My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.22 n.69 Murcia Jan. 2023 Epub Mar 20, 2023
https://dx.doi.org/10.6018/eglobal.524931
Originals
Spatiotemporal distribution and factors related to congenital syphilis in the brazilian northeast
1Department of Nursing, State University of Piauí, Parnaíba-PI, Brazil. geovana.almeida.santos123@gmail.com
2Department of Nursing, State University of Ceará, Fortaleza-CE, Brazil
Aim:
To analyze the spatiotemporal dynamics and socioeconomic factors associated with the incidence of congenital syphilis in the Brazilian Northeast from 2008 to 2018.
Method:
An ecological study conducted on cases of congenital syphilis in the Northeast and notified in the Information System of Notifiable Diseases. Methods of temporal and spatial analysis were applied to identify trends and clusters of the disease as well as a model of linear regression to point out indicators related to congenital syphilis with a 5% significance level.
Results:
The incidence of congenital syphilis has significantly increased in all states of the Northeast (p<0.001), with higher indexes and clusters mostly in municipalities of the coast region. The variables associated with the incidence of congenital syphilis in the Northeast were: percentage of alive newborns with low birth weight (p<0.001), Human Development Index (p<0.001), income per capita (p<0.001), percentage of poor people (p<0.001), percentage of people with 18 years or more with complete basic education (p<0.001), and illiteracy rate (p<0.001).
Conclusion:
it was verified that incidence of congenital syphilis during the period analyzed and high indexes clusters in the coast of the Northeast coast.
Keywords: Congenital syphilis; Risk factors; Time-series studies; Ecological studies
INTRODUCTION
The transmission of Congenital Syphilis (CS) occurs vertically, in other words, from the pregnant woman to the fetus via the placenta at any stage of pregnancy and during the childbirth, in cases in which pregnant women are not treated or are treated inappropriately. It is a disease of compulsory notification and considered, in epidemiological terms, an indicator of the quality of prenatal care of a population1)(2)(3.
According to the World Health Organization (WHO), approximately 1.5 million pregnant women are infected with syphilis annually4. Half of them are not treated and, consequently, will have children with adverse results, such as low birth weight, neonatal death and/or clinical evidence of infection5. In Brazil, in recent years, there has been a progressive increase in the incidence of congenital syphilis, since in 2010, the rate was 1.4 cases/1,000 live births (LB) and, in 2019, the rate increased to 8.2 cases/1,000 live births6. It should be noted that these values are well above the rate recommended by the Pan American Health Organization (PAHO), which is 0.5 cases for every thousand live births7,8.
In this way, inadequate prenatal care is one of the main factors responsible for the high incidence of congenital syphilis worldwide9. In addition, other factors are associated, such as poverty, human immunodeficiency virus (HIV) infection, drug abuse and lack of access to health services. Individual risk factors include pregnant adolescents, non-white race/color, low education, history of sexually transmitted infections (STIs), history of syphilis in previous pregnancies, multiple sexual partners and low income10. Many of these factors can still be observed in Brazil, especially in the Northeast region.
In face of the imminent regional inequalities and the need to point out the factors that are related to the incidence of congenital syphilis, it is necessary to adopt research methods that evaluate the problem both: time, to identify tendencies, and space, considering the specific socioeconomic characteristics of each location11.
Therefore, the results of this study will permit to understand how cases of congenital syphilis are being distributed over time and space, in addition to subsidizing the diagnosis of children's health situation, in order to contribute to the improvement of prevention, diagnosis, treatment and vigilance of congenital syphilis. From this point on, it will be possible to direct health actions in a specific way, answering the real needs of the Northeast region, as well as collaborating for the implementation of health policies that aim to intervene on inequalities between territories and helping to reduce congenital syphilis. In face of what was exposed, the study has as objective to analyze the space-time dynamics and socioeconomic factors associated with the incidence of congenital syphilis in the Northeast from 2008 to 2018.
MATERIAL AND METHOD
Epidemiological study, of ecological type, which is based on the use of geoprocessing tools and spatial analysis in health that had the Northeast region of Brazil as an area of interest. According to the last Brazilian demographic census of 2010, the population of the Northeast was 53,078,137 people, distributed in 1,794 municipalities and nine states, namely: Alagoas (AL), Bahia (BA), Ceará (CE), Maranhão (MA), Paraíba (PB), Pernambuco (PE), Piauí (PI), Rio Grande do Norte (RN) and Sergipe (SE)12. The unit of analysis of this study was the municipalities.
