My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.23 n.73 Murcia Jan. 2024 Epub Feb 23, 2024
https://dx.doi.org/10.6018/eglobal.561191
Originals
Content validity of the nursing diagnosis proposal ocular dryness in adult patients admitted to the intensive care unit
1University of the State of Rio Grande do Norte. Caicó. Brazil
2Federal University of Rio Grande do Norte. Native. Brazil
3Faculty of Nursing and Medicine Nova Esperança. Mossoro, Brazil
Objective:
to verify the content validity of the nursing diagnosis proposal Ocular dryness in adult patients admitted to an intensive care unit.
Materials and methods:
this is a methodological study of content validation of the nursing diagnosis proposal Ocular dryness, operationalized through a focus group. The selection of specialists took into account the clinical and/or academic experience in the area of nursing diagnoses and/or ocular dryness and/or dry eye and/or ocular health, as well as the time of performance with the theme. Thirteen nurses who met the criteria described above were invited, of whom 10 agreed to participate. The validation approach was by consensus. Data were analyzed using descriptive statistics, level of expertise and analysis of diagnostic elements.
Results:
after the final consensus of the nurse judges in relation to the diagnostic elements, a proposal of the diagnosis Ocular dryness was defined based on the validity of content with a new definition, 14 defining characteristics, 9 related factors, 2 populations at risk and 20 associated conditions. In addition, after judging the coherence of the elements in relation to the diagnostic structure, the judges issued the consensus in relation to the conceptual and operational definitions.
Conclusions:
the study allowed verifying the validity of the content by judges of the nursing diagnosis proposal Ocular dryness in patients in intensive care units, which favors the diagnostic reasoning of nurses and the planning of effective interventions related to this diagnosis, allowing the management of the patients in order to provide ocular integrity.
Keywords: Nursing Diagnosis; Validation Studies; Dryness; Eye Health; Intensive Care Units
INTRODUCTION
Critical patients are at greater risk for the development of changes in the ocular surface(1). Ocular dryness, in turn, presents itself as an undesirable human response characterized by inadequate secretion or lacrimal evaporation of the eye(2). Studies describe that the incidence of dry eye in patients admitted to the Intensive Care Unit (ICU) ranges from 53.0% to 75.3%(3,4). The risk of progression of this condition is highlighted, since it can progress to vision los(3,4,5).
Considering the possible damages, the nursing team should implement strategies for early identification of human responses that indicate the presence of ocular dryness. The timely identification of this condition allows the development of appropriate interventions to promote ocular integrity, in order to designate targeted measures for prevention, obtaining better results in patients’ care(6,7).
Related to the diagnostic focus of this proposal, the NANDA-International taxonomy (NANDA-I) establishes the nursing diagnoses (ND) Risk of ocular dryness (00219) and Ineffective self-management of ocular dryness (00277)(8). However, it is understood the need to use the term Ocular dryness as an undesirable human response, permeated by an early stage of tear film dysfunction, and not only as a state of risk or ineffective self-management.
Notably to this human response, nurses have the ability to assess their presence, severity and implement specific interventions aimed at preventing Ocular dryness through the use of their classification systems(7,8). Therefore, the importance of conducting this research as a modification of this state of risk/self-management for a diagnosis focused on the problem is justified. Thus, from the identification of Ocular dryness as an undesirable human response, a new diagnostic proposal was suggested in previous research, noting the need to validate Ocular dryness as a diagnosis focused on the problem(9).
Given the above, the present study aimed to verify the content validity of the nursing diagnosis proposal Ocular dryness in adult patients admitted to an intensive care unit.
MATERIALS AND METHODS
This is a methodological study of content validation of the nursing diagnosis proposal Ocular dryness. The adopted reference addresses the validation of nursing diagnoses based on three stages: concept analysis, content analysis by judges and analysis of the accuracy of clinical indicators(10). In the study in question, the content analysis stage was developed.
This stage was carried out by judges in order to discuss and judge which elements identified represent the diagnosis and which should be eliminated or revised (defining characteristics, related factors, population at risk and associated conditions), as well as the attributes and conceptual and operational definitions built. Thus, it is proposed to improve the diagnostic structure based on the judgment of nurse judges.
