My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.22 n.69 Murcia Jan. 2023 Epub Mar 20, 2023
https://dx.doi.org/10.6018/eglobal.537891
Originals
Description of the Care Burden for a family with an elderly risk of dementia
1Poltekkes Kemenkes Jakarta III, West Java, Indonesia. raden.maryam@poltekkesjakarta3.ac.id
Introduction:
Dementia is one of the leading causes of dependence among the elderly worldwide and has a physical, psychological, social, and economic impact, especially on their families. Early recognition of the caring burden for the elderly at risk of dementia is important to prevent deterioration.
Objective:
This study aims to obtain an overview of the care burden for the elderly at risk of dementia in the community.
Methods:
This descriptive study involves a population of all the elderly living with their families in the Jakarta area with a random sampling of 168 respondents. The screening instrument for modifying the care burden of families consists of 21 items.
Results:
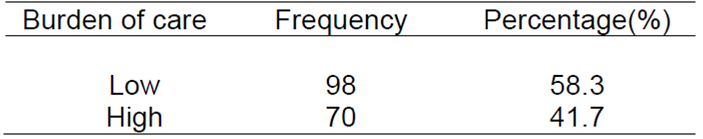
Most elderly are at risk of dementia, accounting for 72%, 73.2% have a chronic disease, and 73.8% are still independently doing BADL. Furthermore, 58.3% of the families have a low burden of care.
Conclusion:
The burden experienced by the elderly and their families influences their life quality. It is hoped that families with older members continue to improve and maintain their quality of life by remaining active and productive in fulfilling their needs and pleasures.
Keywords: burden of care for family; elderly; risk of dementia
INTRODUCTION
The elderly population in the Jakarta area is estimated to increase by 5.13% between 2010 and 2035, from 9.6 million to 16.39% of the total population, which is 11.5 million. Likewise, life expectancy in 2010-2015 was 71.6 years and is expected to increase to 73.9 years in 2030-20351. This shows that the increase in the elderly population is accompanied by increasing age.
According to the theory of functional consequences, changes in body function accompany increasing age2). These changes are caused by the aging process and the accompanying risk factors. The theory of biological aging explains the decline in cell function, which accelerate tissue damage and affects changes in the function of the human body system. The nervous system experiences changes in structure and function due to aging in the elderly, characterized by a decline in thinking and remembering processes.
The decline in the thinking and remembering process in the elderly is known as dementia. It is a collection of symptoms of cognitive deficits that are continuous and progressive, including the decline in memory, language skills, intellectual, and other brain functions. Therefore, they interfere with daily activities and are generally accompanied by behavioral and psychological changes3,4. It is also defined as a decrease in independence and at least one of the powers of concentration, learning, memory, language, daily activities, and the function of understanding the feelings and thoughts of others5.
The prevalence of dementia increases with age. Various studies show that this incidence doubles every 6.3 years, from 3.9 per 1000 people yearly at the age of 60-64 years to 104.8 per 1000 people at 90 years and above6. Its prevalence in Indonesia in 2015 reached 1.2 million people, with an estimated increase to 1.9 million in 2030 and almost 4 million in 20507. This makes dementia a health problem that can influence the life quality of individuals, family, friends, and the community.
Dementia impairs the cognitive and other abilities of the elderly, necessitating the assistance of family members to carry out their daily activities. The impact of this health problem and the time needed for treatment can cause stress and become a burden to their families. This is consistent with the results of a qualitative study that various cognitive and behavioral changes in the elderly can cause stress for their families8. Psychosocial responses that arise when caring for partners include anxiety and confusion, boredom and exhaustion, and positive responses experienced by caregivers are a sense of gratitude and resignation9.
Other qualitative studies yielded several themes about family knowledge of dementia symptoms, including struggle and despair, family as a source of stress, limited knowledge and misunderstanding, not being diagnosed with dementia, and not comprehending medical care10. Families who care for the elderly with complex health problems experience a high subjective burden. Some factors that play a major role in reducing the burden on families include health status, knowledge, caring satisfaction, and social support from the family11,12. Furthermore, reducing the care burden through social and formal support is a way coping skills can boost psychological resilience13.
