My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.23 n.73 Murcia Jan. 2024 Epub Feb 23, 2024
https://dx.doi.org/10.6018/eglobal.579041
Originals
Implementation of Evidenced- Based Nursing in Primary Care
1Family and Community Nursing, Murcia Health Service. Murcia, Spain
Introduction:
The implementation of Evidenced- Based Nursing (EBN) is characterized by multiple benefits, for the patients and the nurses. However, the implementation is difficult for different reasons.
Objectives:
To evaluate the daily use of the EBN, the attitude towards EBN and the skills and knowledge of nurses to apply EBN in the selected health centers and also, to explore the self-perceived factors that may hinder the implementation of EBN at work and the possible measures to improve it by the nurses that work in PC.
Methods:
Cross-sectional, descriptive, multicenter and mixed concurrent triangulation strategy research, compose of a validated questionnaire and two open questions.
Results:
65 nurses participated, mostly women, of whom 50,8% have received EBN’s formation. The punctuation of the different parts of the questionnaire are: 27,02 (x̄) in the EBN’s daily use, 18 (m) in the attitude and 44,15 (x̄) in the EBN’s skills and knowledge. Some factors self-perceived that difficult the EBN’s implementation are the lack of formation and time and the job insecurity and there are some measures suggested for palliate it such as: formation, recruitment and teamwork.
Conclusions:
The participants show a favorable attitude towards EBN, but daily use and skills and knowledge are moderate, observing a relationship between training in EBN and nursing specialization with greater skills and knowledge in EBN. There is a need to carry out studies with a greater impact for a more complete evaluation and implementation of the appropriate strategies.
Key words: Evidence-Based Nursing; Primary Care Nursing; Nursing Research; nursing; Nursing Methodology Research; Clinical Nursing Research
INTRODUCTION
Evidence-Based Nursing (EBN), according to several authors, can be considered as "the conscious, explicit and judicious application of the best available scientific evidence related to nursing knowledge to make decisions about patient care, taking into account their preferences and values, and incorporating professional experience in this decision making(1).
Globally, the use of EBN is essential to obtain better health outcomes, provide higher quality care, and promote patient’s safety (2). Within health services, nurses represent almost half of health professionals worldwide and, particularly in Primary Care (PC), they lead health promotion and disease prevention (3),(4).
Since PC is the first level of care, it’s essential to question daily practice and take advantage of the latest evidence to improve the quality of nursing care (3). The benefits provided by the EBN should not be ignored, since in addition to benefiting the user, at the same time health spending is reduced, thanks to more efficient decision-making. The consideration of most health professionals of the importance of EBN motivates its implementation, while favoring job satisfaction and teamwork (3)-(5).
In previous research about this theme, the nurses, in general favorably perceive EBN, highlighting certain advantages such as the reduction of clinical variability and the empowerment of the profession (6). However, its implementation is slow and they perceive barriers to achieve it (7), such as lack of time, skills or insufficient authority to change protocols, as well as the predominance of the experience criteria among coworkers(8) (9) (10) (11).
In others studies, some barriers were identified, such as lack of formation in terms of researching, tiredness from have to keep up to date and even the rejection of change by the coworkers and, sometimes, by users and their families (11),(12). The origin of this lacks of formation could be, in part, because of the previous study plan, where until recently, research skills were absent in the formative program. With the transition from Diploma to Degree, this subject has been included, although in the background, because the low formation both at the undergraduate and postgraduate (13), level stands out, being the undergraduate stage the most important to internalize critical thinking skills, before the work stage(14).
The health care provided by nurses specialized in Family and Community Nursing increases the quality standards, due to the formative program received for two years, specialized, and based on scientific evidence. This formation also increases the professional autonomy of the nurses. The future of this specialization is destined for “give more and better answers of excellence to the community on what to do to maintain and increase their health”(15),(16).
In summary, in the similar studies consulted to the one that we propone, both nationally and internationally, it’s shown that, despite the fact that the nurses recognize the benefits of EBN and their attitude is positive, knowledge and the application in daily practice are relatively low and many of them don’t fell competent to apply it (3),(8). In order to overcome this handicap, the experts point out that the most important strategies are the presence of an optimal organization culture and attitude of managers, personal motivation, have enough time and the formation of nurses (14).