As a data source, databases from the Information System on Notifiable Diseases (SINAN) and the Information System on Live Births (SINASC) were used, available on the website of the Brazilian Department of Informatics of the Unified Health System (DATASUS). All cases of congenital syphilis that occurred and reported were selected, considering the municipality of residence of children under one year of age in the period from 2008 to 2018.
The raw data of CS cases in each year were tabulated in a Microsoft Office Excel spreadsheet and imported into the free software Joinpoint Regression Program version 4.6.0.0. The Annual Percentage Change (APC) was calculated with a confidence interval of 95% (95%CI), in which negative APC values indicate a decreasing tendency and positive values indicate an increasing tendency (13. The year of occurrence of CS was defined as the dependent variable and the incidence rates in each year as the independent variable.
To calculate the gross CS incidence rates, it was used the software TabWin v.4.14®. As the numerator of the formula, it was used the number of cases of CS among children under one year of age in each year considered for this study and, as a denominator, the number of live births in the population of each Northeastern municipality, also for each year, multiplied by 1,000 alive births. Gross rates were softened by the Local Empirical Bayesian method to correct random fluctuations, especially in municipalities with a few number of inhabitants14.
Two methods were used to identify spatial clusters. The first one corresponds to the spatial autocorrelation function, through the Global and Local Moran Index. The Moran Global Index was used to test the spatial dependence hypothesis and provide a general measure of association for the entire study area. Once the presence of global spatial autocorrelation was verified, the Local Moran Index (Local Index Spatial Analysis - LISA) was applied to verify the presence of spatial aggregates and quantify the degree of spatial association in each municipality of the sample set, considering it if p<0.0511.
Local Moran Index results are presented through the Moran Map and Lisa Map. The Moran Map allows to graphically visualize the degree of similarity between neighbors, being represented by four quadrants: in the first one the municipalities with high rates and that are close to municipalities with equally high rates (High/High spatial pattern); the second represents the municipalities that have low rates and are surrounded by municipalities that also have low rates (Low/Low spatial pattern); the municipalities in the third (High/Low spatial pattern) and in the fourth (Low/High spatial pattern) represent areas of epidemiological transition and have high and low rates, but they are very close to municipalities that have low and high rates, respectively11.
The second method used to detect spatial clusters of congenital syphilis was the analysis of purely spatial scanning using the Scan statistical technique. In addition to identifying spatial clusters, the scan is also able to locate areas at risk for congenital syphilis. The calculation of the relative risk (RR) was performed for each municipality in the Northeast, and those with values >1 have a relative risk for CS that is higher than the risk for the Northeast as a whole.
To compose the construction of the Ordinary Least Squares Estimation (OLS) multivariate linear regression model, ten socioeconomic indicators referring to the population of each Northeastern municipality were collected in the Portal of the Atlas of Human Development in Brazil15. The indicators included in the model were: percentage of live births with low birth weight; percentage of live births with at least seven prenatal consultations; Gini index of per capita household income; average household income per capita; Municipal Human Development Index (IDHM); percentage of women aged 10 to 17 who had children; fertility rate; percentage of 18 years of age or older with complete elementary education; illiteracy rate and percentage of poor individuals.
For the multivariate model, the incidence rates of congenital syphilis and socioeconomic information for all municipalities in the Northeast region were inserted, using the backward method and epidemiological criteria. The presence of collinearity between the independent variables was verified using the Variance Inflation Factor (VIF). Non-collinear variables were inserted into the OLS model, adopting a statistical significance of 5%. To calculate the OLS multivariate model, STATA v.12® software was used. Terra View v.4.2.2® software was used to obtain the neighborhood matrix and to calculate the Bayesian statistics. The non-spatial OLS regression was performed using the Stata 12® software. The maps were created using QGIS v.2.14.17® software.
This study was approved by the Research Ethics Committee of the State University of Piauí under assessment No 3,286,819 and CAAE No 07558218.7.0000.5209, respecting all ethical and legal aspects recommended by Resolutions No. 466/12 and No 510/16.
RESULTS
In the Northeast region of Brazil, 47,198 cases of congenital syphilis were reported from 2008 to 2018. Of these, most were female children (N=24,172;51.1%) aged between 0 and 6 days of life. (N=48,004; 95.9%) (Data not shown in table).