Family health can be affected by the care burden for the elderly with health problems. The elderly with disabilities often negatively perceive their health and become dependent. This is consistent with the opinion that caring for someone with serious cognitive problems can impact the welfare of their caregivers14,15. Furthermore, this situation can be surmounted by educating and preparing family, relatives, friends, and elderly observers to optimally provide care in a way that meets their physical, emotional, social needs social, and financial needs. Families providing care for the elderly must be able to address their physical, psychological, social, and spiritual needs2,16. This is supported by studies' results that people with dementia need care, daily activities, and social activities. Meanwhile, informal caregivers need social activities, information about dementia care and the health care system, and emotional support17.
Dementia care for caregivers and support for the health care system are part of the WHO global action and the strategic plan for managing Alzheimer's disease and other dementias by the Ministry of Health, Indonesia. It is hoped that the prevention and treatment of people with dementia can be initiated as early as possible, starting from the family level. The family as a support system for the elderly is crucial to the application of this study's results. They can participate in providing services to the elderly and contribute to preventing and controlling disease risk factors.
Based on the existing problems and phenomena, this study aims to provide an overview of the care burden for families of the elderly with dementia risk in the Jakarta area.
METHODOLOGY
This is a descriptive study with a population of all families with elderly in the Jakarta area. Two areas were taken randomly to obtain a sample of 168 elderly in East and south Jakarta. The data collection tool is a modification of the Screening for Caregiver Burden, which consists of 21 items. This tool was used to objectively and subjectively measure the experience of the caregivers11,18. It used a five-point Likert scale (0-4), including “no experience”, “there is experience but no difficulty”, “there is experience with a low difficulty level”, “there is experience with a medium difficulty level”, and there is experience with a high difficulty level”. The total score is 84, and the validity and reliability test results using Cronbach's Alpha is 0.888.
This study passed the ethical review from the Faculty of Nursing Ethics Committee, the University of Indonesia, with Number 46/UN2.F12.D/HKP.02.04/2018. It applied three basic ethical principles, namely respecting the dignity of others, not harming, and fairness. The consent of the respondent was obtained by the consent form voluntarily. All data is kept confidential and used for study purposes.
RESULTS
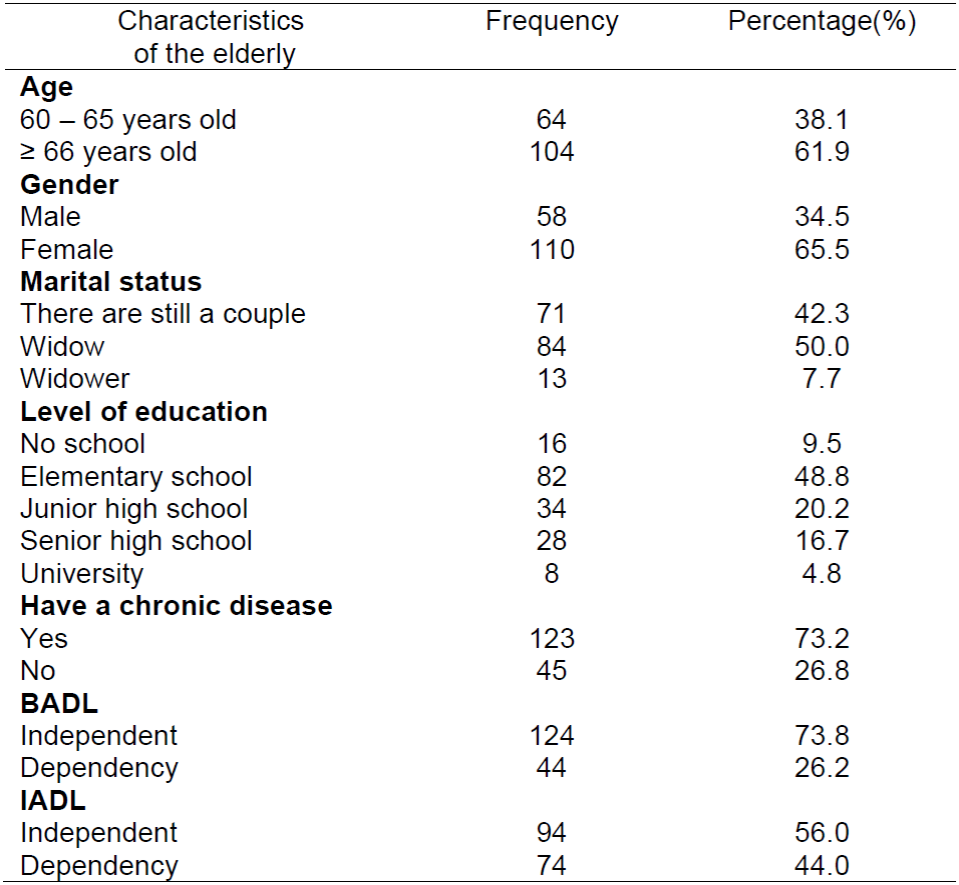
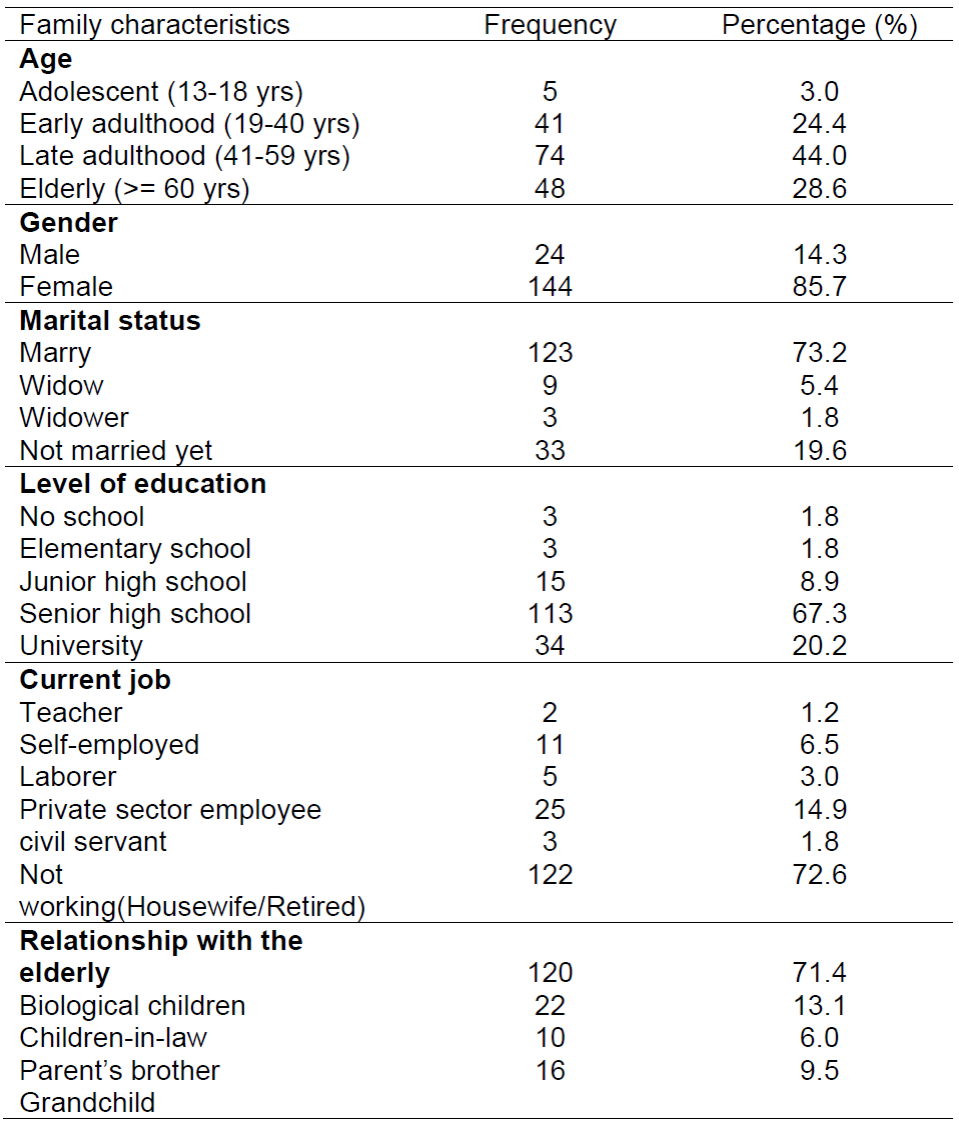
Table 1 gives a detailed description of the characteristics of the elderly. A total of 168 elderly people living with their families participated in the study. Most were 66 years at 61.9%, 65.5% were female, and 48.8% attained elementary school education. Most are capable of performing instrumental activities of daily living (IADL), such as using the telephone, shopping, preparing food, managing the house, washing, using transportation, preparing and taking medicine, and managing finances, accounting for 56%. Furthermore, 73.8% can carry out their daily activities (BADL) independently, such as eating, bathing, moving, going to the bathroom, urinating/defecating, and dressing. The examination of cognitive function status in the elderly was carried out using the Indonesian version of the Hopkins Verbal Learning Test (HVLT) instrument. The result showed that 72% of the elderly in the Jakarta area are at risk of dementia, as shown in Table 2.
