My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.23 n.73 Murcia Jan. 2024 Epub Feb 23, 2024
https://dx.doi.org/10.6018/eglobal.555891
Reviews
Complementary techniques of relaxation and non-pharmacological analgesia during childbirth: systematic review
1University of Alcala. Alcalá de Henares, Madrid. Spain
2Department of Physiotherapy, University of Murcia, Murcia. Spain
3School of Nursing. Faculty of Health Sciences. University of Granada, Granada, Spain
Introduction:
There is a need to provide analgesia strategies that encourage and promote women's participation in decision-making at the time of delivery and relaxation techniques could be a complementary and/or alternative non-pharmacological analgesic method to the widely used epidural anaesthesia in standard labour care.
Objective:
The objective of this study is to analyze the obstetric effects of relaxation techniques on pain management during labour.
Method:
A systematic review is performed with critical reading of included studies. The search for studies was carried out in the main databases MEDLINE, Cochrane Library, Cuiden, LILACS and SciELO. Studies published in English or Spanish between 2015 and February 2021 were included. Eleven studies were included, six of which are systematic reviews and five are randomised clinical trials. The interventions analysed were relaxation techniques such as hypnosis, intradermal injection of sterile water, warm water immersion, massage, acupuncture, music therapy, aromatherapy, continuous support and mind-body practices like relaxing breathing, yoga and meditation, among others.
Conclusion:
The main conclusion of this study is that relaxation techniques may decrease the level of pain during labour, although the current scientific evidence is limited and the methodological quality varies from low to moderate. More randomised controlled trials are needed to support this research.
Keywords: Analgesia; Pain; Labour; Relaxation techniques; Complementary therapies
INTRODUCTION
The labour process varies from woman to woman and its progress does not necessarily have to be linear in all cases. In most nulliparous women the dilation phase is completed in 18 hours and in the case of multiparous women it takes an average of 12 hours (1), all this time passes with painful perineal and lumbar sensations that are generally more intense in primiparous women than in multiparous women(2,3).
Pain during childbirth is described as one of the most intense pains a woman can experience in her lifetime. Currently, pain management is not only of interest from the point of view of symptomatic relief, but also because of the physiological changes it produces in the mother and foetus(3,4,5,6,7). Authors such as Mallen Pérez et al.(8) and Cobo Borda et al. (1) report how childbirth was considered a natural event and was handled by primitive societies in a totally instinctive and solitary manner (1,8), while in some religions it was considered a punishment(1). The concept of pain in childbirth was modified and considered an emotion during periods such as the Middle Ages, the Renaissance and the Industrial Revolution(1,9). Controlling pain in labour brings with it an increase in the physical and emotional well-being of the pregnant woman, which is why in the mid-19th century work began on the concept of pain during childbirth, in which medical care began to be provided and pharmacological analgesia was introduced, from ether and chloroform to the appearance of epidural analgesia(8).
Each woman's expression of pain must be respected, and therefore it is necessary to personalise the resources available for pain relief and pain management during labour. These resources can be pharmacological or non-pharmacological, the latter of which can be divided into relaxation methods, psychological techniques and mechanical techniques. The use of non-pharmacological analgesic methods that are safer for both mother and foetus can be an alternative to pharmacological analgesic methods that may carry various risks, as in the case of epidural analgesia(4,6,10,11). In particular, non-pharmacological analgesic methods such as relaxation techniques, among which we find: warm water immersion, massage and reflexology, acupuncture and acupressure, music therapy, aromatherapy, continuous support or mind-body practices that include yoga, meditation, visualisation and breathing techniques, among others. We could also make use of psychological techniques such as hypnosis or mechanical techniques such as transcutaneous electrical nerve stimulation, use of a birthing ball or Swiss ball, thermal therapies and intradermal injection of sterile water(4,12).
Currently, according to various studies, pregnant women are provided with more information on pharmacological methods of pain relief (especially epidural analgesia) than on the various alternative non-pharmacological methods. Some studies conclude that it would be advisable for professionals to continue searching for the most suiTable way to care for each woman according to her preferences in order to adapt to each situation that arises and to offer all the existing analgesic options, both pharmacological and non-pharmacological(6,10,11,12,13,14).