The model called “Collective Wisdom” was used, in which the collective knowledge of a group of experts presents a better estimate than the opinion of a single expert(10). The validation process regarding the content was carried out through a focus group, because Ocular dryness is a recent term with still limited discussion in the nursing area. The selection of specialists took into account the clinical and/or academic experience in the area of nursing diagnoses and/or Ocular dryness and/or dry eye and/or ocular health, as well as the time of performance with the theme.
Thirteen nurses who met the criteria described above were invited, of whom 10 agreed to participate. Each selected specialist received an invitation letter by e-mail with explanations about the purposes of the study and the methods adopted. For those who expressed interest in participating in the study, the Informed Consent Form and the data collection instrument were sent.
Thus, the diagnostic product built from a concept analysis carried out in a previous study(9), was discussed by a focus group composed of 10 specialist nurses members of the Center for Studies in Nursing Process and Classifications of the Federal University of Rio Grande do Norte (NEPEC/UFRN). The nurse judges discussed and judged the relevance of the diagnostic elements, attributes and conceptual and operational definitions constructed for the clinical indicators of the diagnosis. The analysis took place in November 2018, through three face-to-face meetings lasting 4 hours each. A characterization instrument was applied containing items related to sociodemographic data, academic degree, current occupation, time of professional training, experience with research in the area of nursing diagnoses and/or ocular dryness and/or dry eye and/or ocular health, professional activity, practical experience and teaching among the participants.
In addition, a presentation of the scenario in which Ocular dryness occurs in the present study and each of the diagnostic elements, as well as the attributes that made up the definition of the diagnosis and the conceptual and operational definitions constructed was made. The discourse emerging among the judges was transcribed and analyzed. The opinions of the judges were transcribed in the text immediately by the observer, read after exhaustive discussions and the final version of each element and definition was presented for approval or not.
When there were proposals to add new diagnostic elements or substantially modify the content of the definitions constructed, new searches in the literature were carried out in order to verify the relevance of the new information to be added. Finally, the analysis in relation to the adequacy of the domain and class in which the diagnosis could be added in NANDA-I was made.
The opinions expressed by each judge were considered. Thus, all questions and suggestions of the judges were discussed among the participants until consensus was reached. Consensus was considered when all participants in the group agreed with the synthesis of the discussion about each question or suggestion, carried out by the responsible researcher. Thus, the validation approach was by consensus.
For the descriptive analysis of the participants' characterization, the frequencies, measures of the distribution center and their variability were considered. The Shapiro-Wilk test was applied to verify the normality of the data.
The classification of the experts' expertise was defined as: novice, advanced beginner, competent, proficient and expert. The level of expertise was given by calculating the arithmetic mean of the scores obtained in the following criteria: time of training, practical experience and academic degree, participation in research projects that included the topic addressed and publication of scientific papers in that area(11).
For the analysis of the diagnostic elements, conceptual and operational definitions, domain and class, the opinions expressed by each judge were considered. However, the group consensus was used for the final judgment, which means that during the discussion each participant expressed their opinion on the items and the decision on inclusion, elimination or reformulation was made based on the group consensus.
This study was approved by the Research Ethics Committee of the Federal University of Rio Grande do Norte under opinion 918.510 and CAAE 36079814.6.0000.5537. The participation of nurse judges was consolidated after signing the Informed Consent Form and the Authorization Term for Voice Use.
RESULTS
The sample of 10 nurse judges was predominantly female (90.0%). The master's degree prevailed (50.0%), most had professional experience in care, teaching and research (60.0%) and had didactic experience in teaching nursing diagnoses (90.0%). All participants had experience in participating in research projects involving nursing diagnoses and ocular dryness/dry eye/ocular health.
Related to the publication of scientific papers, all had publications in the area of nursing diagnosis (100.0%) and in the theme of Ocular dryness/dry eye/ocular health (80.0%). Concerning the level of expertise, 03 specialists (30.0%) were advanced beginners, 03 (30.0%) competent, 02 (20.0%) proficient, 01 (10.0%) novice and 01 (10.0%) expert.
The participants' age averaged 28.8 years (±4.8), the length of training a median of 3.5 years and the length of participation in research groups focusing on the theme of nursing terminologies averaged 4 years (±1.8 years).
