My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.21 n.66 Murcia Apr. 2022 Epub May 02, 2022
https://dx.doi.org/10.6018/eglobal.487441
Originals
Assessment of the quality of natural childbirth care in hospital setting through the Bologna index
1 Universidad Federal de Paraíba . João Pessoa, Paraíba, Brasil. maria_clara_paiva@hotmail.com
2 Universidad de Pernambuco , Programa de Posgraduación en Obstetricia de la Facultad Santíssima Trindade, Recife, Pernambuco, Brasil
3 Universidad Federal de Pernambuco , Centro Académico de Vitória, Vitória de Santo Antão, Pernambuco, Brasil.
Objective:
To assess the quality of care during natural childbirth in hospital setting through the Bologna Index.
Method
This is an observational and cross-sectional study, with a quantitative design, performed in a reference service in obstetric care, located in the Northeast region/Brazil. A form based on the quality indicators of the Bologna Index and guidelines for natural childbirth and puerperal care was used. Data were analyzed through descriptive and inferential statistics. When analyzing the Bologna Index, 1 point was assigned to each variable met; and, after assessing each item, care was classified based on the following sum: “0” for lower quality, “1 to 4” for intermediate quality and “5” for higher quality of care.
Results:
It was found an average of 3.44 in the Bologna Index, corresponding to intermediate quality care. Among the five variables that make up the Bologna Index, the highest percentages were related to the use of partograph (85.4%), presence of a caregiver at the time of childbirth (94.5%) and skin-to-skin contact between mother and child in the first hour of life (98.1%). Nevertheless, there was a reduced percentage regarding the use of non-supine positions (9.1%) and absence of stimuli in the first clinical period of childbirth (56.3%).
Conclusion:
there has been progress in the quality of childbirth care in hospital setting, but it is necessary to provide information for the empowerment of women, greater adherence of professionals to good obstetric practices and insertion of nurses in the usual-risk obstetric care.
Keywords: Health assessment; Nursing; Health quality indicators; Assessment methods; Humanized birth
INTRODUCTION
In Brazil, humanization practices in natural childbirth are focused on improving access to care through the use of protocols and follow-up of quality indicators 1. In addition, childbirth care brings up new skills and practices in the hospital environment, with the objective of reducing risks, in such a way as to reorganize the existing obstetric model of medicalization 2.
The humanization of childbirth brought up to the field of obstetrics the discussion about the empowerment and autonomy of women, making them protagonists with a view to reducing the medicalization of the female body during labor and childbirth. In this perspective, good obstetric and neonatal care practices are included as a guarantee of the benefits provided, emphasizing female participation, as they are aware of their possibilities throughout the childbirth process 3.
From a physiological point of view, pregnancy and childbirth are expected to proceed without complications for the mother and her conceptus. Nonetheless, there may be some complications resulting from pre-existing maternal pathologies, inadequate modifications and adaptations of the gravid organism, which can threaten the binomial. In addition, the moment of giving birth has a remarkable meaning in the lives of women and their families, since it is a natural event that needs respect due to the changes that occur, both in the female body and in the female psychological 4.
In Brazil, the prevalence of good obstetric practices is still low, which contributes to the increase in maternal and perinatal risks 5. In 2011, the Ministry of Health (MS, as per its Portuguese acronym) launched the Stork Network program, in order to consolidate the model of humanized care in the labor and childbirth process, as well as to encourage the improvement of the quality of care during the pregnancy-puerperal cycle. This program encompasses a care network that ensures women the right to reproductive planning and humanized action in relation to pregnancy, childbirth and puerperium, besides ensuring children the right to a safe birth 6,3.
For some women, especially high-risk pregnant women, hospital centers that have maternity hospitals are considered safe places to give birth because they include technologies and multidisciplinary care 7. In fact, advances in the field of obstetrics have contributed to the improvement of indicators of maternal and perinatal morbidity and mortality; however, it has exposed women and their conceptuses to high rates of interventions, such as episiotomy, cesarean sections without indications, routine oxytocics, among others, which, most of the time, generate negative experiences or unfavorable maternal and/or neonatal outcomes, which is why it is essential to assess the obstetric care process to ensure safe and humanized care 3.