Table 2. Distribution of the elderly by cognitive function status using HVLT examination in the Jakarta Area in 2020 (N=168).
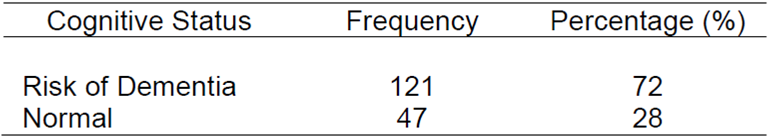
Table 3 describes the families' characteristics who care for the elderly. The most family age is late adulthood at 44%, 85.7% are female, and 73.2% are married. Furthermore, the highest education level is senior high school at 67.3%, and most families who care for the elderly are housewives, accounting for 72.6 %. Biological children mostly dominated the relationship at 71.4%.
DISCUSSION
The results showed that most of the elderly are female and over 66 years of age, with a 72% risk of dementia. This data is consistent with the result of a study that 66 years and above is significantly associated with the risk of dementia (p-value 0.026) and the elderly have a 2.7 times risk of developing the health problem compared to those aged 60-65 years19. An increase in life expectancy will increase cases of degenerative diseases, including dementia. Furthermore, an increase in the number of elderly will increase the need for health infrastructure20,21. The Elderly Posyandu, which is Integrated Service Post, is one of the effective health services established by the Public Health Center program. It provides counseling about health problems for the elderly.
The majority of family members who care for the elderly are biological children, married, and senior high school graduates. Furthermore, the family is the best caregiver for the elderly and is also the smallest unit that has the power to influence society. It becomes the main target in realizing a healthy society through the healthy behavior of every member. Generally, the role and power structure of the family has a significant effect on public health16.
The analysis showed that most of the average item scores indicated “no experience” with the 21 subjective and objective statements. Some of the items include: the elderly can still recognize their families, do not ask the same thing repeatedly, and the family does not feel ashamed to accompany the elderly outside. This shows that most elderly have not been diagnosed with dementia and can still carry out independent activities. Therefore, their care is not a heavy burden for the families.
The description of the statement items also shows that the majority indicated that they lacked experience caring for elderly at risk of dementia with high dependency levels. This is evident in some of their statements in Table 4, such as the elderly do not recognize me often; they suddenly threw, attacked, and threatened other family members and me; “I feel ashamed to take the elderly out of the house for fear that they will do something inappropriate or embarrassing”. The statements above showed that most families do not have the experience. However, they can still take good care of the elderly without being a burden because they are yet to suffer from dementia. Feelings of frustration, worry, sadness, fatigue, shame, and feeling alone are mostly not experienced by the family. The results showed that the care burden for the family was still at a low level of 58.3%.
Table 4. Distribution of the burden of caring for families with elderly at risk of dementia in the Jakarta Region in 2020 (N=168).