Because pain management during labour is a fundamental task that health professionals must address with the highest possible quality and, on the other hand, because pain in the labour process can cause alterations in the pulmonary and cardiovascular systems, considerably reducing tolerance to labour, there is a need to offer analgesia strategies that encourage and promote the participation of women in decision-making at the time of labour. Relaxation techniques could be a complementary and/or alternative non-pharmacological analgesic method in labour(6,7,11,12,13,14,15,16,17).
MATERIALS AND METHODS
Objective
To analyse the obstetric effects of relaxation techniques on pain management during labour.
Design
A systematic review was carried out with critical reading of the included studies on analgesia and relaxation techniques during labour.
Eligibility criteria
Inclusion criteria. We included studies whose participants were women in labour. In turn, we included studies whose type of interventions evaluated the main non-pharmacological analgesic methods used to control pain in labour, including: Hypnosis, Transcutaneous electrical nerve stimulation, Intradermal injection of sterile water, Immersion in water, Massage and reflexology, Acupuncture and acupressure, Music Therapy, Aromatherapy, Continuous support and Mind-body relaxation practices through breathing tecniques, yoga or meditation.
In addition, the interventions could be a specific relaxation technique or a combination of several techniques, thus forming the intervention under study.
We incorporated experimental studies (such as randomised controlled clinical trials (RCT)), systematic reviews (SR) and/or meta-analyses of experimental studies, observational studies evaluating the effect of any non-pharmacological method on pain control during labour, and Clinical Practice Guidelines addressing clinical questions related to the topic of study.
Exclusion criteria. We excluded studies whose interventions were studied at stages other than childbirth, such as during gestation or postpartum. Articles with a publication date prior to 2015 and in a language other than English or Spanish were excluded. We also excluded qualitative studies, research protocols and studies for which we were unable to access the full text.
Sources of information
Different databases were consulted from October 2020 to February 2021, such as Medline, Cochrane Library, Cuiden, LILACS and SciELO. The library of Clinical Practice Guidelines of the National Health System was also accessed through GuíaSalud.
Search strategy
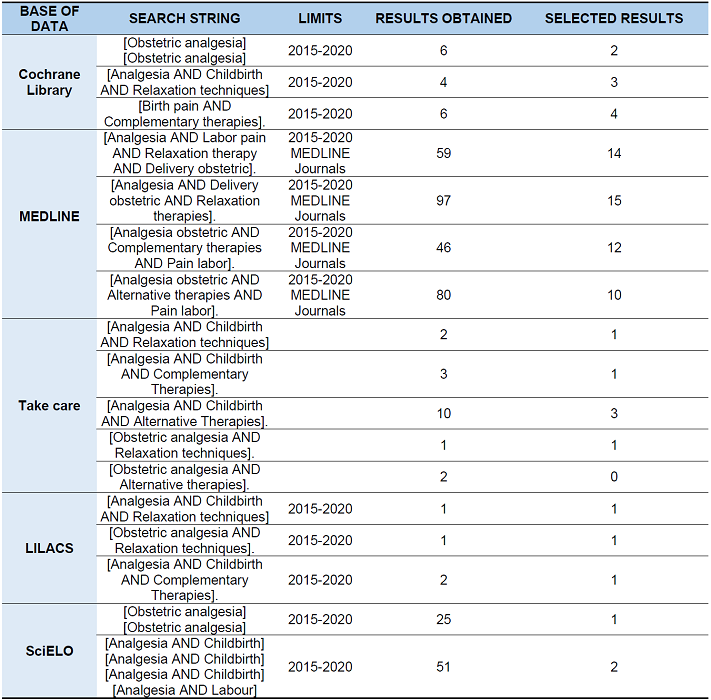
The limits used in the bibliographic search strings were the date of publication (between January 2015 and February 2021), the language (Spanish or English) and in some search strings the full availability of the text was used. In turn, in the Medline database, it was added as an attribute of the articles found that they were included in Medline journals.