Similarly, assessing the quality of care is essential for any health care program, as it favors the improvement of the process, identifying possible successes and errors. Although there are no standardized indicators to assess the quality of maternal and neonatal care, some are suggested by international bodies, such as the World Health Organization (WHO), which help in the process of improving the quality of safe labor and childbirth, as well as healthy growth and development of infants 8.
In this context, the Bologna Index is an instrument to assess the quality of childbirth care, addressing it as a physiological event. This index has the purpose of indicating the quality in the conduct of natural childbirth in obstetric institutions, highlighting the presence of a caregiver, use of partograph, absence of labor stimulation, such as the use of oxytocin, forceps, Kristeller maneuver, among other variables 9,8.
The study on the assessment of good practices in the process of caring for natural childbirth in hospital setting is supported by the need to identify inadequacies and discuss about quality and safe care. Accordingly, it is worth emphasizing the importance of using quality indicators, in particular the Bologna Index, in the assessment of care offered throughout the parturition process, as a diagnosis of care provided and incentive to reflect about the current obstetric practice, aiming at improvement and adoption of good obstetric and neonatal care practices. It is highlighted that the Bologna Index is an instrument used both nationally and internationally, as suggested by the World Health Organization (WHO) 8.
Based on the above, this study had the objective of assessing the quality of care during natural childbirth in hospital setting through the Bologna Index.
METHOD
This is an observational and cross-sectional study, with a quantitative design, which was performed in a reference service in obstetric care, located in the capital of Paraíba, Northeast region/Brazil.
The sample was obtained by convenience and consisted of all eligible patients during the data collection period, which took place between November 2019 and March 2020, totaling a sample of 55 puerperal women.
To that end, women of any age group, with usual-risk pregnancy, whose vaginal delivery, spontaneous or induced, took place in the maternity hospital, between 37 and 42 weeks of pregnancy, with a single fetus and who, in the postpartum period, were included in the rooming-in unit within 48 hours.
The sample excluded puerperal women who had stillbirths or neonatal deaths; women who had some previously diagnosed cognitive and mental limitation that made comprehension and verbal expression difficult, making their participation impossible; and puerperal teenagers without legal guardians at the time of the interview.
Data were collected through face-to-face interviews with puerperal women during their stay in the rooming-in unit of the maternity hospital and additional information contained in the medical records of these women and their newborns.
To that end, a form containing questions about the woman’s sociodemographic characteristics, her obstetric history and data on labor, childbirth and postpartum was designed. The form was based on indicators contained in the guide ‘Natural childbirth care: a practical guide’; Guidelines of the Stork Network (RC, as per its Portuguese acronym) program; National guidelines on natural childbirth care; ‘Recommendations for a positive childbirth experience’; and on the Bologna Index 10)(6)(11)(12.
Subsequently, the data collection form was assessed by three specialists in the area of women’s health for the adequacy of the items. Next, a pilot test was carried out with five puerperal women, in order to check the acceptability, clarity and understanding of the instrument’s language. It was found that further adjustments were necessary, and the statistical sample was discarded. A second pilot test proved the quality and acceptability of the collection form.
The Bologna Index variables used were the presence of a caregiver during childbirth; use of partograph; absence of labor stimulation (use of oxytocin, forceps, Kristeller maneuver); delivery in the non-supine position; and skin-to-skin contact between mother and child for at least 30 minutes in the first hour 8.
Data were tabulated in Excel and analyzed using the Statistical Package for the Social Sciences (SPSS), version 26.0. Descriptive statistics (measures of central tendency, absolute and relative frequencies) and inferential statistics (Pearson’s Chi-square test or Fisher’s Exact test) were used. Fisher’s Exact test was used in cases where the number of cells with a frequency lower than 5 was greater than 20%.
The Chi-Square Proportion Test was also performed to assess the distribution of variables, in order to identify differences between observed and expected frequencies in that population. For all analyses, a significance level of 5% was used (p-value<0.05).
In order to perform the analysis of the Bologna Index, one point was assigned to each variable, if it was met. After assessing the care, the sum value “0” is considered as lower quality, from “1 to 4” as intermediate quality and “5” as higher quality care.