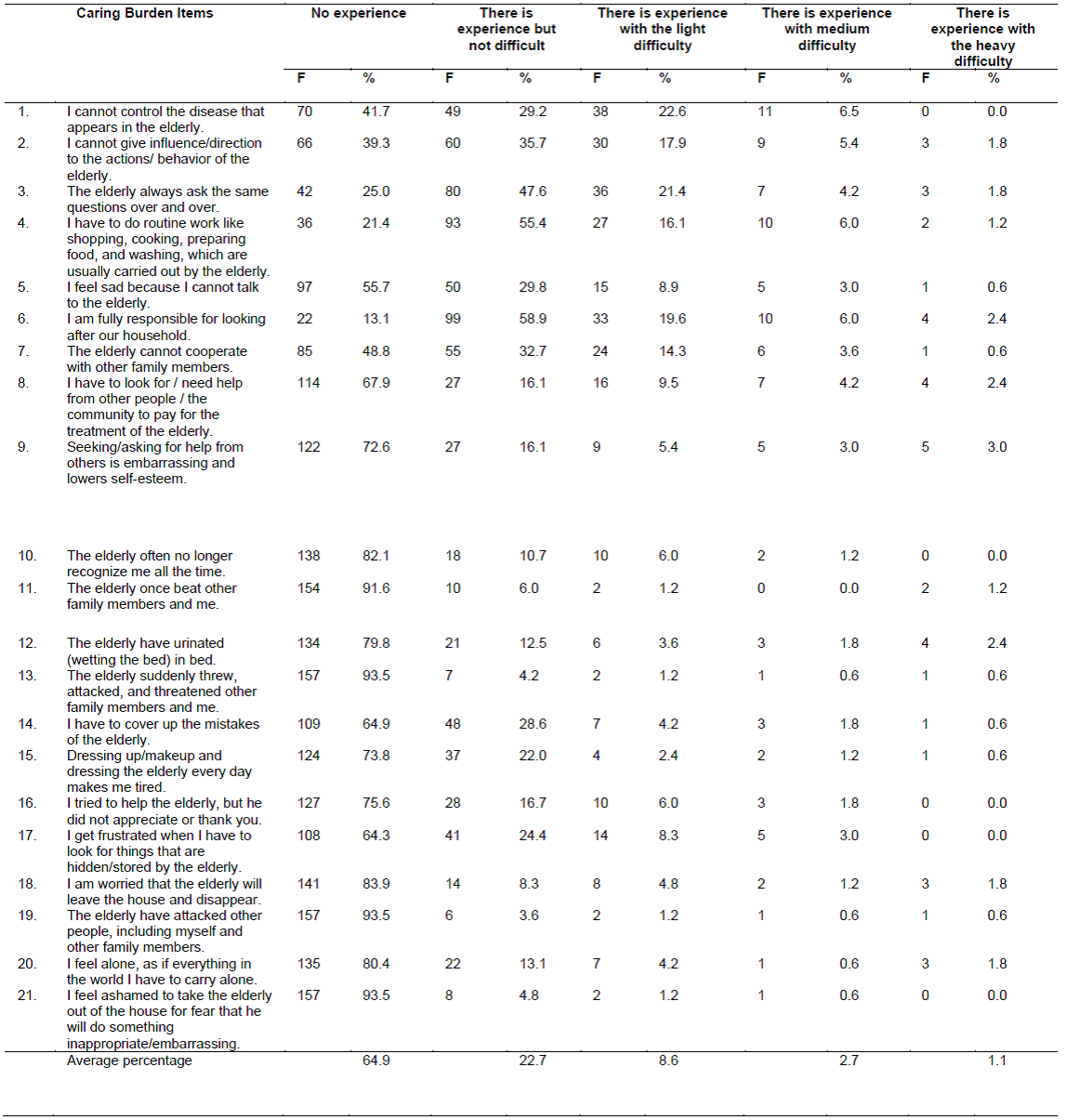
Table 5. Distribution of the burden of caring for families with elderly at risk of dementia in the Jakarta Region in 2020 (N=168).
This is contrary to the results of a qualitative study, which showed that boredom and fatigue are the psychosocial responses that occur when caring for a partner with dementia9. Furthermore, negative aspects related to health services can be a burden for caregivers22.
The analysis also shows that most of the elderly are still independent in carrying out daily activities in the form of BADL and IADL. The interview results also showed that some elderly do their hobbies, such as reading, gardening, sewing, and singing. They also carry out social activities such as recitation, social gatherings, and association, as well as operate their cellphone.
The high burden of care and chronic diseases suffered by the elderly must be a common concern because it negatively affects the quality of life and the family itself. Furthermore, the care burden for caregivers is related to family functions, such as social and emotional communication between members, thus, affecting the quality of life23. The burden of caregivers is a response to physical, mental, emotional, social, and financial stressors associated with providing care to members with chronic illnesses. Early detection of risk factors and the provision of health education and training on how to care for the elderly at risk of dementia are important.