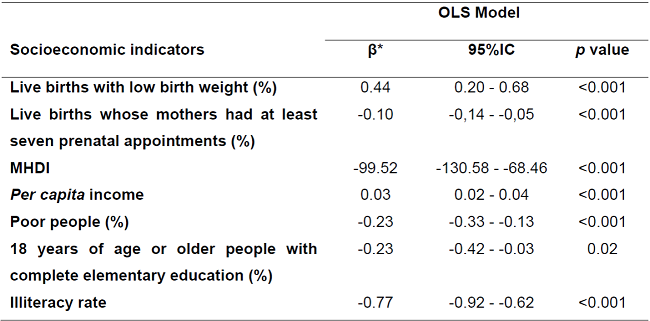
It was verified that the number of cases is higher among brown children (N=34,801; 84.7%), whose mothers were aged between 20 and 29 years (N=25,113; 54.6%), aged 7 years of study or less (N=23,984; 61.9%), who did prenatal care (N=38,730; 83.5%), who received a diagnosis of maternal syphilis during prenatal care (N=15,997; 54 .9%) and who had inadequate treatment (N=27,147; 64.3%) (Table 1).
Table 1: Sociodemographic characterization of congenital syphilis cases in Northeast Brazil in the period 2008-2018. Parnaíba, Piauí, Brazil. (N=47,198).
*Missing cases were excluded (missing/ignored) for the following variables: child's race/color (n=9,117), mother's age group (n=1,211), mother's education (n=10,966), prenatal care birth (n=3,791), time of diagnosis of maternal syphilis (n=2,565) and maternal treatment schedule (n=5,018).
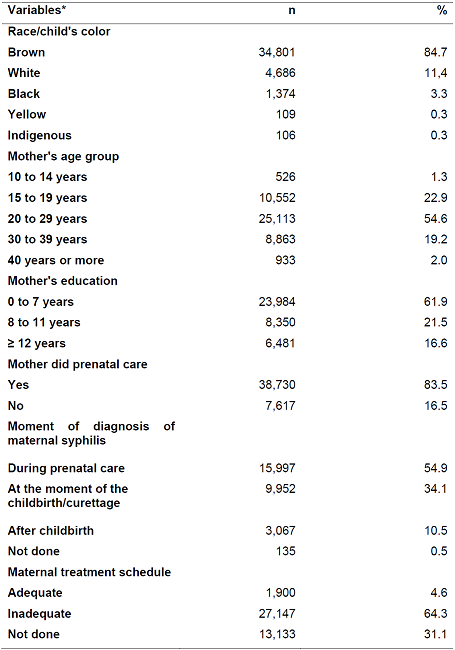
The temporal analysis by Joinpoint shows that the Northeast region presented an increase of 16.9% per year (95%CI: 13.7 - 20.2; p<0.001) in the rates of congenital syphilis. In the analysis of the tendency by state, a significant growth in the rates of the disease was observed in all the northeastern states in the analyzed period (p<0.001). Piauí was the state that presented the most expressive increase, with growth of 44.4% per year (95%CI: 31.8 - 58.1; p<0.001), followed by Bahia, with growth of 24.4% per year. year (95%CI: 17.3 - 31.9; p<0.001) (Table 2).
Table 2: Annual Percentage Variation of congenital Syphilis cases in Northeast Brazil in the 2008-2018 Period. Parnaíba, Piauí, Brazil.
*CI95% Confidence Index of 95%.
Through spatial analysis, it is possible to observe that map 1A demonstrates a non-random spatial pattern of high gross rates of congenital syphilis in very specific territories, such as the metropolitan regions of capitals located on the coast and in some points in the interior of the states of Piauí, Maranhão, Bahia and Ceará (Figure 1A). The local empirical Bayesian method showed a more apparent spatial pattern (Figure 1B). This method generated indicators that confirmed a regional pattern of high rates and practically extinguished the municipalities with a coefficient equal to zero.
The thematic map of the Bayesian incidence of congenital syphilis shows that most Northeastern municipalities have rates ranging from 0.01 to 4.52 cases/1,000 LB. In addition, it appears that the highest rates (≥4.52 cases/1,000NV) are located in municipalities located primarily along the coast of all northeastern states (Figure 1B).
In addition, large-scale clusters with a high/high distribution pattern of congenital syphilis were identified in coastal municipalities in seven of the nine northeastern states, encompassing, above all, the metropolitan regions of capital cities. On the other hand, in Maranhão and Piauí, the high/high standard of SC was observed in municipalities located in the interior of these states, with emphasis on the polygons corresponding to Teresina, capital of the state of Piauí, and Imperatriz, the second-largest city in the state from Maranhão (Figure 1C). All municipalities that showed some spatial pattern on the Moran Map (Figure 1C) showed statistically significant autocorrelation on the Lisa Map with p<0.05 (Figure 1D).