This study was approved by the Research Ethics Committee of the Health Sciences Center (CCS) of the Federal University of Pernambuco (UFPE), with Opinion nº 3.958.607/2020 and Certificate of Presentation for Ethical Consideration nº 94050318.6.0000.5208.
RESULTS
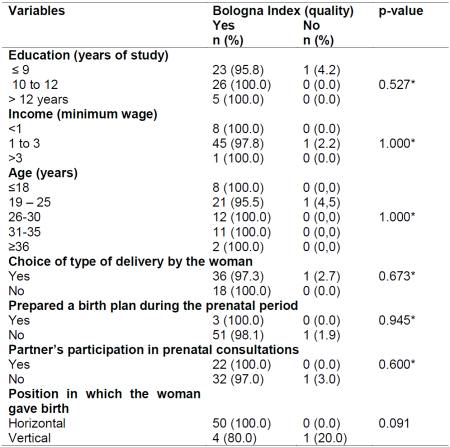
Concerning the sociodemographic characteristics, it was found an average age of 25 years (SD ± 6.56), most women lived with a partner (36; 65.5%), self-declared brown (37; 37.3%), had a paid activity (28; 50.9%), had a monthly income of 1 to 3 minimum wages (46; 83.6%) and had completed high school (26; 47%), as displayed in Table 1.
Table 1. Sociodemographic distribution of puerperal women (n=55). João Pessoa, PB, Brazil, 2021.
*Minimum wage at the time of data collection: R$1,045.00 -
**Chi-Square Proportion Test.
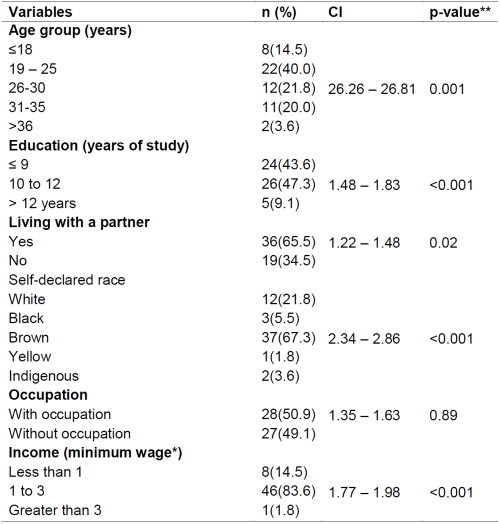
As for the obstetric data, it was noted an average gestational age of 39 weeks (SD ± 1.56) and 1.93 cm of dilation (SD ± 0.89) at the time of admission to the maternity hospital. Most women were admitted for natural childbirth with less than 6 cm of cervical dilation (63.6%). Among the study participants, only three prepared and delivered the birth plan (5.5%). It was noted an incentive to breastfeeding in the delivery room (42; 76.4%). Low-risk obstetric deliveries were assisted by physicians (33; 60%) and by nurses (22; 40%). The obstetric profile of puerperal women and data on newborns are described in Table 2.
Table 2. Obstetric profile of puerperal women and data on newborns (n=55). João Pessoa, PB, Brazil, 2021.
*Chi-Square Proportion Test.
Among the interviewees, 26 were primiparous and 47 had spontaneous deliveries. The average number of visits to the maternity hospital in search of admission was 2.71 (SD ± 0.10) and the average number of vaginal touches performed between the time of admission and the childbirth was 2.60 (SD ± 0.09), performed mostly by the medical professional (46; 83.6%). In most births, newborns had an Apgar score greater than 7 in the first minute of life (49; 89%).