The reason why we have realized this study in PC lies in the importance of this level of care, being the first contact with the health system and leading, among other processes, health promotion and disease prevention. However, there’re different factors that could affect its implementation (11),(12). In addition, there’s a few similar studies realized in Región de Murcia o at the national level. So, we see the need to deepen the subject in order to get closer to the reality of the implementation of scientific evidence by this group.
The purpose of this study is to know the current situation of PC nurses regarding the use of EBN, in addition to have a general vision of the strengths and weaknesses that can be covered. The current level of implementation of the EBN in the health centers in which the questionnaire will be passed will be disclosed, in addition to the different barriers self-perceived by nurses, on which action could be taken to improve decision-making based on the scientific evidence. It could be also useful to facilitate and promote initiatives and thus improve daily clinical practice, in an autonomous and empowered way, thanks to EBN.
The objectives of this study are to evaluate the daily use of the EBN, the attitude towards EBN and the skills and knowledge of nurses to apply EBN in the selected health centers and also, to explore the self-perceived factors that may hinder the implementation of EBN at work and the possible measures to improve it by the nurses that work in PC.
MATERIAL AND METHOD
Study design and subjects
This study is mixed research (qualitative and quantitative) of concurrent triangulation study, through a cross-sectional, descriptive, and multicenter study, composed of a validated questionnaire and two open questions. The project was planned in January 2022, and the complete writing of the results of the study was finished in April 2023.
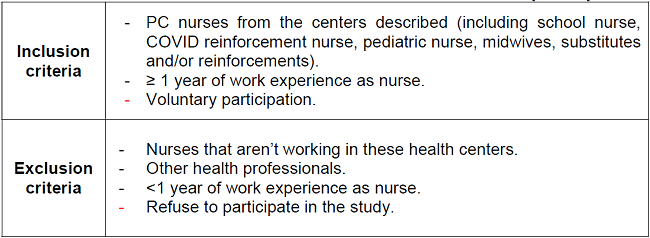
The participants are nurses that works in PC from various health centers of the Murcian Health Service: El Palmar, Santo Ángel, La Ñora, San Andrés, Alcantarilla-Sangonera, Sangonera la Verde, Espinardo and the peripherical centers from the Basic Health Zone of Murcia-La Ñora: Javalí Nuevo and Puebla de Soto. The selection of subjects that are part of the sample has been carried out by means of a non-probability sampling for convenience, inviting all nurses from each of the centers that were participating, considering the inclusion and exclusion criteria described in the table 1.
The sample universe is 85 people, covering the staff of PC nurses available in each health center selected, in addition to the substitutes and/or reinforcements, so we first passed the questionnaire to capture the largest number of participants possible, and then we did a reuptake to include those nurses that couldn’t participate the first time. The application of the questionnaire was carried out during the second quarter of the year 2022, offering its completion at first to capture the largest number of participants possible and we carried out a re-capture to include those nurses who couldn’t participate the first time. Finally, we have a sample size of 65 people, since there were 20 who refused to participate.
Data collection
This process has been carried out by completing a printed questionnaire that we have offered to each of the centers, prior notice to the Nursing managers, during working hours (8am-3pm), during the second quarter of 2022. We provide the questionnaires to Nursing managers and/or tutors, as well as to other Family and Community Nursing residents, collaborating in this task.