The Scan technique identified 16 clusters, however, only 12 had statistical significance (p<0.05). The primary cluster (p<0.001) has the lowest probability of having occurred by chance and included 593 municipalities, belonging to the states of Ceará, Rio Grande do Norte, Paraíba, Pernambuco and Sergipe (in red). It should be noted that all other states had statistically significant secondary clusters (p<0.05) of congenital syphilis cases (in yellow) (Figure 1E).
The technique also made it possible to identify the risk of illness due to congenital syphilis in the Northeastern municipalities. Thus, it was found that in most of them, the risk of illness is lower than the risk of the region as a whole (blank). In dark green, the municipalities that presented the highest Relative Risks in the region (RR=2.36 - 3.73) among them, four capitals stand out: Maceió (AL), Recife (PE), Natal (RN) and Fortaleza (CE). In addition to these capitals, Teresina (PI), as well as Aracaju (SE), São Luís (MA) and Salvador (BA) also stand out, which presented 1.0 to 2.4 times more risk of CS compared to all other Northeastern municipalities (Figure 1F).
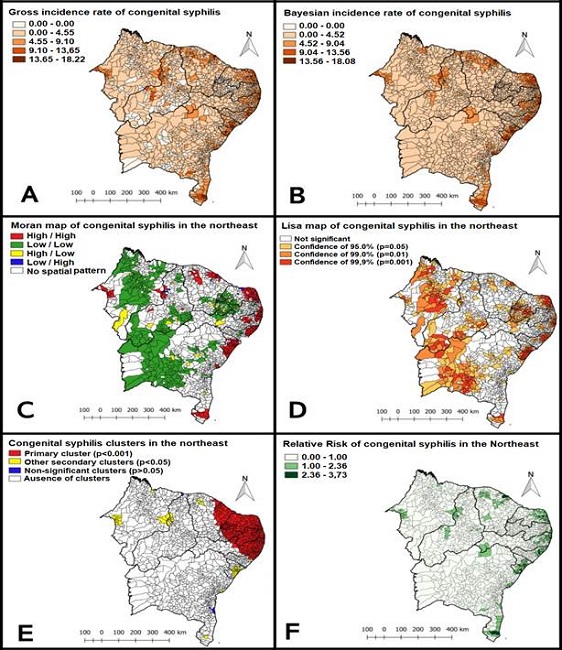
Figure 1: Gross incidence rate of congenital syphilis (A), Incidence rate of congenital syphilis softened by the local empirical Bayesian method (B), Moran Map (C), Lisa Map (D), Clusters (E) and Relative Risk for incidence of congenital syphilis (F). Northeast, Brazil, 2008-2018.
Table 3 presents detailed information on statistically significant clusters (p<0.05) of congenital syphilis in the Northeast region. The primary cluster has a radius of 742.10 km and its municipalities present a 2.28 times higher risk of children being infected with congenital syphilis compared to the entire study area (Northeast).
Table 3: Spatial clusters of congenital syphilis cases, defined by the purely spatial Scan statistic. Northeast, Brazil, 2008 - 2018.
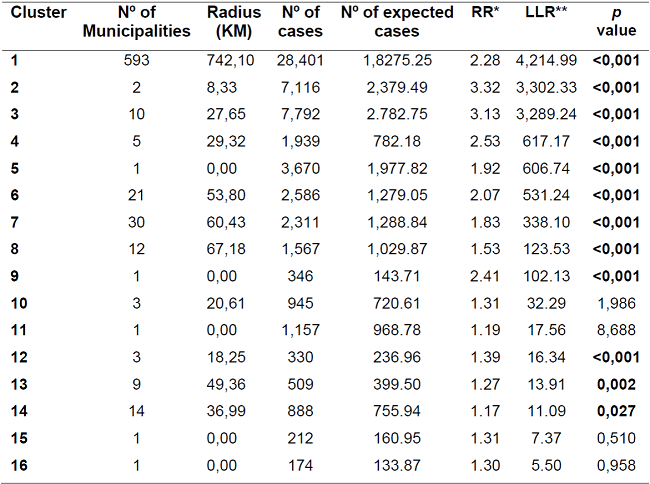
*RR: Relative risk for the cluster compared to the rest of the Northeast region.