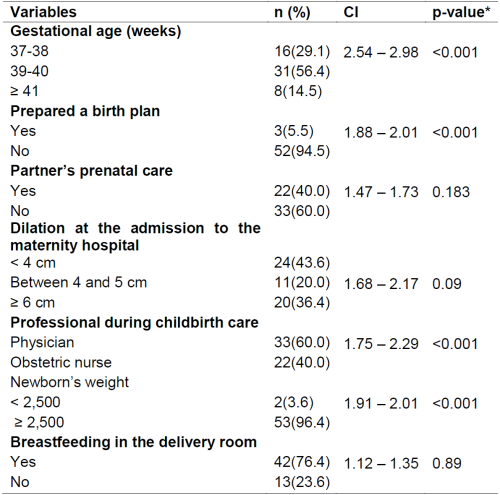
As for the assessment of obstetric care by the Bologna Index, it was noted an overall average of 3.44, classifying the service with intermediate quality. Among the five variables that make up the Bologna Index, the highest percentages were related to the use of partograph (85.4%), presence of a caregiver at the time of childbirth (94.5%) and skin-to-skin contact between mother and child, at least 30 minutes, in the first hour of life (98.1%). Regarding the non-recommended obstetric care practices, it was found the use of oxytocin (27.2%) during the first stage of labor and performance of the Kristeller maneuver (9%) at the time of birth (Table 3).
Table 3. Bologna Index variables in the labor and childbirth care service (n=55). João Pessoa, PB, Brazil, 2021.
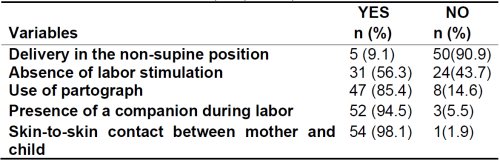
Among the types of positions for natural childbirth, the most frequent was the lithotomy position (50; 90.9%). Nonetheless, it was found an influence of the horizontal position on the intermediate quality obtained from the Bologna Index, as displayed in Table 4.
DISCUSSION
The assessment of the care provided during labor and childbirth in hospital setting based on quality indicators is essential for the improvement of obstetric care and greater satisfaction with the experience of natural childbirth. According to this proposal, the assessment of care quality becomes continuous and not based only on the consequences of any error in the process 1,13.
It is worth underlining that the Bologna Index encompasses variables that aggregate aspects associated with care procedures during childbirth, being a quantitative, accessible and easy-to-apply indicator, which has the objective of assessing the quality of care during natural childbirth 8.
In Brazil, intermediate quality obstetric care, obtained by the Bologna Index, was also found in the states of Rio Grande do Norte and Pernambuco 9,8. Thus, there was a sociodemographic profile similar to other Brazilian surveys conducted with puerperal women in public maternity hospitals 14,15.
On the other hand, a survey conducted in Porto Alegre pointed out that the quality of hospital care during childbirth is not satisfactory when compared to other countries in the world that had lower rates of neonatal mortality and greater adherence to good obstetric practices. This statement may be associated with the maintenance of inadequate and harmful practices held in the hospital obstetric environment in Brazil14.
It is noticed that this fact directly impacts the care provided and reinforces the female passivity at the expense of the hegemony of the protagonism of health professionals throughout the physiological process, since there are few women who prepare birth plans and, possibly, dialogue with the team about the execution of interventions during the parturition period 8.
It is underlined that the need for guidance and greater encouragement of good obstetric practices in such a way as to address respect for the physiology of childbirth. In addition to stimulating vertical positions, when encouraging the woman in the face of several possibilities and free choice of position, not using the Kristeller maneuver, greater awareness of the importance and benefits of using partograph, respect for the presence of a caregiver during childbirth as well as encouragement for the golden hour, in order to strengthen the bond and the benefits for maternal and neonatal health8)(13)(15.
The use of non-supine positions is associated with pain control and reduction and makes uterine contractions more efficient. It is underlined that this practice belongs to category A of the WHO classification 8. Nonetheless, there was a considerable frequency of women who gave birth in the horizontal position and, consequently, there was a contribution to the reduction of points in the Bologna Index.
In Porto Alegre, it was found that vertical positions in the expulsive period were predominant in births assisted by obstetric nurses as a strategy that helps to reduce the duration of the second stage of labor, risk of cesarean section, need for epidural analgesia, among other advantages. Accordingly, it is underlined that women should be informed about the benefits related to the vertical position and encouraged to assume the one that best suits their needs, in order to favor the natural course of childbirth 16.
In the results, it was noted a relevant percentage regarding the non-use of labor-stimulating drugs. Nevertheless, it was still found the use of oxytocin during the first clinical period, as well as the performance of the Kristeller maneuver, procedures that are contrary to the physiology of natural childbirth.