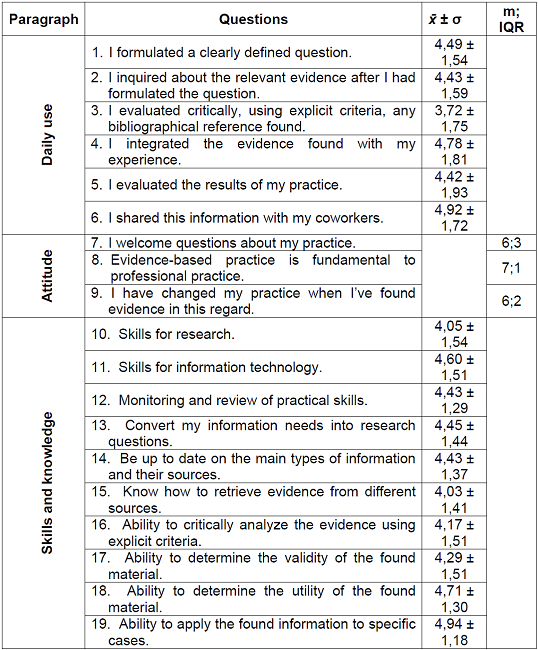
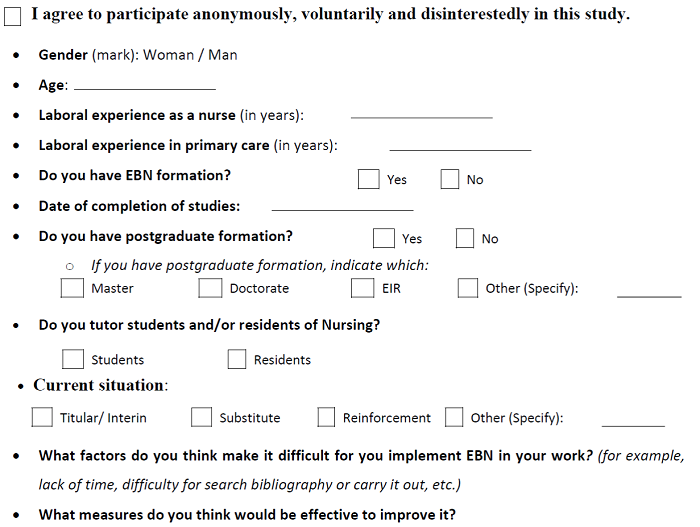
The questionnaire consists of three parts. To begin with, sociodemographic and labor variables have been collected. Secondly, a questionnaire in Spanish called the Clinical Effectiveness and Evidence-Based Practice Questionnaire (CPBE-19) validated in 2009 in the context of nursing practice has been used. This is self-administered and it’s composed by 19 questions distributed in three sections in relation to EBN: “daily practice”, “attitude" and "knowledge and skills”. These questions are scored on a Likert-type scale from 1 to 7, where 1 corresponds to the lowest degree of agreement (9). The time spent is approximately 10 minutes.
Finally, the participants answered two open questions to identify, on the one hand, the self-perceived factors that may hinder the implementation of EBN in PC and, on the other hand, the measures that could improve its use.
Study variables
Sociodemographic variables were collected: sex and age (in years) and professional variables: work experience as a nurse (in years), experience in PC as a nurse (in years), time elapsed since completion of studies (in years), previous formation in EBN, tutoring of nursing students and/or residents, postgraduate training and the current employment situation.
Statistic analysis
An analysis of the different variables has been carried out using the statistical program IBM SPSS Statistics version 27.0.1.0©, in addition to the qualitative content analysis through data coding, corresponding to the two open questions. The data haven’t been analyzed individually by health center in order to guarantee anonymity, especially in those health centers and clinics with fewer nurses and, therefore, fewer participants.
Ethical considerations
The participation in this study is completely voluntary and disinterested. The participants had the information about the study before answering the questionnaire, having to accept the informed consent previously. No data have been obtained that allow identification. The study has the permission of the Area 1- Murcia West Management (available in Annex I), and the permission of the Ethics Committee is not necessary given the characteristics of the study.
RESULTS
Statistical tests and sample’s description
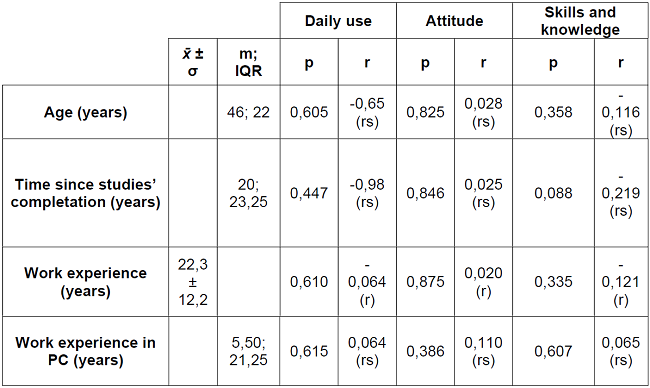
Firstly, the Kolmogorov-Smirnov normality test has been applied, obtaining as a result a parametric distribution for all the quantitative variables except for "PC experience" (p=0.01), the "time since completion of the studies” (p<0.001), age (p<0.001) and the “attitude” section of the applied questionnaire (p<0.01). Regarding descriptive statistics, we used the mean (x̄) and standard deviation (σ) for the parametric quantitative variables and the median (m) and interquartile range (IQR) for the non-parametric variables. Regarding the qualitative variables, we used the absolute frequency (n) and the percentage (%).