**LLR: Logarithmic likelihood ratio test.
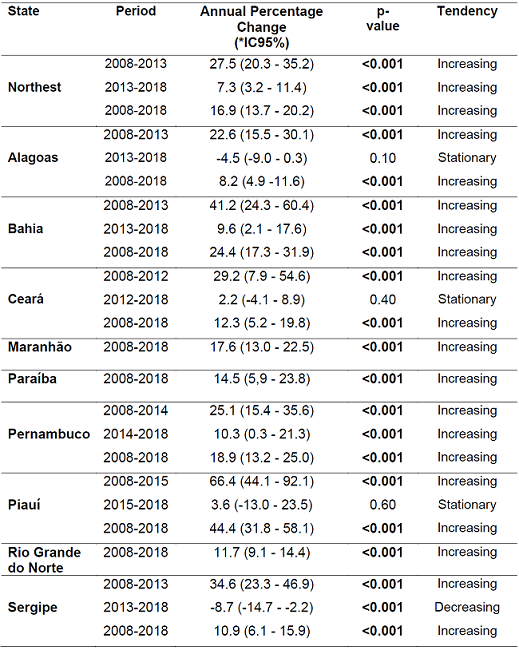
The OLS pointed out that the variables' percentage of live births with low birth weight (β=0.44; p<0.001) and per capita income (β=0.03; p<0.001) have a positive and significant association with the dependent variable. This demonstrates that the higher the values of these variables are, the higher the incidence of congenital syphilis in the region. It was also found that the variables' percentage of live births whose mothers have at least seven prenatal consultations (β=-0.10; p<0.001), MHDI (β=-99.52; p<0.001), percentage of poor people (β=-0.23; p<0.001), percentage of people aged 18 or over with complete elementary school (β=-0.23; p=0.02) and illiteracy rate (β= -0.77; p<0.001) had a significant negative association with the incidence of congenital syphilis. (Table 4). In the OLS, the coefficient of determination (R2) was 0.16 and the VIF was 2.82 (Table 4).
DISCUSSION
In this study, we highlight the higher incidence of congenital syphilis among children whose mothers are young women between 20 and 29 years old, in line with findings already reported in the literature3)(10)(16. This age group, as it represents the peak of a woman's reproductive life, justifies the highest number of reported cases. In addition, sexual behavior, such as the lack of condom use and multiple partners, may be related to the risk of acquiring STIs, including syphilis17.
The largest record of cases was of children whose mothers did prenatal care. Given this result, it can be inferred that the quality of prenatal care needs more strategic and educational actions to qualify the treatment18,19. In this way, a study carried out in Piauí showed that, of the cases in which mother-concept transmission occurred, 82.4% of the pregnant women did prenatal care and, of those, only 40.4% of the diagnoses occurred during pregnancy20.
The incidence rates of CS in the Northeast region showed progressive growth over the years studied, with an average rate almost 10 times higher than the reference rate recommended by PAHO7,8. Studies carried out in different Brazilian territories have also shown a tendency for CS to increase throughout the national territory17)(21)(22.
The fact that capitals and metropolitan regions of large cities present clusters of high SC rates may be reflecting a more reliable notification system in relation to other smaller municipalities. In addition, the increase in disease notifications during prenatal care in recent years, may be associated with the strengthening of maternal and child care services, which occurred especially after the implementation of the Rede Cegonha program. This program provided an increase in the coverage of testing of pregnant women for diagnosis in a timely manner, especially in regions that have a wide network of health services offered to the population, which facilitates the detection of cases1,12.
Through regression analysis, it was observed that the percentage of live births with low birth weight has a directly proportional association with the incidence of congenital syphilis. This indicator expresses intrauterine growth retardation and represents an important risk factor for neonatal and infant morbidity and mortality. High proportions of live births with low birth weight are generally related to low levels of socioeconomic development and maternal and child care23. National studies corroborate this result, since congenital syphilis is particularly one of the main causes of low birth weight16,23.
A negative association was also evidenced between the percentage of live births whose mothers had at least seven prenatal appointments and congenital syphilis. In Brazil, the Ministry of Health launched the Program for Humanization in Prenatal and Birth (PHPN) in 2000. Among the recommendations, the document guides pregnant women to make at least six prenatal care appointments during pregnancy: one in the first trimester, two in the second and three in the third24. Monitoring from the first trimester of pregnancy enables laboratory tests to be carried out and can reduce maternal and infant morbidity and mortality25. A study pointed out that women with a low frequency of prenatal appointments express a higher risk for the occurrence of syphilis. This effect reduces as the number of prenatal care appointments increases26. It should be noted that the occurrence of congenital syphilis is used as a sensible indicator for assessing the quality of prenatal care27.