Providing education and interaction in support groups can reduce the burden of caring for dementia patients24. These results are also supported by a study's report that health status, knowledge, care satisfaction, and social support from family are factors that play a major role in reducing the care burden11,12. Social and formal support can alleviate the caregiving burden, hence, coping skills become effective for increasing psychological resilience25. This is in line with the opinion of 26, which states that knowledge and understanding can raise awareness in a person and change behavior.
This condition causes the elderly at risk of dementia to require special attention and care from families and health care providers. The support of health workers is very important for sufferers and their families, especially in terms of providing information. This is because health education can improve health status, prevent additional problems, maintain existing status, maximize the functions and roles of clients during illness, and help clients and families overcome problems26,27. Unique sources of cognition are knowledge, awareness, understanding, or specific information about anything acquired from education and experience16)(28)(29)(30.
CONCLUSIONS
Families with elderly at risk of dementia have a low care burden because they are able to continue their daily lives independently and actively participate in social and religious activities. It is hoped that the family will continue to carry out regular checks related to chronic diseases and early detection of dementia to avoid increased symptoms. Similarly, families are expected to maintain physical and emotional conditions through support group activities such as health education.
REFERENCES
1. BAPPENAS. Proyeksi Penduduk Indonesia (Indonesia Population Projection) 2010 - 2035. Jakarta: Badan Pusat Statistik. 2013. [ Links ]
2. Miller CA. Nursing for wellness in older adult: theory and practice. 4th Edition. Philadelphia: Lippincot. 2014. [ Links ]
3. Ong P.A., Muis A., Rambe A.S., Widjojo S., Laksmidewi P., Pramono A., et al. Panduan Praktik Klinik. Diagnosis dan Penatalaksanaan Demensia. Jakarta: PERDOSSI. 2015. [ Links ]
4. Nasrun M.W.S., Aries W., Keliat B.A., Abikusno R.M.N., Harimurti K. Dasar-dasar Perawatan Demensia. Jakarta: PADI. 2017. [ Links ]
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder (DSM-5). (5th Ed). American Psychiatric Publishing. 2013. [ Links ]
6. Alzheimer's Disease International. World Alzheimer Report 2015. The global impact of dementia an analysis of prevalence, incidence, cost and trends. London: ADI. 2015. [ Links ]
7. Kemenkes. Strategi Nasional Penanggulangan Penyakit Alzheimer dan Demensia lainnya: Menuju Lanjut Usia Sehat dan Produktif. Jakarta. 2015. [ Links ]
8. Fitriani E.T., Hamid A.Y.S., Eka Putri Y.S. Studi fenomenologi stres dan strategi koping keluarga yang merawat lanjut usia dengan demensia di kota Tulungagung. Tesis. Diakses dari http://lib.ui.ac.id/detail?id=20349913&lokasi=lokal. 2013. [ Links ]
9. Pradana A.H., Sahar J., Permatasari H. Dementia: How does spouse perceive it?. Enfermeria Clinica, 2021; 31(Supp 2): 516-519. [ Links ]
10. Casado B.L., Lee S.E., Hong M., Hong S. The experience of family caregivers of older Korean Americans with dementia symptoms. Clinical Gerontologist, 2015; 38: 32-48. DOI: 10.1080/07317115.2014.970316. [ Links ]
11. Sahar J., Courtney M., Edwards H. Improvement of family carer's knowledge, skills and attitudes in caring for older people following the implementation of a Family Carer's Training Program in the community in Indonesia. International Journal of Nursing Practice, 2003; 9. doi: 10.1046/j.1440-172X.2003.00428.x. [ Links ]
12. Maryam R.S., Rosidawati, Riasmini M., Suryati E.S. Beban keluarga merawat lansia dapat memicu tindakan kekerasan dan penelantaran terhadap lansia. Jurnal Keperawatan Indonesia, 2012; 15(3): 143-150. [ Links ]