Next, after the different bivariate analyses, it is shown if there is a statistically significant association (p<0.05) between variables or not, using a 95% confidence interval. We have used the T-student statistical test to evaluate the association between parametric quantitative variables and dichotomous qualitative variables and the U-Mann Whitney in the case of non-parametric ones. We used ANOVA of one factor in the case of polytomous qualitative variables with a parametric quantitative variable and Kruskal-Wallis in the case of non-parametric ones.
Finally, we have realized correlation analysis for evaluate the association between quantitative variables and the validated questionnaire, using the Pearson’s correlation for parametric quantitative variables and the Spearman’s correlation for the non-parametric ones.
The number of participants we asked to fill out the questionnaire was 85, although only 65 completed at the end, with a response rate of 76.5%. The study sample is made up predominantly of women (84.6%) from nine health centers, with a median age of 47 years and the median number of years worked in PC is 5.5.
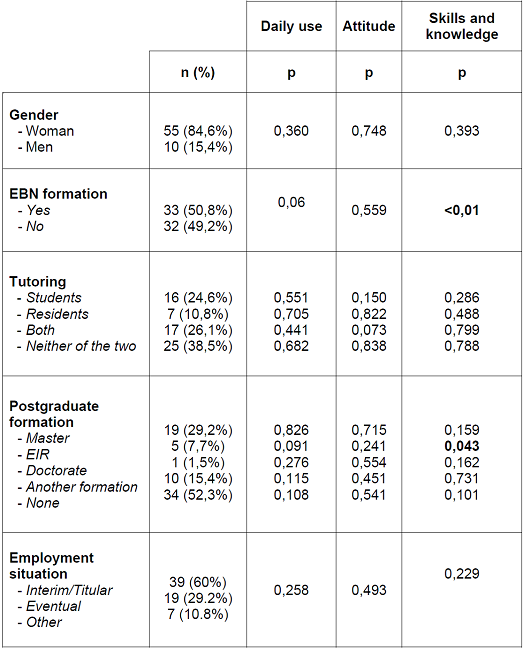
Of the total sample, approximately half (50.8%) have received EBN formation. Regarding postgraduate training, it is present in 47.7% of those surveyed. The most frequent is the master's degree (23.1%) and some of them have more than one type of postgraduate formation (6.15%). The rest of the variables are defined in the tables 3y4.
Daily use of EBN
The mean total score of EBN daily use is 27.02±8.25 points (out of a maximum of 42 points). The question with the highest score is sharing the evidence found with coworkers (x̄=4.92). The other way, the one with the lowest score is about the evaluation of the quality of the evidence (x̄=3.72). The rest of the questions have a similar average score, being in an intermediate position table 2).
Attitude towards EBN
The median of the total attitude score is 18 points (out of a maximum of 21 points) and the IQR is 4. The three questions in this section present high scores (between 6-7 points), in which they recognize the importance of incorporate evidence into professional practice. Likewise, they have a good predisposition to have their daily practice questioned by their coworkers and present a positive attitude towards change in the face of new evidence table 2).
Skills and knowledge to apply EBN
The average score is 44.15±11.39 points (out of a maximum of 70 points), reflecting a certain lack of knowledge and skills to apply the EBN. Of the questions presented, the one that received the lowest score was the one referring to the knowledge to collect scientific evidence from different sources (x̄= 4.03), also highlighting the issue related to research skills (x̄=4.05). As for the question with the highest score, this is in reference to the ability to apply the information found to specific cases (x̄=4.94) table 2).
After analyzing each section of the questionnaire, bivariate analysis were carried out (table 3), in which statistically significant differences are observed when relating EBN formation with EBN skills and knowledge (p<0.01).
With respect to gender, tutoring of students and/or residents, and employment status, no significant differences were found when relating it to any section of the questionnaire (p>0.05). Finally, in terms of postgraduate formation, there are significant differences in the case of EIR formation in respect to EBN skills and knowledge (p<0.05).
Finally, after the different correlation analysis (table 4), we haven’t obtained significant differences in any variable, so we cannot confirm any type of relationship.
Self-perceived factors that may hinder the implementation of the EBN and possible measures to improve it
We have carried out a descriptive analysis after coding the data of the two open questions that the participants had to complete. In this way, we have two categories: limiting factors when implementing the EBN and measures to improve its application. In turn, we’ve obtained others subcategories:
Limiting factors
- Labor conditions: The most repeated factor was the lack of time, reported by 47 people, some of whom related it to work overload and burnout. Another 4 people reported job insecurity, 1 person indicated a lack of physical space for nurses and, finally, 1 indicated a lack of financial resources.