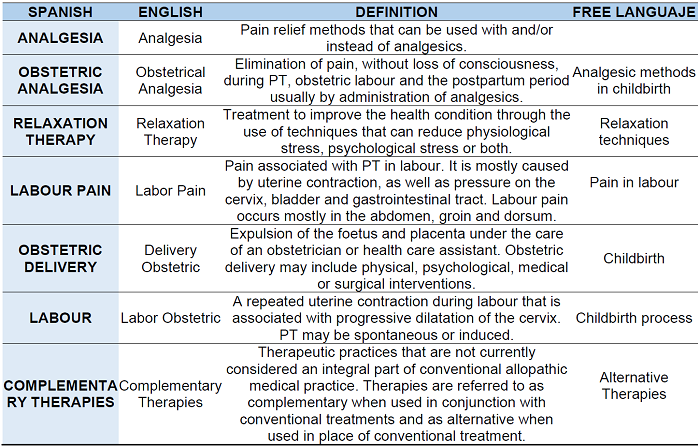
The descriptors used in the search strings Appendix Awere previously consulted in DeCS(18) and MeSH (19) and the free language used in the bibliographic searches was obtained from HONSelec(20).
The boolean AND operator was used in several search strings.
We also conducted a reverse search for studies from those that were potentially relevant to this review.
Selection process
After conducting the search for studies, those that were not related to the topic of study were eliminated by reading the title, abstract and keywords. The full text was also accessed where necessary in order to decide whether the information they contained was related to the topic of study. The studies selected as potentially relevant were then read in full and those that did not relate to the topic of study or did not meet the inclusion criteria were discarded.
Finally, the following data was recorded for the included studies: author and year, design, objective, intervention, participants and main results through statistical data.
Risk of bias in individual studies
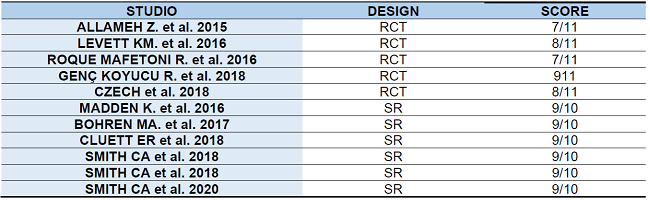
The methodological quality of the included full-text studies was assessed using the critical reading tool CASPe [21] tool, discarding those that did not achieve a score greater than or equal to 7 of the 11 items that make up the assessment guide for clinical trials and greater than or equal to 6 of the 10 items for systematic reviews or meta-analyses. The score obtained from the critical reading of the included studies is attached Appendix B).
RESULTS
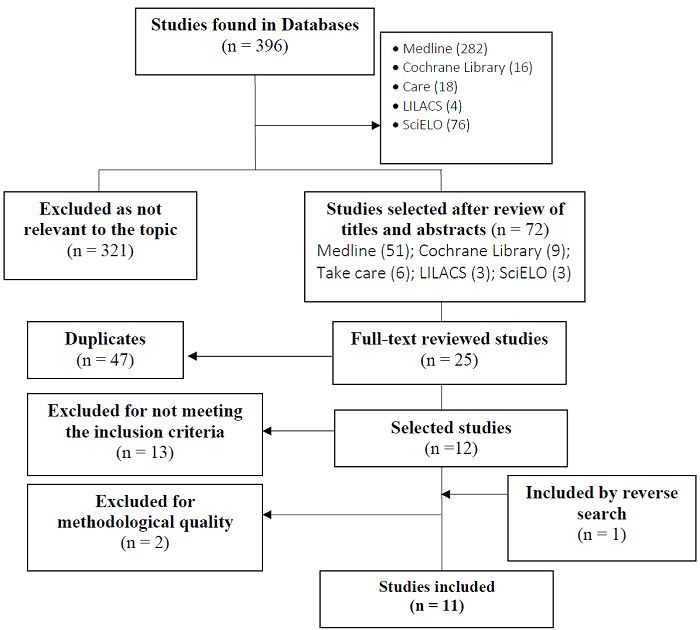
In the initial search strategy, a total of 72 studies were identified, which were successively screened according to the purpose of the present study until the selection of studies was reached (Figure 1). Finally, 11 studies were included in this review, 6 of which are systematic reviews and 5 are randomised clinical trials.
Flow chart of the study: The results obtained from the main search strings used in databases are presented in (Appendix C).