13. Senturk S.G., Akyol S.G., Kucukguclu O. The Relationship between Caregiver Burden and Psychological Resilience in Caregivers of Individuals with Dementia. International Journal of Caring Sciences, 2018; 11(2), 1223. [ Links ]
14. Canevelli M., Valletta M., Toccacelli B., Remoli G., Sarti G., Nuti F., et al. Facing dementia during the COVID 19 outbreak. Journal of the American Geriatrics Society, 2020; 68(8): 1673-1676. doi: 10.1111/jgs.16644. [ Links ]
15. Cohen G., Russo M. J., Campos J. A., Allegri R. F. Living with dementia: Increased level of caregiver stress in times of COVID-19. International Psychogeriatrics, 2020; 1-5. doi:10.1017/S1041610220001593. [ Links ]
16. Friedman M.M., Bowden V.R., Jones E.G. Family Nursing: Research, Theory and Practice. (5th ed). Upper Saddle River: Prentice Hall. 2003. [ Links ]
17. Wammes J.D., Labrie N.H.M., Agogo G.O., Monin J.K., deBekker-Grob, E.W., & MacNeil, V. Persons with dementia and informal caregivers prioritizing care: A mixed-methods study. Alzheimer's Dement, 2021; 7:e12193. https://doi.org/10.1002/trc2.12193. [ Links ]
18. Vitaliano P.P., Young H.M., Russo J. Burden: A Review of Measures Used Among Caregivers of Individuals with Dementia. The Gerontologist, 1991;31(1): 67-75. [ Links ]
19. Maryam R.S., Sahar J. Determining factors of dementia in elderly individuals residing in the special capital region of Jakarta. Enferm Clin, 2019; 29 (S2): 594-599. [ Links ]
20. Doblhammer G, Fink A, Fritze T, Günster C. The demography and epidemiology of dementia. Geriatric Mental Health Care 1, 2013: 29-33. [ Links ]
21. Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA, Kuslansky G, et al. Leisure activities and the risk of dementia in the elderly. The New England Journal of Medicine. 2003; 348:2508-16. [ Links ]
22. Lund C.L., Leino-Kilpi H., Bleijlevens M.H.C., Witten A.S., Martin M.S., Nilsson K., et al. Predicting caregiver burden in informal caregivers caring for persons with dementia living at home - A follow-up cohort study. Dementia, 2020; 19(3): 640-660. DOI: 10.1177/1471301218782502. [ Links ]
23. Ghasemi M., Arab M., Shahrbabaki P.V. Relationship Between Caregiver Burden and Family Functioning in Family Caregivers of Older Adults With Heart Failure. Journal of Gerontological Nursing, 2020, 46(6): 25-33. [ Links ]
24. Demir G., Platin N. Impact of Neuman Systems Model in Reducing Care Burden Primary Caregivers of Patients with Dementia. International Journal of Caring Sciences, 2017, 10 (1): 393. [ Links ]
25. Senturk S.G., Akyol S.G., Kucukguclu O. The Relationship between Caregiver Burden and Psychological Resilience in Caregivers of Individuals with Dementia. International Journal of Caring Sciences, 2018; 11(2): 1223. [ Links ]
26. Notoatmodjo, S. Promosi Kesehatan dan Perilaku Kesehatan. Edisi Revisi. Jakarta: Penerbit PT Rineka Cipta. 2012. [ Links ]
27. Wang Y, Xiao LD, He GP. A comprehensive approach to psychometric assessment of instruments used in dementia educational interventions for health professional: a cross-sectioal study. International Journal of Nursing Studies, 2015; 52: 568-577. [ Links ]
28. Lueckenotte A.G. Gerontologic Nursing. (3rd ed). St. Louis: Mosby Elsevier. 2003. [ Links ]
29. Pramujiwati D., Keliat B.A., Wardani I.Y. (2013). Pemberdayaan keluarga dan kader kesehatan jiwa dalam penanganan pasien harga diri rendah kronik dengan pendekatan model Precede L. Green di RW 06, 07 dan 10 Tanah Baru Bogor Utara Jurnal Keperawatan Jiwa, 2013, 1(2): 170-177. [ Links ]
30. Rustina Y., Nursasi A.Y., Budiati T., Syahreni E., Fitriyani P. Pengaruh Pemberdayaan Keluarga terhadap Status Kesehatan Bayi Berat Lahir Rendah di Kota Jakarta. Makara J. Health Res, 2014; 18(1): 19-24. doi: 10.7454/msk.v18i1.3089. [ Links ]
Received: September 03, 2022; Accepted: October 01, 2022











 text in
text in