- Formation: Regarding this subcategory, 29 people indicated a lack of formation in EBN and 2 people found it difficult to apply theory to practice, 1 of them considering that it’s due to lack of consensus on protocols.
- Individuals’ factors: There were 5 people who indicated a lack of willingness and interest on the part of their coworkers, of which 2 indicated an attitude of "negativity to change for convenience".
Measures
- Formation offer: Of the total number of subjects, 27 people demanded formation in EBN, of which 1 indicated that mandatory annual formation. On the other hand, 1 person indicated formation in handing new technologies.
- Management: The need to hire staff and/or reduce quotas was indicated by 13 people, of which 2 specified that the hiring could be focused on family and community specialist nurses and 5 people mentioned the offer of contracts to be able to cover the days for formation. Another measure mentioned by 8 people was the creation of a time slot during the working day to be able to search for evidence. In addition, 1 person indicated improving job stability, given the eventual hiring situation. Finally, 2 people indicated updating protocols to work systematically.
- Implication: To promote teamwork was one of the measures referred by 7 people, carrying out bibliographic searches and the subsequent sharing in a clinical session. 1 person indicated contact other PC professionals who are already implementing it, while another indicated carrying out a self-audit to assess deficiencies and share information with the entire team. Last, 2 people mentioned the need to raise awareness of the benefits of using EBN for better patient care and one of them indicates that this should be promoted from management.
DISCUSSION
In relation to the general objective of knowing the current implementation of EBN by nurses from different health centers in the Region of Murcia that have participated, the results obtained show a quite favorable attitude towards using the EBN, although the daily use and the knowledge and skills in EBN are still pending points to work on, following the trend of other studies carried out at the national level (2),(3).
Although we cannot establish relationships between a large number of variables, we did obtain significant differences with respect to having or not formation in EBN and a nursing specialism, since they favor the increase in skills and knowledge in EBN. In another similar study carried out in Spain, the same results were obtained for these two variables(3) and, despite the fact that having a nursing specialism improves EBN skills and knowledge, this is not reflected in daily use, and may be related to the organizational characteristics of the work. To do this, a study proposes that community nurse specialists adopt the role of EBN mentor nurses, leading the change towards an evidence-based organization (3).
Taking other studies as a reference, to increase the implementation of EBN by nurses, formative activities seem to be the most accessible intervention. However, there’re others such as the distribution of educational material from support (17) and the commitment on the part of managers to offer an adequate organizational culture that promotes EBN and motivates nurses to carry it out, since the characteristics of the environment seem to influence the incorporation of the best available evidence in daily practice (18). The creation of working groups can also be promoted, to facilitate the updating of knowledge according to the latest evidence (19). However, the EBN application will only be fully implemented when the nurses consider it useful for their daily practice (20).
Despite having a small sample size, certain trends can be observed in the relationship between variables that could be confirmed with a larger sample size, such as a possible inverse relationship between age and the time since the completion of studies with regarding the daily use of EBN.
Regarding the limitations of this study, these derive from non-probabilistic sampling, in addition to having a relatively small sample size, which could make it difficult to represent and extrapolate the results to the rest of the nurses who work in Primary Care in the Region. of Murcia. It is possible that the small sample size is related to not having obtained significant differences in many of the variables. Therefore, it would be ideal to continue deepening and carry out larger-scale studies in the Region of Murcia.
It is worth mentioning the non-response bias in the qualitative part of the study, since not all the participants answered the open questions, which makes it difficult to know if there are more limiting factors or measures that haven’t been mentioned in the rest of the answers.
Finally, as a proposal for improvement, an exhaustive evaluation of the perceived barriers and the detected needs could be carried out to program interventions that inspire community nurses in the use of EBN in their daily practice.
CONCLUSIONS
Participating nurses show a favorable attitude towards EBN, but daily use and skills and knowledge are moderate. There are various barriers that they perceive in relation to this topic, reiterating the lack of training, time and interest on the part of the professionals and some measures that they suggest to alleviate it are: formation, hiring of personnel and/or reduction of quotas and the development of teamwork. Regarding the rest of the variables, formation in EBN and nursing specialization are related to a higher level of skills and knowledge in EBN. Finally, we highlight the need to carry out studies with a greater impact in order to adequately assess the current state and needs and, thus, implement strategies that promote a change in PC in order to a nursing practice base on the last evidence.