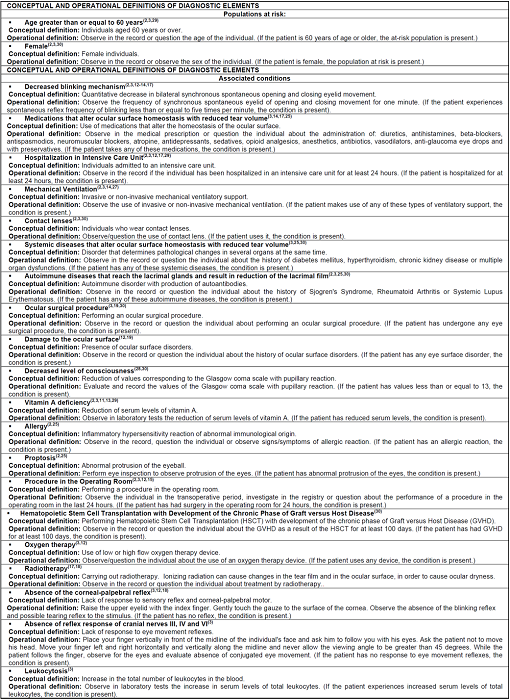
Regarding the definition of the diagnosis, there was a change from “Quantitative tear film deficiency, which can alter the maintenance of the integrity of the ocular surface, associated with the presence of clinical signs and/or symptoms with potential harm to ocular health” to “Quantitative tear film insufficiency, which can compromise the maintenance of the integrity of the ocular surface”.
Regarding the defining characteristics, the division between signs and symptoms was accepted by the judges, six were modified in relation to the title in order to make them more intelligible, namely: “Decreased tear volumetry” reformulated to “Decreased tear volume”; “Mucosal secretion/excess of ciliary crusts” to “Excessive mucoid secretion”; “Mucosal plaques” to “Mucoid plaque”; “Foreign body sensation” to “Ocular foreign body sensation”; “Burning” to “Burning eye sensation”; “Pruritus” to “Pruritus sensation in the eye”. Two defining characteristics were included, namely: “sandy sensation in the eye” and “Ocular dryness sensation”. There was no suggestion of exclusion and the others remained as described in the initial proposal after concept analysis.
Regarding the related factors, the division between individual and environmental factors was considered by the judges. Thus, regarding the factors related to the individuals, six had their titles rephrased for a better description and, of these, four were transferred to associated conditions since we understand that they are not independently modifiable by nurses, namely: “Incomplete eyelid closure (lagophthalmia)” was changed to “Lagophthalmia”; “Decreased blinking mechanism” to “Decrease in the blinking mechanism” (transferred to associated conditions); “Exposure to screens” to “Exposure to digital screens”; “Exophthalmia” to “Proptosis” (transferred to associated conditions); “Impaired corneal reflex” to “Absence of corneal-palpebral reflex” (transferred to associated conditions); and “Absence of reflex response of cranial nerves III, III and VI” to “Absence of response to reflexes of cranial nerve pairs III, IV and VI”(transferred to associated conditions). On environmental factors, “Excessive wind” was reworded to “Excessive air current”. No related factors were excluded and the others remained as they were written in the initial proposal.
Regarding the populations at risk, six had their titles reformulated and, of these, five were transferred to associated conditions, taking into account that they are medical procedures/treatments that are not independently modifiable by the nurses. They are: “Advanced age” to “Age greater than or equal to 60 years”; “Hospitalized in the Intensive Care Unit” to “Hospitalization in the Intensive Care Unit” (transferred to associated conditions); “Contact lens wearers” to “Contact lens” (transferred to associated conditions); “Subjected to procedures in the Surgical Center” to “Procedure in the Surgical Center” (transferred to associated conditions); “Submitted to Hematopoietic Stem Cell Transplantation” to “Hematopoietic Stem Cell Transplantation with development of the chronic phase of Graft versus Host Disease” (transferred to associated conditions); “Submitted to Radiotherapy” to “Radiotherapy” (transferred to associated conditions). There was no population at risk excluded and only one (female) remained described according to the initial proposal.