In Brazil, the use of synthetic oxytocin is associated with the growth of hospitalization in cases of natural childbirth, the Figure of the obstetrician as the main responsible for the parturition process, the high medicalization of the female body and other obstetric interventions, such as episiotomy, use of the horizontal position and the Kristeller maneuver, a procedure that is currently forbidden 17. A cross-sectional study conducted in Sweden showed a percentage of 46% in the use of synthetic oxytocin in the first stage of childbirth, relating it to negative experiences faced by women during childbirth 18.
Synthetic oxytocin is routinely used in several Brazilian maternity hospitals with the purpose of increasing and accelerating contractions, which directly interferes with natural childbirth 19. In turn, Kristeller maneuver, in addition to being known to be harmful to maternal and neonatal health, is also ineffective during childbirth, which should proceed with the least possible interventions, as recommended by scientific evidence 20.
In addition, there is the WHO recommendation to avoid early admission with cervical dilatation less than 4 centimeters because it leads to unnecessary interventions, associated with an increase in the length of stay of the parturient woman in the hospital environment 12.
As for the use of partograph, it is recognized that this tool contributes to the accurate follow-up of labor, deviations in relation to maternal and fetal well-being and the evolution of childbirth 21. These records help the team to carry out interventions that are essential to the clinical needs of mothers and fetuses, in order to reduce the risk of maternal-fetal mortality 22. A descriptive exploratory cross-sectional study conducted in Acre showed the use of partograph in 53.5% of the analyzed medical records 23.
From this perspective, it is essential to raise awareness of the team for the adequate and continuous completion of the partograph, as well as its full understanding. To that end, it is essential that each professional, responsible for obstetric care, recognize the importance of this instrument, in such a way as to prioritize its use, even in an unfavorable setting, since inadequate records or the non-use of this instrument can favor the increase of number of cesarean sections 24.
In the current research, it was noticed an expressive respect for the presence of a caregiver during childbirth, which is directly associated with the guarantee of the law and a respectful, welcoming and qualified care. Accordingly, the sensitive experience of childbirth refers to a type of desired family communion, since the company of someone who shares the emotion of giving birth is a link with the family and intimate context experienced before the hospital, which helps to situate the childbirth as a life story 25.
The presence of a caregiver, according to the woman’s preference, during labor, childbirth and immediate postpartum, was regulated in Brazil by Law nº 11.108, dated April 7, 2005 26. This measure was reaffirmed through Ordinance GM/MS nº 1.459, dated June 24, 2011, which institutes the Stork Network program, with the objective of guaranteeing safety and welcoming during labor and childbirth for women and their newborns, through the presence of a caregiver 6.
In the variation of the Bologna Index, the immediate and continuous skin-to-skin contact between mother and child in the first hour after delivery is also assessed, and this has the purpose of improving the adaptation period of the newborn and the mother in the transition from the intrauterine to the extrauterine space and to provide a greater bond between the binomial. In a retrospective and documentary study, with a quantitative approach, conducted in a maternity hospital in the state of Alagoas, it was noted a percentage of 79.17% in relation to compliance with the variable “immediate skin-to-skin contact”, which shows adherence to this humanization practice in cases of natural childbirth 21. In addition, a descriptive study, with a qualitative approach, developed in the state of Pernambuco, expressed that nurses showed adequate scientific knowledge about this practice, as well as about other humanization actions carried out in the delivery room 27.
During usual-risk natural childbirth care, the role of the obstetric nurse can ensure the woman a feeling of support, sense of tranquility and confidence in the birth setting. This relationship of mutual trust between the nurse and the parturient woman favors her well-being and creates a bond based on interaction and listening skills, in order to make these relationships more horizontal and therapeutic 15.
A descriptive and exploratory study, with a qualitative approach, conducted in Salvador revealed that the women interviewed reported satisfaction with nursing care, associating it with attention in the care received, in the treatment according to individual and subjective needs, in staying by the side and in receiving words of encouragement during the natural childbirth process 28.
It is important to infer that the care model proposed by the Stork Network program suggests the guarantee of good practices and safety in labor and childbirth care, including the participation of obstetric nursing in usual-risk childbirth care, encouraging its protagonism in care and autonomy to act as a team 29. Nevertheless, in Brazilian maternity hospitals, there is still a strong influence of the medical professional as responsible for the usual-risk parturition process 30.