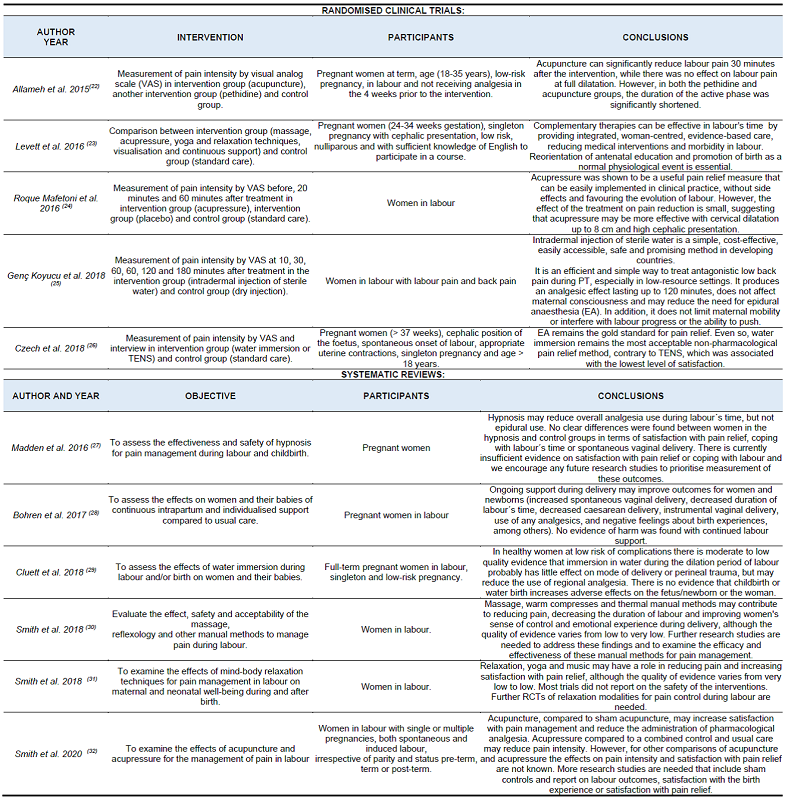
The results obtained from the included studies are described below. First, the most relevant characteristics of the included studies are presented (Table 1). Finally, the main results on relaxation techniques as a non-pharmacological analgesic method used during labour are discussed.
The results of this review presented in the Table above aim to achieve the objective proposed for this work. All the selected studies, regardless of their design, study patients belonging to the same population group, in this case women during pregnancy and childbirth. To analyse the obstetric effects of relaxation techniques in the treatment of pain during labour, 11 articles were analysed, including the study by Allameh et al. (22) in which a comparative study was carried out between pregnant women treated with acupuncture and pregnant women treated with pethidine and their relationship with pain during labour. With regard to the same variable, in this case pain control, Roque Mafetoni et al. (24) worked with acupressure at the time of delivery and found positive results. Genç Koyucu et al. (25), in their study, presents the ability to reduce pain with an intradermal injection of sterile water, which is also useful because it does not limit maternal mobility or interfere with the progress of labour or the ability to push. In any case, the literature indicates that immersion in water is the non-pharmacological treatment of choice, as highlighted by Czech et al. Cluett et al. (29), refer in their work on the same subject.
Another relevant study was that of Levett et al. (23) where they claim to reorient prenatal education and promote childbirth as a normal physiological event. Madden et al. (27), work on the effectiveness of hypnosis at the time of delivery, corroborating the reduction of analgesia used in cases treated with this therapy.
Smith et al. (30) examine massage therapies, reflexology and other manual methods for the treatment of pain during labour. In addition, they examine the effects of mind-body relaxation techniques for pain management during labour on maternal and neonatal well-being during and after birth (31).
DISCUSSION
The eleven studies included in this systematic review suggest very limited ascientific evidence on relaxation techniques during labour. Due to the small number of studies examining different methods of non-pharmacological analgesia during labour, there is a limitation in making comparisons with other studies. This is highlighted in his latest study on the subject Yinchu et al. (32), where he stresses the need for more well-designed projects to validate the conclusions of his work.
It is true that this study attempts to investigate the most recent scientific evidence and, if possible, the highest methodological quality by using limits in the search chains and through a critical reading of the selected studies. The heterogeneity of the results is also accepted, mainly due to the specific objectives of examining and learning about the different non-pharmacological analgesia methods used, be they relaxation techniques, comfort measures and/or ways to control pain during labour.
During the process of preparing the study we tried to minimise the risk of bias and although the search for studies was exhaustive, accurate and in widely used languages such as English or Spanish, it is possible that some of the literature on relaxation techniques is not published in journals and therefore excluded from the main databases, so we cannot rule out the possibility that studies of interest may have been missed.