Regarding the associated conditions, seven had their titles reformulated, becoming: “Medications that alter ocular surface homeostasis” to “Medications that alter ocular surface homeostasis with reduction of tear volume”; “Systemic changes (Diabetes Mellitus, Hypertension, Hyperthyroidism, Chronic Renal Insufficiency, Multiple organ failure)” to “Systemic diseases that change ocular surface homeostasis with reduction of tear volume”; “Autoimmune diseases (Sjogren's syndrome, rheumatoid arthritis, systemic lupus erythematosus)” to “Autoimmune diseases that reach the lacrimal glands and result in reduction of lacrimal film”; “Ocular surgical procedures (Refractive surgery, cataract surgery, blepharteroplasty)” to “Ocular surgical procedure”; ““Decreased Glasgow Coma Scale Score/Reduced Level of Consciousness” to “Decreased level of consciousness”; “Ill-fitting non-invasive mechanical ventilation masks” to “Ill-fitting non-invasive mechanical ventilation or oxygen therapy device” (moved to related factors); “Change in leukocytes” to “Leukocytosis”.
An associated condition was transferred to factors related to the understanding of being able to be independently modified by nurses and one (sedation) was excluded because it was already contemplated in another item (drugs that alter the homeostasis of the ocular surface with reduction of tear volume). The other conditions remained with the presentation according to the initial proposal.
In addition, after discussions in the focus group, the proposed diagnosis remained an integral part of domain 11, Safety/protection, and Class 2, Physical injury, estimated as adequate when taking into account the definitions of the domains and classes described in NANDA-I.
After the final consensus of the nurse judges as to the diagnostic elements, a proposal of the diagnosis Ocular dryness was defined based on the validity of the content with the new definition, 14 defining characteristics, 9 related factors, 2 populations at risk, and 20 associated conditions, as shown in Table 1.
Table 1. Proposition of the structure of the nursing diagnosis Ocular dryness based on content validity. Natal, RN, Brazil, 2019.
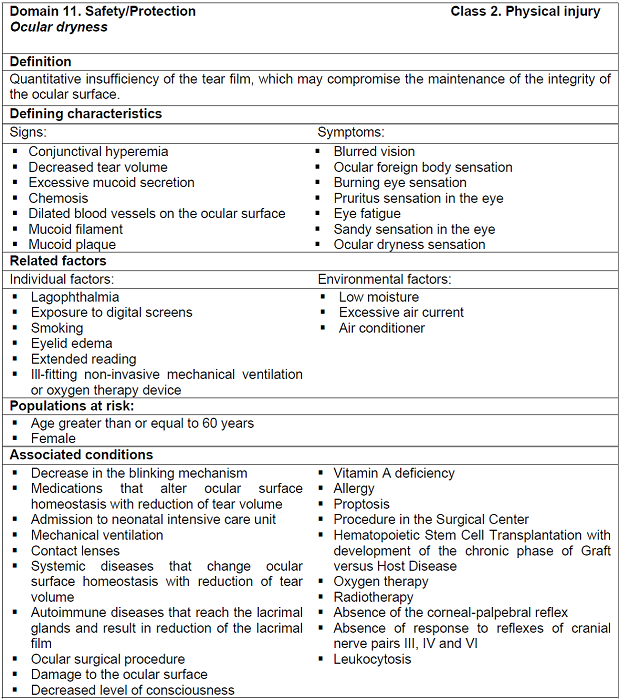
After judging the coherence of the elements in relation to the diagnostic structure, the judges issued the consensus in relation to the conceptual and operational definitions. It is noteworthy that all have undergone reformulations in order to become simpler, clearer, express a single idea and allow differentiation between the other elements of the diagnosis. The new descriptions of the definitions related to the defining characteristics are presented in Table 2.