It was observed that the MHDI showed an inversely proportional relationship with the incidence of congenital syphilis. A study conducted in Rio Grande do Sul showed a contrary result to this investigation, as the municipalities with the highest MHDIs in the state had more cases of SC compared to the municipalities with the lowest MHDIs. This fact may be the result of better care conditions in health units and, in this way, represent greater access to diagnosis and higher notification rates21.
In this study, the higher the per capita income, the higher the incidence of congenital syphilis. Most people affected by syphilis in the Americas are the most impoverished and marginalized individuals28. Even if syphilis is not restricted to the most disadvantaged populations, studies indicate that low education and low income are factors that directly influence the persistence of this disease29,30. However, it should be noted that the paradoxical result found in this investigation is probably due to better conditions of care in health units in territories where spatial clusters were identified, as consequence, better access to diagnostic methods, and higher rates of notifications21.
A study carried out in Brazil from 2001 to 2017 corroborates this result, with the most economically developed regions showing increasing tendency in congenital syphilis cases. This fact is associated with advances in the epidemiological surveillance system, use of rapid tests, qualification of health professionals and expansion of patients' access to the basic health system22.
The percentage of poor people was negatively associated with congenital syphilis. This result contrasts with those obtained by a study carried out in Pará, which showed that conditions of vulnerability directly influence the increase in cases of congenital syphilis11. It is noteworthy that living conditions influence the determination of CS, showing a higher occurrence of this disease in the most impoverished portion of the population. This is due to the difficulty of pregnant women with low income to have access to quality prenatal care, with the opportunity for diagnosis and treatment1,26. On the other hand, a Brazilian research carried out in 2013 showed that 61.3% of pregnant women had seven or more prenatal care appointments. Most of these women had a high level of education, lived in the Southeast and South regions and were older (40 years or more), showing that syphilis can affect individuals from all social classes24.
A negative relationship was observed between the percentage of people aged 18 years and over, with complete primary education, and the incidence of CS. Therefore, studies have shown that maternal education is associated with cases of congenital syphilis11,8. In addition, it is believed that people with low education are in a situation of social vulnerability, which influences less access to information3. Low schooling is a major obstacle for the government to eradicate congenital syphilis, as the understanding of the disease, in addition to its treatment, is essential for the progress11.
The negative relationship found in this study between SC and the illiteracy rate is probably due to the reduction observed over time in the percentage of people from Northeast who cannot read and write. Over the last decade, the Ministry of Education has built a systemic policy to fight illiteracy. With the Brasil Alfabetizado Program, additional resources were allocated to train literacy teachers, purchase teaching materials, school meals and student transportation. Thus, a reduction in illiteracy among young people and adults was observed in the Northeast, from 50.0% in 2012 to 37.2% in 201831.
It is important to emphasize that some results of this study should be interpreted with caution. Although some predictor variables, such as the percentage of live births with at least seven prenatal appointments and per capita income, have shown statistical significance in the OLS model, their estimated coefficients are very close to zero, demonstrating that the effect of these indicators on the outcome variable is small. Another limitation presented in this study is related to the ecological delimitation, as the analysis of variables at the population level does not necessarily represent an association at the individual level. In addition, the use of secondary data may present inconsistencies in terms of their quantity and quality. However, it should be noted that such limitations do not make it impossible to carry out the research and do not reduce its importance.
CONCLUSION
It was observed a significant growth in SC rates in the Northeast region, with emphasis on the state of Piauí. It was found that the highest rates are concentrated in municipalities located primarily along the coast of all northeastern states. In addition, it was observed that the variables associated with the incidence of congenital syphilis were: percentage of live births with low birth weight, percentage of live births with at least seven prenatal appointments, MHDI, per capita income, percentage of poor people, percentage of people aged 18 or over with complete primary education and illiteracy rate.
The implementation of improvements in the quality of prenatal care is essential to combat congenital syphilis, as well as the development of strategies that facilitate the adherence of pregnant women to prenatal care. Therefore, disease prevention strategies should be directed to the municipalities with the highest occurrence, in order to make public health actions more effective, in addition to ensure an improvement in the population's living conditions.