Relaxation techniques
Hypnosis
Madden et al. (27) found that pain intensity was lower for women in a self-hypnosis or hypnotherapy group than for those in a standard care group using the McGill Pain Questionnaire in a trial of 60 women [MD] -0.70 (95% CI -1.03 to -0.37); (p < 0.0001). They further concluded that hypnosis may reduce overall analgesia use during labour, but not epidural use.
TENS
In an RCT by Czech et al. (27) comparing pharmacological and non-pharmacological methods of labour pain relief, epidural analgesia (EA) was the standard method for pain relief and water immersion was the most accepTable non-pharmacological pain relief method, contrary to TENS, which was associated with the lowest level of satisfaction.
Intradermal injection of sterile water
A randomised controlled clinical trial by Genç Koyucu et al. (25) assessed pain during labour through visual analogue scale (VAS) at 10, 30, 60, 60, 120 and 180 minutes after giving sterile water injections to one intervention group and dry injections to another control group in the Michaelis rhombus of the sacral area.
Pain scores were assessed at 10, 30, 60, 60, 120 and 180 minutes using a visual analogue scale. In addition, the need for epidural analgesia, Apgar score, mode of delivery, timing of delivery, maternal satisfaction and breastfeeding score were assessed.
The mean back pain scores at 30 minutes after the injections were significantly lower in the intervention group (31.66 ± 11.38) than in the control group (75 ± 18.26); (p < 0.01). The mean decrease in pain scores after 30 minutes from baseline was significantly higher in the study group (54.82 ± 7.81) than in the control group (13.33 ± 12.05); (p < 0.01). The need for epidural analgesia, labour time, mode of delivery, Apgar and lactation scores were similar in both groups. In addition, maternal satisfaction with the analgesic effect was significantly higher in the intervention group (84.5%) compared to the control group (35.7%); (p <0.01).
Intradermal sterile water injections have therefore proved to be a simple, cost-effective, easily accessible, safe and promising method, especially in developing countries, for treating antagonistic low back pain during labour. It produces an analgesic effect lasting up to 120 minutes, does not affect maternal consciousness and may reduce the need for EA. In addition, it does not limit maternal mobility or interfere with the progress of labour or the ability to push.
Aromatherapy
No studies addressing aromatherapy as a non-pharmacological analgesic method during labour are included in this review. However, it is worth highlighting a contribution made Yinchu et al. (33) in her study, where she presents that the results obtained in her work support the use of aromatherapy to alleviate labour pain in low-risk pregnant women.
Water immersion
In the RCT by Czech et al. (26) comparing pharmacological and non-pharmacological methods of labour pain relief, there was no statistical difference in the level of pain experienced in the water immersion intervention group (p > 0.05) but it did achieve the highest levels of maternal satisfaction (n = 38; 95%). Still, water immersion was the most accepTable non-pharmacological pain relief method.
The SR of Cluett et al. (29) highlights the use of EA: In the first stage of labour the intervention group (39%) and the control group (43%); [RR] 0.91 (95% CI 0.83 to 0.99); (p = 0.03). While in the second stage of labour no statistical difference in pain intensity is shown (p > 0.05). Finally, it was concluded that, in healthy women at low risk of complications, immersion in water during the dilation period of labour could probably reduce the use of EA.
Continuous support
Bohren et al. (28) found a lower number of negative feelings about the labour experience in the intervention group (continuous support) and the control group (standard care) in the intervention group than in the control group through a SR where the experience during labour was measured through interviews: [RR] 0.69 (95% CI 0.59 to 0.79); (p < 0.0001).
Levett et al. (23) also provide related results, as EA use in the intervention group (continuous support) was lower than in the control group (standard care): [RR] 0.35 (95% CI 0.23 to 0.52); (p ≤ 0.001).
Acupuncture and acupressure
According to an RCT by Allameh et al. (22) comparing the mean pain intensity score of subjects 30 minutes after the intervention: In the intervention group (acupuncture) the mean pain intensity was determined as 5.77 with the minimum of 3 and maximum of 9; in the other intervention group (pethidine), the mean was 6.87 with the minimum of 4 and maximum of 10, and in the control group the mean pain intensity was measured as 7.8. ANOVA test showed a significant difference between the three groups (p = 0.0001).