Table 2. Conceptual and operational definitions of the defining characteristics of the nursing diagnosis Ocular dryness based on content validity. Natal, RN, Brazil, 2019.(2),(3),(4),(10),(12),(15),(16),(17),(18),(19),(20),(21),(22),(23),(24),(25),(26)
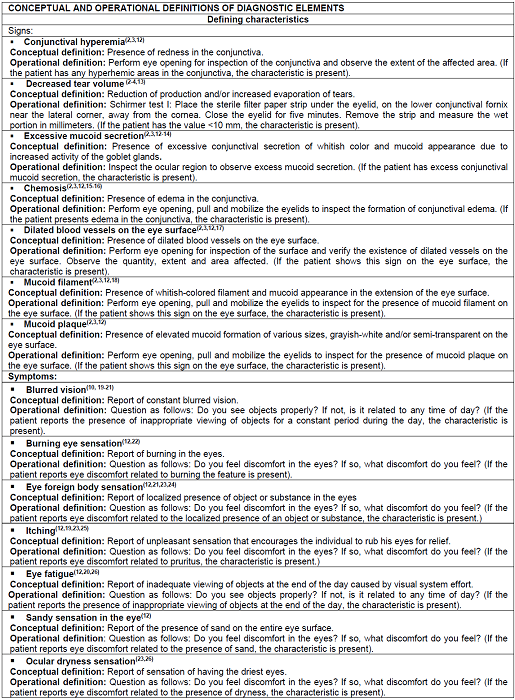
The new conceptual and operational definitions regarding the related factors of the nursing diagnosis proposal Ocular dryness were validated by the judges, as shown in Table 3 below.
Table 3. Conceptual and operational definitions of the related factors of the nursing diagnosis Ocular dryness based on content validity. Natal, RN, Brazil, 2019.(2),(3),(7),(12),(19),(27),(28),(14),(29),(30)
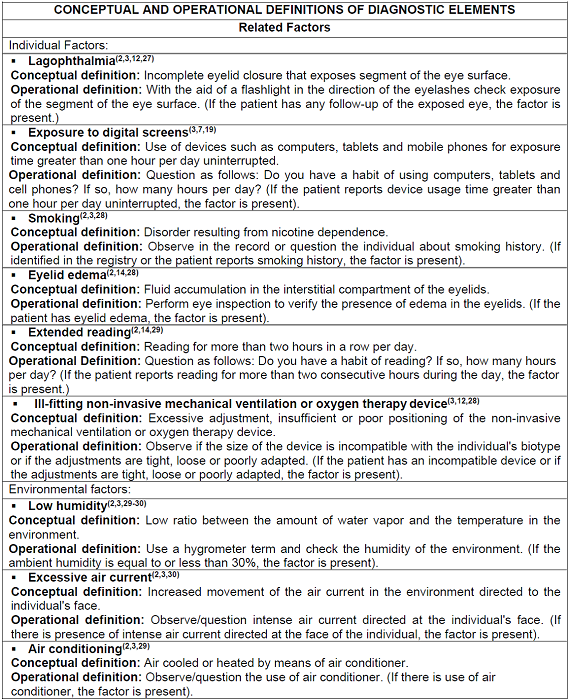
In addition, the new conceptual and operational definitions regarding the populations at risk and the associated conditions of the nursing diagnosis proposal Ocular dryness were validated by the specialists, as shown in Table 4 below.
DISCUSSION
In the process of validation of the diagnostic content, it is essential to have the opinion of specialists in the thematic area of research. However, there is some difficulty in obtaining specialists to validate nursing diagnoses in practice. In this sense, the stage of content analysis by specialists was operationalized through the focus group.
Regarding the characterization of the participants, it was observed that most were female, with a master's degree, had professional experience in care, teaching and research and had didactic experience in teaching nursing diagnoses. In addition, most of the judges had experience in participating in projects/publishing research involving nursing diagnoses and ocular dryness/dry eye/ocular health. These characteristics allow the understanding that the participants had an appropriate knowledge to ensure an in-depth discussion about the concept studied.
The classification of the level of expertise that stood out were the advanced beginner levels and the competent ones. In this study, only one specialist was classified in the last level of expertise, being the expert. However, this does not interfere with the results of this study, since the model adopted was that of “collective wisdom”, which ensures that the opinions of many people with different levels of expertise tend to present better accuracy in inferences when compared to all separate individual assumptions or even the isolated assumptions of experts(10).