REFERENCES
1. Alonso Coello P, Ezquerro Rodríguez O, Fargues García I, García Alamino JA, et al. Enfermería Basada en la Evidencia. Hacia la excelencia en los cuidados. Difusión Avances de Enfermería (DAE, S.L.), 2004: 10-23. Disponible en: https://ebevidencia.com/wp-content/uploads/2013/08/EBE.-Hacia-la-excelencia-en-cuidados.pdf [ Links ]
2. Ramos-Morcillo AJ, Fernández-Salazar S, Leal-Costa C, Ruzafa-Martínez M. Evidence-Based Practice nurses' competency: Spanish National Survey and establishment of a scale of the EBP-COQ-Prof(c). J Nurs Manag. 2020; 29: 794-804. Disponible en: https://onlinelibrary.wiley.com/doi/epdf/10.1111/jonm.13220?src=getftr [ Links ]
3. Fernández-Salazar S, Ramos-Morcillo AJ, Leal-Costa C, García-González J, Hernández-Méndez S y Ruzafa-Martínez M. Competencia en Práctica Basada en la Evidencia y factores asociados en las enfermeras de Atención Primaria en España. Aten Primaria, 2021; 53(7), 102050. Disponible en: https://www.sciencedirect.com/science/article/pii/S0212656721000846 [ Links ]
4. V. Jylhä, A. Oikarainen, M.-L. Perälä, A. Holopainen. Facilitating evidence-based practice in nursing and midwifery in the WHO European Region. World Health Organization, Copenhagen. 2017. Disponible en: https://www.euro.who.int/__data/assets/pdf_file/0017/348020/WH06_EBP_report_complete.pdf [ Links ]
5. Coster S, Watkins M, Norman I.J. What is the impact of professional nursing on patients' outcomes globally? An overview of research evidence. Int J Nurs Stud. 2018; 78: 76-83. Disponible en: https://pubmed.ncbi.nlm.nih.gov/29110907/ [ Links ]
6. Pericas-Beltran J, González-Torrente S, De Pedro-Gómez J, Morales-Asencio JM, Bennasar-Veny M. Percepción de las enfermeras españolas de Atención Primaria sobre la práctica clínica basada en la evidencia: un estudio cualitativo. Revista Int Nurs Rev. 2014; 61(1): 90-98. Disponible en: https://onlinelibrary.wiley.com/doi/10.1111/inr.12075 [ Links ]
7. Arechabala MC, Catoni MI, Rojas N, Rubio M, Carrasco P. Implementación de la práctica basada en evidencia en el currículo de Enfermería. Educ Med Super, 2018; 32(1). Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-21412018000100024&lng=es [ Links ]
8. Melnyk BM, Fineout-Overholt E, Fischbeck N, Li H, Small L, Wilcox L, Kraus R. Nurses' perceived knowledge, beliefs, skills, and needs regarding evidence-based practice: implications for accelerating the paradigm shift. Worldviews Evid Based Nurs. 2004; 1(3): 185-93. Disponible en: https://pubmed.ncbi.nlm.nih.gov/17163896/ [ Links ]
9. De Pedro GJ, Morales-Asencio JM, Sesé A, Bennasar M, Ruiz MJ, Muñoz F. Validación de la versión española del cuestionario sobre la Práctica Basada en la Evidencia en Enfermería. Rev Esp Salud Public. 2009; 83 (4): 577-586. Disponible en: https://scielo.isciii.es/pdf/resp/v83n4/original5.pdf [ Links ]
10. Ammatuna GP, Terrasa SA, Vazquez FR. Adaptación transcultural de un cuestionario para evaluar la autopercepción de la práctica clínica basada en la evidencia. Una experiencia con licenciadas en obstetricia. Evidencia, 2019; 22(3), e002028. Disponible en: https://www.evidencia.org.ar/index.php/Evidencia/article/view/4253 [ Links ]