Roque Mafetoni et al. (24) through an RCT, shows the differences occurring at 20 and 60 minutes between the intervention group (acupressure), another intervention group (placebo) and control group (standard care). The means of pain did not vary in any group before treatment (p=0.0929), however, they were lower in the intervention group (acupressure) at 20 minutes (p-value=<0.0001) and also after 60 minutes (p=0.0001) when compared to the placebo and control groups.
Another RCT, in this case by Levett et al. (23) supports the above results, as EA use in the intervention group (acupressure) was lower than in the control group (standard care): [RR] 0.35 (95% CI 0.23 to 0.52); (p ≤ 0.001).
On the other hand, in the SR by Smith et al. (32) no statistical differences in pain intensity (p > 0.05) were observed between the control group (acupuncture or acupressure) and the control group (standard care).
Yinchu et al. (33) in their study highlight that the use of acupressure improves labour pain in low-risk pregnant women.
Music therapy
Only Smith et al. (31) through a SR shows results about music therapy during labour, specifically during the latent phase, a decrease in pain intensity was observed in the intervention group (music) compared to the control group (standard care) [MD] -0.73 (95% CI -1.01 to -0.45); (p < 0.0005).
Massage and reflexology
A SR by Smith et al. (30)shows a decrease in pain intensity in the intervention group (massage) compared to the control group (standard care) in the dilation period [DME] -0.81 (95% CI -1.06 to -0.56); (p < 0.0001), while no statistically significant differences were observed in the second stage of labour and delivery (p > 0.05). In the same study, lower levels of pain were observed in the intervention group (warm compresses) compared to the control group (standard care) in both the first and second stages of labour [SMD] -0.59 (95% CI -1.18 to -0.00); (p = 0.05) and [SMD] -1.49 (95% CI -2.85 to -0.13); (p = 0.03) respectively. On the other hand, the intervention group (other manual thermal methods) were also effective in reducing pain in the dilation period [MD] 1.44 (95% CI -2.24 to -0.65); (p = 0).
The RCT by Levett et al. (23) supports this finding as EA use in the intervention group (massage) was lower than in the control group (standard care): [RR] 0.35 (95% CI 0.23 to 0.52); (p ≤ 0.001).
Therefore, massage, warm compresses and manual thermal methods can help to reduce pain, shorten the duration of labour and improve women's sense of control and emotional experience during labour.
Mind-body practices
The SR of Smith et al. (31) assesses pain intensity in intervention groups with mind-body relaxation practices including breathing techniques, yoga and meditation and control groups with standard care. A decrease in pain was observed in the intervention group with relaxation and mind-body techniques during the latent phase of labour [MD] - 1.25 (95% CI -1.97 to -0.53); (p = 0) and yoga techniques [MD] -6.12 (95% CI -11.77 to -0.47); (p = 0.03).
The RCT by Levett et al. (23) reports results along the same lines, as EA use in the intervention group (yoga and breathing techniques) was lower than in the control group (standard care): [RR] 0.35 (95% CI 0.23 to 0.52); (p ≤ 0.001).
Limitations
The main limitation of the study, the small number of studies published about the different methods of non-pharmacological analgesia during labor made it difficult to make comparisons with other studies. Likewise, the existing heterogeneity of the results was accepted, essentially due to the specific objectives set to examine and learn about the different non-pharmacological analgesic methods used, whether they are relaxation techniques, comfort measures and/or ways to control pain during the birth.
CONCLUSIONS
The main findings of this review include several areas that should be highlighted.
Firstly, the clinical implications of the subject matter of this review indicate that the results of the included studies on relaxation techniques during labour show a possible decrease in labour pain compared to usual care. In turn, there are results of moderate methodological quality showing a decrease in pain in the early stages of labour in those women in whom certain relaxation techniques were performed.
Even so, no study has found negative effects on the health of women and their babies, so it would be of interest to promote this type of therapy and study its follow-up.
In terms of research, it would be desirable for future research to follow the same line of investigation through the development of RCTs, due to the small number of studies present in the databases that analyse the different methods of non-pharmacological analgesia during childbirth. This aspect is recognised by all the authors included in this review.
With regard to the management of this type of therapy, it would be advisable for health professionals attending childbirth to receive ongoing training on the different pharmacological and non-pharmacological methods of analgesia, in order to develop analgesic strategies that encourage and favour the participation of women in decision-making at the time of delivery. This work should be backed and supported by appropriate health and educational policies.