In addition, the evaluation of the elements of the nursing diagnosis proposal Ocular dryness becomes relevant, since it is essential to review the elements of the diagnoses that allow the nurses to accurately identify the ND, so that it can intervene effectively in the health care of individuals(8). The definition of the diagnosis suggested in this study was validated by the judges as “Quantitative tear film insufficiency, which can compromise the maintenance of the integrity of the ocular surface”. The proposed change was based on the discussion that patients diagnosed with ocular dryness may be in an initial state of tear film insufficiency such that they may or may not present clinical signs and/or symptoms.
The judges agreed with the domain and class of insertion of the nursing diagnosis in NANDA-I, which remained as a member of domain 11, Safety/protection, defined as being free from danger; physical injury or damage to the immune system; conservation against losses; and protection of safety and the absence of danger; and in Class 2, Physical injury, characterized as damage or injury to the body(8).
The analysis performed by the judges showed that 14 defining characteristics were expressive for the conceptual core, therefore, belonging to the diagnosis of the study. The judges judged it relevant to include the defining characteristics “Sandy sensation in the eye” and “Ocular dryness sensation” for the inference of Ocular dryness. Corroborating this fact, the literature points out the two defining characteristics included as recurrent symptoms in ocular dryness(30).
Among the related factors, the judges consider nine relevant factors, which were allocated between individual factors and environmental factors. Noting the opinion of the judges, studies point to lagophthalmia as the main ocular alteration identified and an important determining factor for the development of ophthalmic damage(5). Other factors such as exposure to digital screens, smoking and eyelid edema are cited in the literature as factors that strongly influence the appearance of ocular dryness(19,28).
With regard to populations at risk, studies point to aging as a state that comprises the loss of androgens and results in alteration in the main lacrimal gland. In relation to the female sex, women have lower production of androgens in relation to men, allowing the impairment of the function of the lacrimal glands(29,30). In this understanding, the judges considered age greater than or equal to 60 years and female sex as populations with higher risk of presenting ocular dryness.
According to the judges' analysis, 20 associated conditions proposed, which are not independently modifiable by the nurses, were considered relevant to substantiate the diagnostic inference. Admission to the Intensive Care Unit, systemic diseases that alter the homeostasis of the ocular surface with reduction of tear volume and medications that alter the homeostasis of the ocular surface with reduction of tear volume are associated conditions commonly identified in ocular dryness(9).
All aspects related to medical diagnoses, medications in use, procedures and devices that cause reduction of tear volume, identified in a previous study(9), were analyzed by the judges as valid in relation to the associated conditions of the diagnosis under study.
Thus, the judges consented to the coherence of the elements in relation to the diagnostic structure and made the conceptual and operational definitions simpler and clearer in order to express a single idea and allow differentiation between the other elements of the diagnosis.
Understanding the conceptual and operational aspects of the elements of ocular dryness makes it possible to identify them more explicitly in the face of ocular manifestations. The operational definitions of each element provide instrumentalized subsidies for nurses, in a way that allows an evaluation directed towards the identification of the diagnosis(10).
This study presents as a limitation the fact that some nurses who participated in the study never used the nursing diagnosis Ocular dryness in their professional practice, either in research or care. However, most of the judges who participated in this study had clinical and/or academic experience in the area of nursing diagnoses and/or ocular dryness and/or dry eye and/or ocular health and contributed to the validation of the content of the diagnosis in question.
The present study contributed to validate with judges a new nursing diagnosis proposal that will be used for improvements in professional nursing practice in relation to an individual or population. This study also provides subsidies for the revision of the NANDA-I taxonomy in order to facilitate the identification of the nursing diagnosis Ocular dryness.
CONCLUSION
The study allowed the validation of the content by judges of the nursing diagnosis proposal Ocular dryness in patients in intensive care units with a new definition, 14 defining characteristics, nine related factors, two populations at risk and 20 associated conditions. The elements of the diagnosis in question were analyzed with a more coherent and clear structure for definition, defining characteristics, related factors, and populations at risk and associated conditions.
The validation of the content of the nursing diagnosis in question favors the nurses’ diagnostic reasoning and the planning of effective interventions related to this diagnosis, allowing the management of the patients in order to provide ocular integrity. In addition, this study allows giving consistency to the elements of the diagnosis and fills the gaps in the NANDA-I Taxonomy.