11. Cidoncha-Moreno, M.A; Ruíz de Alegría-Fernández de Retana, B. Percepción de barreras para la utilización de la investigación en enfermeras de Osakidetza. Enfermería Clínica, 2017; 27(5): 286-293. Disponible en: https://www.elsevier.es/es-revista-enfermeria-clinica-35-articulo-percepcion-barreras-utilizacion-investigacion-enfermeras-S1130862117300463 [ Links ]
12. Sánchez-García I; López-Medina I.M.;Pancorbo-Hidalgo P. Obstáculos percibidos por las enfermeras para la práctica basada en evidencias: Un estudio cualitativo. Enfermería Clínica. 2013; 23(6): 279-283. Disponible en: https://www.elsevier.es/es-revista-enfermeria-clinica-35-articulo-obstaculos-percibidos-por-enfermeras-practica-S1130862113001332 [ Links ]
13. Solís Muñoz M. Competencias en práctica clínica basada en la evidencia en las enfermeras de España [Tesis doctoral]. Madrid: Universidad Complutense de Madrid; 2015. Disponible en: https://eprints.ucm.es/id/eprint/34374/1/T36690.pdf [ Links ]
14. Orellana Yañez A., Paravic Klijn T., Enfermería Basada en Evidencia: Barreras y estrategias para su implementación. Cienc. enferm. 2007; 13(1): 17-24. Disponible en: http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-95532007000100003&lng=es [ Links ]
15. Bennasar Veny M. La Especialidad de Enfermería Familiar y Comunitaria y la importancia de una formación basada en la evidencia. Evidentia. 2010; 7(31): 1. Disponible en: http://www.index-f.com/evidentia/n31/ev3111.php [ Links ]
16. Heierle Valero C. La especialidad de Enfermería Familiar y Comunitaria. Enferm Comun. 2009. 5 (2). Disponible en: http://www.index-f.com/comunitaria/v5n2/ec0052.php [ Links ]
17. Forsetlund L, O'Brien M.A., Forsén L, Mwai L, Reinar LM, Okwen MP, et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009 (2); CD003030. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7138253/pdf/CD003030.pdf [ Links ]
18. Gómez J.P, Morales- Asencio J.M., Sesé A., Benassar M., Artigues G., Perelló C. Entorno de práctica de los profesionales de enfermería y competencia para la incorporación de la evidencia a las decisiones: situación en las Islas Baleares. Gac. Sanit. 2011; 25 (3): 191-7. Disponible en: https://www.sciencedirect.com/science/article/pii/S0213911110003250 [ Links ]
19. Orellana Yañez A, Paravic Klijn T. Enfermería basada en evidencia: Barreras y estrategias para su implementación. Cienc. enferm. 2007; 13(1): 17-24. Disponible en: http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-95532007000100003&lng=es [ Links ]
20. Mathieson A, Grande G, Luker K. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: a systematic mixed-studies review and qualitative synthesis. Prim Health Care Res Dev. 2019;20(6). Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6476399/ [ Links ]
ANNEX 1.
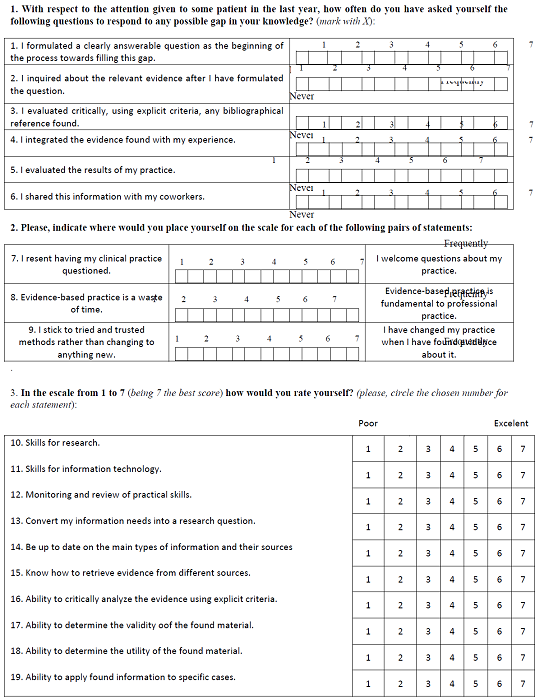
Clinical Effectiveness and Evidence-Based Practice Questionnaire (CPBE-19).Next, we have the questionnaire, which is designed to collect information and opinions about the use of evidence-based practice among health professionals. There are not correct or incorrect answers, we are only interested on your opinions and the use of evidence in your practice.
Received: July 23, 2023; Accepted: August 12, 2023











 text in
text in