The current scenario in which these therapies are being developed is still far from complete. This review concludes that the approach to childbirth treated with this type of therapy favours the woman and the baby, although a more thorough and detailed study is needed to understand the scope of these therapies in greater depth. At the same time, specific training for health professionals on this subject is crucial for the evolution of this type of treatment.
REFERENCES
1. Cobo Borda J.G., Diaz Piedrahíta, S.; Hernández Castro, J.J.; Mendoza-Vega, J.; Montoya Vargas, C.; Moreno Benavides, C.; Palacios Sánchez, L.; Ruiz Sternberg, A.M.; Ruiz Sternberg, J.E.; Vélez van Beermeke, A. Lecciones de historia del dolor; Centro Editorial Universidad del Rosario, Ed.; 1ª; Bogotá, 2005; ISBN 958-8225-58-. [ Links ]
2. De Sanidad, M.; Política Social, Y. Guía de Práctica Clínica sobre la Atención al Parto Normal; Eusko Jaurlaritzaren Argitalpen Zerbitzu Nagusia, Ed.; 1a.; Vitoria-Gasteiz, 2010; ISBN 978-84-457-3090-4. [ Links ]
3. Molina, F. Tratamiento del dolor en el parto. Rev Soc Esp Dolor 1999, 6, 292-301. [ Links ]
4. Ortiz-Gómez, J.R.; Palacio-Abizanda, F.J.; Fornet-Ruiz, I. Técnicas analgésicas para el parto: alternativas en caso de fallo de la epidural. An. Sist. Sanit. Navar. 2014, 37, 411-427, doi:10.4321/s1137-66272014000300010. [ Links ]
5. Berrocal Gil, A.B.; Galán Martín de la Leona, D.; Parreño Sánchez, R.M.; Mateo Jurado, I. Analgesia en el trabajo de parto. Enferm Integr. 2013, 101, 25-29. [ Links ]
6. Gomezese, O.F.; Estupiñan Ribera, B. Analgesia obstétrica: situación actual y alternativas. Rev. Col. Anest. 2017, 45, 132-137, doi:10.1016/j.rca.2017.01.002. [ Links ]
7. Anim-Somuah, M.; Smyth, R.M.D.; Cyna, A.M.; Cuthbert, A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst. Rev. 2018, doi:10.1002/14651858.CD000331.pub4. [ Links ]
8. Mallén-Pérez, L.; Eulàlia Juvé-Udina, M.; Roé-Justiniano, M.T.; Domènech-Farrarons, À. Dolor de parto: análisis del concepto. Matronas Prof 2015, 16, 61-67. [ Links ]
9. Manuel Sedano, L.; Cecilia Sedano, M.; Rodrigo Sedano, M. Reseña histórica e hitos de la obstetricia. Rev. Médica Clínica Las Condes 2014, 25, 866-873, doi:10.1016/s0716-8640(14)70632-7. [ Links ]
10. Mallén Pérez, L.; Terré Rull, C.; Palacio Riera, M. Inmersión en agua durante el parto: revisión bibliográfica. Matronas Prof 2015, 16, 108-113. [ Links ]
11. Fernández Medina, I.M. Alternativas analgésicas al dolor de parto. Enferm. Glob. 2014, 13, 400-406. [ Links ]
12. Ballesteros Calero, C.; Velázquez López, R.; Luque Díaz, M. Atención al parto normal: análisis comparativo de recomendaciones propuestas en España - Revista Matronas. Matronas hoy 2013, 1, 6-12. [ Links ]
13. Smith, C.A.; Collins, C.T.; Cyna, A.M.; Crowther, C.A. Complementary and alternative therapies for pain management in labour. Cochrane Database Syst. Rev. 2006, 1-37, doi:10.1002/14651858.cd003521.pub2. [ Links ]
14. Caballero Barrera, V.; Santos Pazos, P.J.; Polonio Olivares, M.L. Alternativas no farmacológicas para el alivio del dolor en el trabajo de parto. Nure Investig. 2016, 13, 1-7. [ Links ]
15. Federación de Asociaciones de Matronas de España Iniciativa Parto Normal. Guía para madres y padres. 2011 [ Links ]
16. Ministerio de Sanidad, Servicios Sociales e Igualdad Informe sobre la Atención al Parto y Nacimiento en el Sistema Nacional de Salud; 2012; [ Links ]
