ Links ]
19. Siqueira MA, Rolim MAD, Ferreira Junior AR, Rocha FAA, Cavalcante MMB. Sentimentos e conhecimentos de puérperas em face da Sífilis congênita neonatal. Rev. Bras. Pesq. Saúde, jul-set 2017; 19(3): 56-61. [ Links ]
20. Pereira RMS, Valerio FM, Barros KM, Reis TS, Trajano LT, Silva LR. Conhecimento de acadêmicos da área de saúde sobre sífilis. Revista Práxis [internet].Dez 2018 [citado 2020 Jun 20]; 10(20): 119-127. Disponível em: http://revistas.unifoa.edu.br/index.php/praxis/article/view/1516/2317 [ Links ]
21. Navega DA, Maia ACB. Conhecer (e) saber: relatos de pessoas curadas da sífilis. RevBrasPromç Saúde [internet],Abr 2018 [citado 2020 Jun30];31(2):1-9. Disponível em: https://periodicos.unifor.br/RBPS/article/view/6943/pdf [ Links ]
22. Gravata A, Castro R, Borges-costa J. Study of the Sociodemographic Factors and RiskyBehaviours Associated with the Acquisition of Sexual Transmitted Infections by Foreign xchange Students in Portugal. Acta MedPort[internet],Jun, 2016 [citado 2020 Jun 30]; 29(6):360-366. Disponível em: http://dx.doi.org/10.20344/amp.6692. [ Links ]
23. Padovani C, Oliveira RR, Pelloso SM. Syphilis in during pregnancy: association of maternal and perinatal characteristics in a region of southern Brazil. Rev. Latino-Am. Enfermagem [Internet]. 2018 [cited 2020 Jun 30]; 26: e3019. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692018000100335&lng=en. [ Links ]
24. Figueiredo R, Santos NJS. Redução de exposição a infecções por DST/HIV/AIDS em práticas sexuais. In: Paiva V, Ayres JR, Buchalla CM. Vulnerabilidade e direitoshumanos. Curitiba: Editora Juruá; 2012, 328p. [ Links ]
25. Ferreira CO, Viana ASA, Silva AA, Rezende REA, Gomes AVTM, Davoglio RS. Perfil epidemiológico dos usuários de um centro de testagem e aconselhamento da Bahia. Rev. Baiana de Saúde Pública [internet]. abr/jun 2016[citado 2020 Jun 30]; 40(2): 388-409. Disponível em: https://doi.org/10.22278/2318-2660.2016.v40.n2.a1980. [ Links ]
26. Dourado I, Maccarthy S, Reddy M, Calazans G, Gruskin S. Revisitando o uso do preservativo no Brasil. Rev. Bras.Epidemiol [Internet]. set 2015 [citado 2020 Jun 30]; 18 (suppl 1): 63-88. Disponível em: https://www.scielo.br/pdf/rbepid/v18s1/pt_1415-790X-rbepid-18-s1-00063.pdf [ Links ]
27. WiyehAB, Mome RKB, Mahasha PW, Konqnyuy EJ, Wiysonge CS. Effectiveness of the female condom in preventing HIV and sexually transmitted infections: a systematic review and meta-analysis. BMC Public Health [internet]. 2020 [cited 2020 Jun 30]; 20(319): 17p.Available from: https://doi.org/10.1186/s12889-020-8384-7 [ Links ]
28. Beksisnka M, Wong R, Smit J. Male and female condoms: Their key role in pregnancy and STI/HIV prevention. Best Res Clin ObstetGynaecol [internet]. 2019 [cited 2020 Jun 30]; 1-13. Available from:https://doi.org/10.1016/j.bpobgyn.2019.12.001 [ Links ]
29. Bastos LM, Tolentino JMS, Frota MAO, Tomaz WC, Fialho MLS, Batista ACB, et al. Avaliação do nível de conhecimento em relação à Aids e sífilispor idosos do interior cearense, Brasil. Ciênc. saúde coletiva [Internet]. Ago2018 [citado 2020 Jun 30]; 23(8): 2495-2502. Disponível em: https://doi.org/10.1590/1413-81232018238.10072016. [ Links ]
30. Ribeiro LV, Sabidó M, Galbán E, Guerra JA, Mabey D, Peeling RW, Benzaken AS. Home-based counseling and testing for HIV and syphilis - an evaluation of acceptability and quality control, in remote Amazonas State, Brazil. Sex Transm Infect 2015; 91(2): 94-96. [ Links ]
Received: October 02, 2020; Accepted: January 13, 2021











 text in
text in 