REFERENCIAS
1. Soares KKS, Prado TN, Zandonade E, Silva SFM, Miranda AE. Análise espacial da sífilis em gestantes e sífilis congênita no estado do Espírito Santo, 2011-2018. Epidemiol. Serv. Saúde. 2020; 29(1):1-12.https://doi.org/10.5123/S1679-49742020000100018 [ Links ]
2. Mamede LRLS, Silva AMTC, Almeida RJ. Análise epidemiológica da sífilis materna e congênita: uma revisão sistemática. Revista Saúde (Sta. Maria). 2021; 47. https://doi.org/10.5902/2236583461351 [ Links ]
3. Conceição HN, Câmara JT, Pereira BM. Análise epidemiológica e espacial dos casos de sífilis gestacional e congênita. Saúde Debate. 2019; 43 (123): 1145-1158. https://doi.org/10.1590/0103-1104201912313 [ Links ]
4. World Health Organization (WHO). Guidelines for the treatment of Treponema pallidum (syphilis). Geneva: WHO; 2016. [cited Jan 09, 2021]. Available from: https://apps.who.int [ Links ]
5. Holzmann APF, Barros SMO, Silva CSO, Barbosa D. Sífilis materna e sífilis congênita: avaliação da assistência hospitalar. Temas em Saúde. 2018;18(3):148-177. https://doi.org/10.29327/213319.18.3-9 [ Links ]
6. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde, Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis (DCCI). Boletim Epidemiológico - Sífilis. Ano VI - nº 01. Brasília: Ministério da Saúde, 2020. [cited Jan 08, 2020]. Available from: http://www.aids.gov.br/pt-br/pub/2020/boletim-sifilis-2020 [ Links ]
7. Costa JS, Santos-Júnior FM, Moreira RS, Góes MAO. Tendência temporal da sífilis congênita em Sergipe, Brasil, 2006 - 2017. Rev. Saúde Col. 2019; 9: 8-15. https://doi.org/10.13102/rscdauefs.v9i0.3356 [ Links ]
8. Bastos Neto BC, Souza IM, Santos, L.P.S. Análise temporal da incidência de sífilis congênita no Brasil, 2007-2016. Arq Med Hosp Fac Cienc Med Santa Casa. 2020; 65(22). https://doi.org/10.26432/1809-3019.2020.65.022 [ Links ]
9. Nonato, S.M; Melo, A.P.S; Guimarães, M.D.C. Sífilis na gestação e fatores associados à sífilis congênita em Belo Horizonte-MG, 2010-2013. Epidemiol. Serv. Saúde. 2015; 24(4):681-694. https://doi.org/10.5123/S1679-49742015000400010 [ Links ]
10. Almeida AS, Andrade J, Fermiano R, Jamas MT, Carvalhaes MABL, Parada CMGL. Sífilis na gestação, fatores associados à sífilis congênita e condições do recém-nascido ao nascer. Texto & Contexto Enfermagem. 2021; 30, e20200423. https://doi.org/10.1590/1980-265X-TCE-2020-0423 [ Links ]
11. Carmo BAG, Santos DF, Hayase KAS, Santos MMQ, Naiff GRO, Botelho EP. Sífilis congênita em região da Amazônia brasileira: análise temporal e espacial. Rev. Eletr. Enferm. [Internet]. 2020; 22:62349. https://doi.org/10.5216/ree.v22.62349 [ Links ]
12. Instituto Brasileiro de Geografia e Estatística (IBGE). Censo demográfico 2010. Brasília: IBGE, 2010. [cited Jan 08, 2020]. Available from: http://censo2010.ibge.gov.br/ [ Links ]
13. Sousa GJB, Garces TS, Pereira MLD, Moreira TMM, Silveira GM. Temporal pattern of tuberculosis cure, mortality, and treatment abandonment in Brazilian capitals. Rev Latino-Am Enfermagem. 2019; 27:e3218. https://doi.org/10.1590/1518-8345.3019.3218 [ Links ]
14. Brasil. Ministério da Saúde. Abordagens Espaciais na Saúde Pública. Brasília: Ministério da Saúde, 2006. [cited Jan 08, 2020]. Available from: http://bvsms.saude.gov.br/bvs/ [ Links ]
15. Programa das Nações Unidas para o Desenvolvimento (PNUD). Atlas do Desenvolvimento Humano no Brasil [Internet], 2021. [cited Jul 04, 2020]. Available from: http://www.atlasbrasil.org.br/ [ Links ]
16. Silva IMD, Leal EMM, Pacheco H, Souza Júnior JG, Silva FS. Perfil epidemiológico da sífilis congênita. Rev enferm UFPE on line. 2019;13(3): 604-613. https://doi.org/10.5205/1981-8963-v13i03a236252p604-613-2019 [ Links ]