Finally, it is noted that, when present in the pregnancy-puerperal process, the humanized care plan favors the exchange of information between health professionals and women, as a means of ensuring knowledge about legal rights, as well as empowerment about the physiology of natural childbirth. In addition, this knowledge favors women’s autonomy in terms of childbirth, making them the protagonists during pregnancy, childbirth and puerperium 7.
CONCLUSION
Natural childbirth care in hospital setting was classified as intermediate quality by the Bologna Index, with relevant expression regarding skin-to-skin contact between mother and child, presence of a caregiver during childbirth and the use of partograph. In light of the results observed in the current study, it is noticed that there has been progress in the quality of care in childbirths in hospital setting, but it is necessary to expand the information for women, which corroborates the autonomy and safe choices based on the encouragement of the birth plan, in addition to greater adherence of professionals to good obstetric practices and insertion of nurses in usual-risk obstetric care.
The data from this research have the potential to contribute to the improvement of labor and childbirth care and to the discussion of variables that stimulate the quality of obstetric care, in order to awaken continuity in the adherence to good practices in public health services.
With regard to the limitations of this study, it is highlighted the fact that the interviews were performed within 48 hours postpartum, during the hospitalization of puerperal women. This condition can generate a courtesy bias for data collection and, consequently, influence responses about childbirth care practices. In addition, another limitation refers to the fact that the Bologna Index does not include qualitative variables that can be essential to obtain a broader perception of the quality of obstetric care.
REFERENCIAS
1. Genovesi FF, Canario MASS, Godoy CB, Maciel SM, Cardelli AAM, Ferrari RAP.Maternal and child health care: adequacy index in public health services. Rev Bras Enferm [Internet]. 2020 [acesso 2021 Mar 25]; 73(Suppl 4). Disponível em: https://doi.org/10.1590/0034-7167-2017-0757 [ Links ]
2. Bourguignon AM, Grisotti M. A humanização do parto e nascimento no Brasil nas trajetórias de suas pesquisadoras. Hist Cienc Saude Manguinhos [Internet]. 2020 [acesso 2021 Mar 25]; 27(2):485-502. Disponível em: https://doi.org/10.1590/S0104-59702020000200010 [ Links ]
3. Leal MC, Bittencourt SA, Esteves-Pereira AP, Ayres BVS, Silva LBRAA, Thomaz EBAF, et al. Progress in childbirth care in Brazil: preliminary results of two evaluation studies. Cad Saúde Pública [Internet]. 2019 [acesso 2021 Mar 26];35(7):e00223018. Disponível em: https://doi.org/10.1590/0102-311X00223018 [ Links ]
4. Carvalho SS, Silva CS. Revisão integrativa: promoção das boas práticas na atenção ao parto normal. Rev Aten Saúde [Internet]. 2020 [acesso 2021 Mar 27];18(63):110-9. Disponível em: https://dx.doi.org//10.13037/ras.vol18n63.6290 [ Links ]
5. Vieira BC, Backes MTS, Costa LD, Fernandes VMB, Dias HHZR, Backes DS.Applying best practices to pregnant women in the obstetric center. Rev Bras Enferm[Internet]. 2019 [acesso 2021 Mar 27];72:191-6. Disponível em: https://doi.org/10.1590/0034-7167-2018-0422 [ Links ]
6. Ministério da Saúde (BR). Portaria nº 1.459, de 24 de junho de 2011. Institui a Rede Cegonha. Diário Oficial da União, Brasília (DF), 2011 [acesso 2021 Mar 29]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1459_24_06_2011.html [ Links ]