REFERENCIAS
1. Machado ASM, Cruz ICF. Risk of eye dryness in intensive care unit: systematic review of literature. J Nurs Care. 2019;11(1). Available from: http://www.jsncare.uff.br/index.php/jsncare/article/view/3131/791. [ Links ]
2. Dana R, Bradley JL, Guerin A, et al. Comorbidities and Prescribed Medications in Patients With or Without Dry Eye Disease: A Population-Based Study. Am J Ophthalmol. 2019;198:181-192. DOI: 10.1016/j.ajo.2018.10.001 [ Links ]
3. Araújo JNM, Botarelli FR, Fernandes APNL, et al. Predictive clinical factors for ocular dryness in patients admitted to the Intensive Care Unit. Rev Esc Enferm USP. 2019;53:e03493. DOI: 10.1590/S1980-220X2018036603493 [ Links ]
4. Araújo JNM, Fernandes APNL, Silva HP, et al. Risk of dry eye and ocular dryness in intensive care: a cross - sectional study. Online Braz J Nurs. 2018;17(2). DOI: 10.17665/1676-4285.20185937 [ Links ]
5. Golden MI, Meyer JJ, Patel BC. Dry Eye Syndrome. StatPearls. 2021. Available from: https://pubmed.ncbi.nlm.nih.gov/29262012/ [ Links ]
6. Plaszewska-Zywko L, Sega A, Bukowa A, Wojnar-Gruszka K, Podstawa M, Kózka M. Risk Factors of Eye Complications in Patients Treated in the Intensive Care Unit. Int J Environ Res Public Health. 2021;18(21):11178. DOI: 10.3390/ijerph182111178 [ Links ]
7. Pourghaffari Lahiji A, Gohari M, Mirzaei S, Nasiriani K. The effect of implementation of evidence-based eye care protocol for patients in the intensive care units on superficial eye disorders. BMC Ophthalmol. 2021;21:275. DOI: 10.1186/s12886-021-02034-x [ Links ]
8. Herdman TH, Kamitsuru S, Lopez CT. Diagnósticos de enfermagem da NANDA-I: Definições e classificação 2021-2023. 12 ed. Porto Alegre: Artmed; 2021. [ Links ]
9. Araújo JNM. Construção e validação do diagnóstico de enfermagem ressecamento ocular em pacientes adultos internados em unidade de terapia intensiva. Natal. Tese Doutorado em Enfermagem - Centro de Ciências da Saúde, Universidade Federal do Rio Grande do Norte; 2019. [ Links ]
10. Lopes MVO, Silva VM, Araújo TL. Métodos de pesquisa para validação clínica de conceitos diagnósticos. In: NANDA International, Inc.; Herdman TH, organizadora. PRONANDA. Porto Alegre: Artmed Panamericana, 2022. [ Links ]
11. Benner P, Tanner C, Chesla C. Expertise in nursing practice: caring, clinical judgment, and ethics. 2. ed. New York: Springer Publishing Comapny, 2009. [ Links ]
12. Fernandes APNL, Araújo JNM, Botarelli FR, et al. Dry Eye Syndrome in Intensive Care Units: a concept analysis. Rev Bras Enferm. 2018;71(3):1162-1169. DOI: 10.1590/0034-7167-2016-0582 [ Links ]
13. Koh S, Rao SK, Srinivas SP, Tong L, Young AL. Evaluation of ocular surface and tear function - A review of current approaches for dry eye. Indian J Ophthalmol. 2022 Jun;70(6):1883-1891. DOI: 10.4103/ijo.IJO_1804_21 [ Links ]
14. Walter K. What Is Dry Eye Disease? JAMA. 2022;328(1):84. DOI: 10.1001/jama.2022.5978 [ Links ]
15. Santos QF, Paes GO, Góes FGB. Alterações oculares em unidade de terapia intensiva: scoping review. Rev Recien. 2021; 11(34):168-180. DOI: 10.24276/rrecien2021.11.34.168-180 [ Links ]