17. Souza BSO, Rodrigues RM, Gomes RML. Análise epidemiológica de casos notificados de sífilis. Rev Soc Bras Clin Med. 2018; 16(2): 94-8. [ Links ]
18. Slutsker JS, Hennessy RR, Schillinger JA. Factors Contributing to Congenital Syphilis Cases - New York City, 2010-2016. Morb Mortal Wkly Rep. 2018;67(39):1088-93. https://doi.org/10.15585/mmwr.mm6739a3 [ Links ]
19. Holztrattner JS, Linch GF da C, Paz AA, Gouveia HG, Coelho DF. Sífilis congênita: realização do pré-natal e tratamento da gestante e de seu parceiro. Cogitare enferm. 2019; 24: e59316. http://dx.doi.org/10.5380/ce.v24i0.59316 [ Links ]
20. Barbosa DRM, Almeida MG, Silva AO, Araújo AA, Santos AG. Perfil epidemiológico dos casos de sífilis gestacional. Rev. enferm. UFPE on line. 2017; 11(5). https://doi.org/10.5205/1981-8963-v11i5a23335p1867-1874-2017 [ Links ]
21. Teixeira LO. Tendência temporal e distribuição espacial da sífilis congênita no estado do Rio Grande do Sul entre 2001 e 2012. Ciência & Saúde Coletiva [online]. 2018; 23(8):2587-2597. [ Links ]
22. Oliveira VS, Rodrigues RL, Chaves VB, Santos TS, de Assis FM, Ternes YMF, Aquino EC. Aglomerados de alto risco e tendência temporal da sífilis congênita no Brasil. Rev Panam Salud Publica. 2020; 44: 1-9. https://doi.org/10.26633/RPSP.2020.75 [ Links ]
23. Domingues RSRM, Leal, M.C. Incidência de sífilis congênita e fatores associados à transmissão vertical da sífilis: dados do estudo Nascer no Brasil. Cad. Saúde Pública. 2016; 32(6). https://doi.org/10.1590/0102-311X00082415 [ Links ]
24. Nunes ADS, Amador AE, Dantas APQM, Azevedo UM, Barbosa IR. Acesso à assistência pré-natal no brasil: análise dos dados da pesquisa nacional de saúde. Revista Brasileira em Promoção da Saúde. 2017; 30(3). https://doi.org/10.5020/18061230.2017.6158 [ Links ]
25. Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané SG, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes-Estimates for 2016 and progress since 2012. PLoS ONE. 2019; 14(2): e0211720. https://doi.org/10.1371/journal.pone.0219613 [ Links ]
26. Macêdo VC, Lira PIC, Frias PG, Romaguera LMD, Caires SFF, Ximenes RAA. Fatores de risco para sífilis em mulheres: estudo caso-controle. Rev Saude Publica. 2017; 51(78): 1-12. https://doi.org/10.11606/S1518-8787.2017051007066 [ Links ]
27. Alves PIC, Scatena LM, Haas VJ, Castro SS. Evolução temporal e caracterização dos casos de sífilis congênita em Minas Gerais, Brasil, 2007-2015. Ciência & Saúde Coletiva. 2020; 25(8): 2949-2960. https://doi.org/10.1590/1413-81232020258.20982018 [ Links ]
28. Pan American Health Organization (PAHO). Elimination of mother-to-child transmission of HIV and syphilis in the Americas. Update 2016. Washington DC: PAHO; 2017. [cited Mar 12, 2021]. Available from: https://iris.paho.org/ [ Links ]
29. Souza CDF, Machado MF, Correia DS, Carmo RS, Cuevas LE, Santos VS. Spatiotemporal clustering, social vulnerability and risk of congenital syphilis in northeast Brazil: an ecological study. Trans R Soc Trop Med Hyg. 2020; 0: 1-9. https://doi.org/10.1093/trstmh/traa034 [ Links ]
30. Andrade E, Valvassori PMD, Mingote ACA, Guedes AL de L, Nogueira MC. Epidemiologia da sífilis congênita no Brasil: Uma revisão sistemática. Principia [Internet]. 2021; 20(23). https://doi.org/10.34019/2179-3700.2020.v20.31004 [ Links ]
31. Pesquisa Nacional por Amostra de Domicílios Contínua (PNAD). Ministério do Planejamento, Desenvolvimento e Gestão. Instituto Brasileiro de Geografia e Estatística - IBGE. Diretoria de Pesquisas. Coordenação de Trabalho e Rendimento. Notas técnicas. Versão 1.5. Rio de Janeiro. 2018. [cited Jan 08, 2020]. Available from: https://biblioteca.ibge.gov.br/ [ Links ]
Received: May 22, 2022; Accepted: September 21, 2022











 text in
text in