7. Leal MS, Moreira RCR, Barros KCC, Servo MLS, Bispo TCF. Humanization practices in the parturitive course from the perspective of puerperae and nurse-midwives. Rev Bras Enferm [Internet]. 2021 [acesso 2021 Mai 9];74(Suppl 4):e20190743. Disponível em: https://doi.org/10.1590/0034-7167-2019-0743 [ Links ]
8. Moura NAS, Holanda VR, Albuquerque GPM, Castro JFL, Silva HRL, Rocha EPG.Analysis of practices in childbirth and postpartum hospital care. Rev Rene [Internet]. 2020 [acesso 2021 Mar 30];21:e43671. Disponívelem: https://doi.org/10.15253/2175-6783.20202143671 [ Links ]
9. Carvalho IS, Brito RS. Using the Bologna Score to assess normal delivery healthcare. Rev Esc Enferm USP [Internet]. 2016 [acesso 2021 Mar 30];50(5):741-8. Disponível em: http://dx.doi.org/10.1590/S0080-623420160000600005 [ Links ]
10. Organização Mundial de Saúde. Assistência ao parto normal: um guia prático [Internet]. Saúde materna e neonatal. Unidade de maternidade segura. Saúde reprodutiva e da família. Genebra: OMS, 1996 [cited 2021 Abr 2]. Disponível em: https://www.yumpu.com/pt/document/view/42116270/maternidade-segura-aben [ Links ]
11. Ministério da Saúde (BR). Diretrizes nacionais de assistência ao parto normal: versão resumida. Brasília: Ministério da Saúde; 2017 [acesso 2021 Abr 2]. Disponível em:http://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_nacionais_assistencia_parto_normal.pdf [ Links ]
12. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018 [acesso 2021 Abr 9]. Disponívelem: https://www.who.int/publications/i/item/9789241550215 [ Links ]
13. Vilela MEA, Leal MC, Thomaz EBAF, Gomes MASM, Bittencourt SDA, Gama SGN, et al. Assessment of delivery and childbirth care in the maternity units of RedeCegonha: the methodological paths. CiêncSaúde Colet [Internet]. 2021 [acesso 2021 Abr 16];26(3):789-800. Disponívelem: https://doi.org/10.1590/1413-81232021263.10642020 [ Links ]
14. Lopes GDC, Gonçalves AC, Gouveia HG, Armellini CJ. Attention to childbirth and delivery in a university hospital: comparison of practices developed after Network Stork. Rev Lat Am Enfermagem[Internet]. 2019 [acesso 2021 Abr 16];27:e3139.Disponívelem: https://doi.org/10.1590/1518-8345.2643-3139 [ Links ]
15. Gama SGN, Viellas EF, Medina ET, Angulo-Tuesta A, Silva CKRT, Silva SD. Delivery care by obstetric nurses in maternity hospitals linked to the RedeCegonha, Brazil - 2017. Ciênc Saúde Colet [Internet]. 2021 [acesso 2021 Abr 17];26(3):919-29. Disponível em: https://doi.org/10.1590/1413-81232021263.28482020 [ Links ]
16. Ritter SK, Gonçalves AC, Gouveia HG. Care practices in normal-risk births assisted by obstetric nurses. Acta Paul Enferm [Internet]. 2020 [acesso 2021 Abr 17]; 33:eAPE20180284. Disponível em: https://doi.org/10.37689/acta-ape/2020AO0284 [ Links ]
17. Nucci M, Nakano AR, Teixeira LA. Synthetic oxytocin and hastening labor: reflections on the synthesis and early use of oxytocin in Brazilian obstetrics. Hist Cienc Saude Manguinhos [Internet]. 2018 [acesso 2021 Abr 17];25(4):979-98. Disponível em: https://doi.org/10.1590/S0104-59702018000500006 [ Links ]
18. Johansson C, Finnbogadóttir H. First-time mothers' satisfaction with their birth experience-a cross-sectional study. Midwifery [Internet]. 2019 [acesso 2021 Abr 22];79:102540. Disponível em: https://doi.org/10.1016/j.midw.2019.102540 [ Links ]