16. Li T, Zhou H. Effect of Polyethylene Cover for Preventing Corneal Injury in Critically Ill Patients: A Meta-Analysis. Comput Math Methods Med. 2022;2022:6578229. DOI: 10.1155/2022/6578229 [ Links ]
17. Momeni Mehrjardi Z, Mirzaei S, Gohari M, Hafezieh A, Nasiriani K. Effect of Training Eye Care Clinical Guideline for ICU Patients on Clinical Competence of Eye Care in Nurses. Crit Care Res Pract. 2021;2021:6669538. DOI: 10.1155/2021/6669538 [ Links ]
18. Bird B, Dingley S, Stawicki SP, et al. Exposure Keratopathy in the Intensive Care Unit: Do Not Neglect the Unseen. Vignettes in Patient Safety. 2018;2. DOI: 10.5772/intechopen.72791 [ Links ]
19. Akpek EK, Amescua G, Farid M, et al. Dry Eye Syndrome Preferred Practice Pattern®. Ophthalmol. 2018;126(1):P286-P334. DOI: 10.1016/j.ophtha.2018.10.023 [ Links ]
20. Asbell PA, Maguire MG, Peskin E, et al. Dry Eye Assessment and Management (DREAM(c)) Study: Study design and baseline characteristics. Contemp Clin Trials. 2018;71:70-79. DOI: 10.1016/j.cct.2018.06.002 [ Links ]
21. Clayton JA. Dry Eye. N Engl J Med. 2018;379(11):e19. DOI: 10.1056/NEJMra1407936 [ Links ]
22. Olaniyan SI, Fasina O, Bekibele CO, et al. Dry eye disease in an adult population in South-West Nigeria. Cont Lens Anterior Eye. 2016;39(5):359-364. DOI: 10.1016/j.clae.2016.06.008 [ Links ]
23. Brissette AR, Drinkwater OJ, Bohm KJ, et al. The utility of a normal tear osmolarity test in patients presenting with dry eye disease like symptoms: A prospective analysis. Cont Lens Anterior Eye. 2019;42(2):185-189. DOI: 10.1016/j.clae.2018.09.002 [ Links ]
24. Kyei S, Dzasimatu SK, Asiedu K, et al. Association between dry eye symptoms and signs. J Curr Ophthalmol. 2018;30(4):321-325. DOI: 10.1016/j.joco.2018.05.002 [ Links ]
25. Chalas R, Rykwa D, Wróbel-Dudzinska D, et al. Subjective Complaints of Ocular Dryness and Xerostomia Among the Non-Sjögren Adult Population of Lublin Region, Poland. Med Sci Monit. 2018;24:200-206. DOI: 10.12659/MSM.906618 [ Links ]
26. Uchino M, Kawashima M, Uchino Y, et al. The evaluation of dry eye mobile apps for screening of dry eye disease and educational tear event in Japan. Ocul Surf. 2018;16(4):430-435. DOI: 10.1016/j.jtos.2018.06.002 [ Links ]
27. Kocaçal Güler E, Eser I, Egrilmez S. Nurses can play an active role in the early diagnosis of exposure keratopathy in intensive care patients. Jpn J Nurs Sci. 2018;15(1):31-38. DOI: 10.1111/jjns.12165 [ Links ]
28. Schub T, Mennella H. Dry Eye Syndrome. CINAHL Nursing Guide. 2018. Available from: https://research.ebscomedical.com/eds?search=y&query=%22Mennella%20H%22&type=AR&ff[]=SubjectEDS%3Amedical-surgical%20nursing&searchfield=AU&resultsperpage=25&pagenumber=1 [ Links ]
29. Araújo JNM, Fernandes APNL, Silva HP, et al. Ojo seco y enfermedades de la córnea en pacientes en cuidados intensivos. Rev Cubana Enferm. 2018;34(2):456-470. Available from: http://scielo.sld.cu/scielo.php?pid=S0864-03192018000200018&script=sci_abstract&tlng=pt [ Links ]
30. Graham AD, Lundgrin EL, Lin MC. The Berkeley Dry Eye Flow Chart: A fast, functional screening instrument for contact lens-induced dryness. PLoS ONE. 2018;13(1); 1-18. DOI: 10.1371/journal.pone.0190752 [ Links ]
Received: March 17, 2023; Accepted: September 29, 2023











 text in
text in