17. Huntley, A.L.; Coon, J.T.; Ernst, E. Complementary and alternative medicine for labor pain: A systematic review. Am. J. Obstet. Gynecol. 2004, 191, 36-44, doi:10.1016/j.ajog.2003.12.008. [ Links ]
18. DeCS - Descriptores en Ciencias de la Salud. https://decs.bvsalud.org/es/ [ Links ]
19. Inicio - MeSH - NCBI. https://www.ncbi.nlm.nih.gov/mesh/ [ Links ]
20. HONselect Available online: https://www.hon.ch/HONsearch/Pro/honselect_sp.html(accessed on Feb 1, 2022). [ Links ]
21. CASPe | Programa de Habilidades en Lectura Crítica Español Critical Appraisal Skills Programme Español. https://redcaspe.org/l [ Links ]
22. Allameh, Z.; Tehrani, H.; Ghasemi, M. Comparing the impact of acupuncture and pethidine on reducing labor pain. Adv. Biomed. Res. 2015, 4, 46, doi:10.4103/2277-9175.151302. [ Links ]
23. Levett, K.M.; Smith, C.A.; Bensoussan, A.; Dahlen, H.G. Complementary therapies for labour and birth study: a randomised controlled trial of antenatal integrative medicine for pain management in labour. BMJ Open 2016, 6, e010691, doi:10.1136/bmjopen-2015-010691. [ Links ]
24. Mafetoni, R.R.; Shimo, A.K.K. The effects of acupressure on labor pains during child birth: randomized clinical trial. Rev. Lat. Am. Enfermagem 2016, 24, e2738, doi:10.1590/1518-8345.0739.2738. [ Links ]
25. Genç Koyucu, R.; Demirci, N.; Ender Yumru, A.; Salman, S.; Ayanoglu, Y.T.; Tosun, Y.; Tayfur, C. Effects of intradermal sterile water injections in women with low back pain in labor: A randomized, controlled, clinical trial. Balkan Med. J. 2018, 35, 148-154, doi:10.4274/balkanmedj.2016.0879. [ Links ]
26. Czech, I.; Fuchs, P.; Fuchs, A.; Lorek, M.; Tobolska-Lorek, D.; Drosdzol-Cop, A.; Sikora, J. Pharmacological and non-pharmacological methods of labour pain relief-establishment of effectiveness and comparison. Int. J. Environ. Res. Public Health 2018, 15, 2792, doi:10.3390/ijerph15122792. [ Links ]
27. Madden, K.; Middleton, P.; Cyna, A.M.; Matthewson, M.; Jones, L. Hypnosis for pain management during labour and childbirth. Cochrane Database Syst. Rev. 2016, doi:10.1002/14651858.CD009356.pub3. [ Links ]
28. Bohren, M.A.; Hofmeyr, G.J.; Sakala, C.; Fukuzawa, R.K.; Cuthbert, A. Continuous support for women during childbirth. Cochrane Database Syst. Rev. 2017, 2017. [ Links ]
29. Cluett, E.R.; Burns, E.; Cuthbert, A. Immersion in water during labour and birth. Cochrane Database Syst. Rev. 2018, 1-114, doi:10.1002/14651858.CD000111.pub4. [ Links ]
30. Smith, C.A.; Levett, K.M.; Collins, C.T.; Dahlen, H.G.; Ee, C.C.; Suganuma, M. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst. Rev. 2018, doi:10.1002/14651858.CD009290.pub3. [ Links ]
31. Smith, C.A.; Levett, K.M.; Collins, C.T.; Armour, M.; Dahlen, H.G.; Suganuma, M. Relaxation techniques for pain management in labour. Cochrane Database Syst. Rev. 2018, doi:10.1002/14651858.CD009514.pub2. [ Links ]
32. Smith, C.A.; Collins, C.T.; Levett, K.M.; Armour, M.; Dahlen, H.G.; Tan, A.L.; Mesgarpour, B. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst. Rev. 2020, doi:10.1002/14651858.CD009232.pub2. [ Links ]
33. Hu, Y.; Lu, H.; Huang, J.; Zang, Y. Efficacy and safety of non-pharmacological interventions for labour pain management: A systematic review and Bayesian network meta-analysis. J. Clin. Nurs. 2021, 30, 3398-3414, doi:10.1111/jocn.15865. [ Links ]
Received: February 02, 2023; Accepted: July 08, 2023











 text in
text in