19. Pereira LR, Rodrigues GMM, Ferreira ES, Barros INM, Carneiro MS, Siqueira LS. Normal childbirth and interventions in a public maternity. Rev BaianaEnferm [Internet]. 2019 [acesso 2021 Abr 22];33:e-32631. Disponível em: http://dx.doi.org/10.18471/rbe.v33.32631 [ Links ]
20. Nascimento KIM, Lima VS, Novaes CDP, Ponte AR, Aragão CRB, Trindade GBM, et al. Manobra de Kristeller: uma violência obstétrica. Braz J Health Rev [Internet]. 2021 [acesso 2021 Abr 29];4(2):7362-80. Disponível em: https://doi.org/10.34119/bjhrv4n2-278 [ Links ]
21. Silva LF, Sanches METL, Santos AAP, Oliveira JCS, Acioli DMN, Santos JAM. Adesão às boas práticas obstétricas: construção da assistência qualificada em maternidades-escolas. Rev. baiana enferm [Internet]. 2021 [acesso 2021 Abr 29];35:e37891. Disponível em: http://dx.doi.org/10.18471/rbe.v35.37891 [ Links ]
22. Lucena TS, Morais RJL, Santos AAP. Analysis of partogram completion as good obstetric practice in the monitoring of labor. Rev Pesqui (Univ Fed Estado Rio J, Online). [Internet]. 2019 [acesso 2021 Abr 29];11(1):222-7. Disponível em: https://doi.org/10.9789/2175-5361.2019.v11i1.222-227 [ Links ]
23. Lima SBG, Schirmer J, Dotto LMG, Santos CL. Obstetric practices adopted by a public maternity in Rio Branco-AC. Cogitare Enferm [Internet]. 2018 [acesso 2021 Abr 29]; (23)4:e53258. Disponível em: http://dx.doi.org/10.5380/ce.v23i4.53258 [ Links ]
24. Medeiros AB,Freire ILS, Santos FR, Silva BCO, Batista GFM, Menezes MM. Partograma: instrumento de segurança no cuidado multidisciplinar. Rev Cuid (Bucaramanga. 2010). [Internet]. 2020 [acesso 2021 Mai 8];11(3):e1046. Disponível em: https://doi.org/10.15649/cuidarte.1046 [ Links ]
25. Tomasi YT, Saraiva SS, Boing AC, Delziovo CR, Wagner KJP, Boing AF. From prenatal care to childbirth: a cross-sectional study on the influence of a companion on good obstetric practices in the Brazilian National Health System in Santa Catarina State, 2019. EpidemiolServSaúde[Internet]. 2021 [acesso 2021 Mai 8];30(1):e2020383. Disponível em: http://dx.doi.org/10.1590/s1679-49742021000100014 [ Links ]
26. Ministério da Saúde (BR). Lei nº 11.108, de 7 de abril de 2005. Garante as parturientes o direito à presença de acompanhante durante o trabalho de parto, parto e pós-parto imediato, no âmbito do SUS. Diário Oficial da União, Brasília (DF), 2005 [acesso 2021 Abr 8]. Disponível em: http://www.planalto.gov.br/ccivil_03/_ato2004-2006/2005/lei/l11108.htm. [ Links ]
27. Souza HLR, Fernandes FECV, Pereira RCLF, Melo RA. Compreensão da enfermagem sobre o contato pele a pele entre mãe/bebê na sala de parto. Rev Enferm UFSM [Internet]. 2020 [acesso 2021 Mai 8];10(e93):1-19. Disponível em: https://doi.org/10.5902/2179769242729 [ Links ]
28. Bomfim ANA, Couto TM, Lima KTRS, Almeida LTS, Santos GO, Santana AT. Women's perceptions about nursing care during normal delivery. Rev Baiana Enferm [Internet]. 2021 [acesso 2021 Mai 8];35:e39087. Disponível em: http://dx.doi.org/10.18471/rbe.v35.39087 [ Links ]
29. Santos Filho SB, Souza KV. RedeCegonha network and the methodological challenges of implementing networks in the SUS. Ciênc Saúde Colet [Internet]. 2021 [acesso 2021 Mai9];26(3):775-80. Disponível em: https://doi.org/10.1590/1413-81232021263.21462020 [ Links ]
30. Gomes CBA, Dias RS, Silva WGB, Pacheco MAB, Sousa FGM, Loyola CMD. Prenatal nursing consultation: Narratives of pregnant women and nurses. Texto Contexto Enferm [Internet].2019 [acesso 2021 mai 9];28:e20170544. Disponível em: http://dx.doi.org/10.1590/1980-265X-TCE-2017-0544 [ Links ]
Received: July 23, 2021; Accepted: December 24, 2021











 text in
text in