My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.23 n.73 Murcia Jan. 2024 Epub Feb 23, 2024
https://dx.doi.org/10.6018/eglobal.579091
Reviews
Strategies to ensure the critical patient safety
1Nurse. Doctorate Student in Nursing at the Universidad Nacional Mayor de San Marcos. Lima Peru
2Doctor in Nursing, Professor at the Federal University of Santa Catarina, Graduate Program in Nursing. Florianópolis, Santa Catarina, Brazil
3Doctor in Nursing, Professor at the Universidad Nacional Mayor de San Marcos, Graduate Program in Nursing. Lima Peru
Method:
Integrative review, search carried out in May 2022 using the data sources: MEDLINE, SciELO, WOS, LILACS, Scopus and IBECS. The analysis and synthesis were built from the results found, seeking to group them by categories based on the similarity of content.
Results:
377 articles were found, then the inclusion criteria and exhaustive reading were applied, resulting in a sample of 13 articles. The results were classified into five categories: Prevention of pneumonia associated with mechanical ventilation; Safety in the administration of management of medicines; Prevention of pressure injuries; Educational program oriented to patient safety in intensive care and; Reflections of the health team regarding safety culture.
Conclusions:
This study contributes to comprehensively identify the various strategies whose results demonstrated a positive change in the prevention of adverse events and strengthening of safety in health care.
Keywords: Strategies; Guideline; Patient safety; Intensive care unit; Nurses
INTRODUCTION
Since 1999, patient safety became more relevant after the report To err is human: building a safer health system, by the American Institute of Medicine. In response to the alarming results of this report, the World Health Organization ( WHO) creates the World Alliance for Patient Safety with the purpose of coordinating, disseminating and accelerating improvements in patient safety throughout the world; with emphasis on encouraging research, to improve the safety of health care, having as a primary tool the notification of adverse events (AE) in order to prevent them through the implementation of various strategies applied to the reality of each country(1).
The intensive care unit is one of the essential elements of the health system, patients admitted to these units are characterized by hemodynamic instability, the use of various drugs to induce sleep, ventilatory support and other medical procedures. Due to these conditions, patients are vulnerable to various incidents. Saldana et al.(2)in his study applied in 17 Intensive Care Units (ICU) in Argentina, Colombia and Mexico, found that the most relevant adverse events were those linked to direct care and airway management. Being 94.8% due to preventable errors.
Taking into account how complicated it is to develop a unique and immediate solution to this problem, over the years, various studies have been carried out that evaluate the knowledge that the nurse has regarding to safety, using the questionnaire Hospital Survey on Patient Safety Culture(3). Some studies focused on the factors associated with pressure injuries(4), medication errors (5), infections associated with the use of mechanical ventilators(6). And others focused on the behavior of the personnel for the prevention of infections associated with the use of the central venous catheter(7), and the bladder catheter (8). However, no studies were found where all these guidelines, plans or programs aimed at patient safety are integrated and compared, resulting in health professionals not being able to quickly and punctually access a set of strategies that can be applied to its reality.
To respond to this problem, an integrative review of the literature was carried out with the aim of identifying strategies to guarantee patient safety in intensive care units.
METHOD
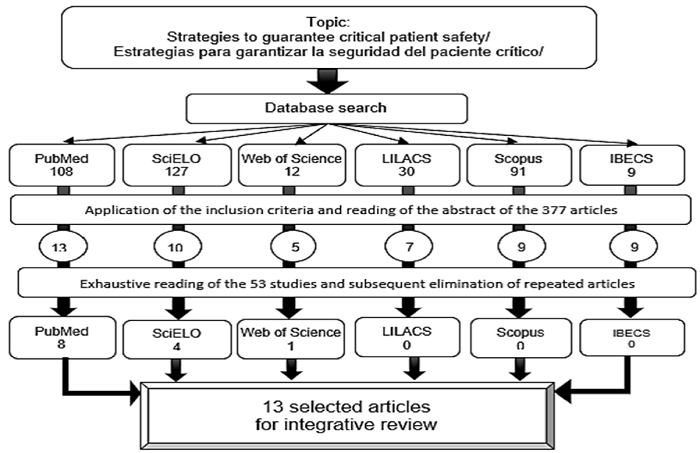
Integrative review whose search and selection of articles was carried out in May 2022 through access to the platforms of the following data sources: MEDLINE via PubMed, SciELO, WOS, LILACS, Scopus and IBECS.
The inclusion criteria were: Randomized articles, qualitative and quantitative investigations, clinical investigations, carried out from 2017 to 2022, with free access to the full text, in Spanish, English and Portuguese. The exclusion criteria were integrative, informative review articles, event summaries, books, theses, duplicity, case reports, unavailable material, outside the established time frame, and those referring to pediatrics, neonatology, or maternal care.
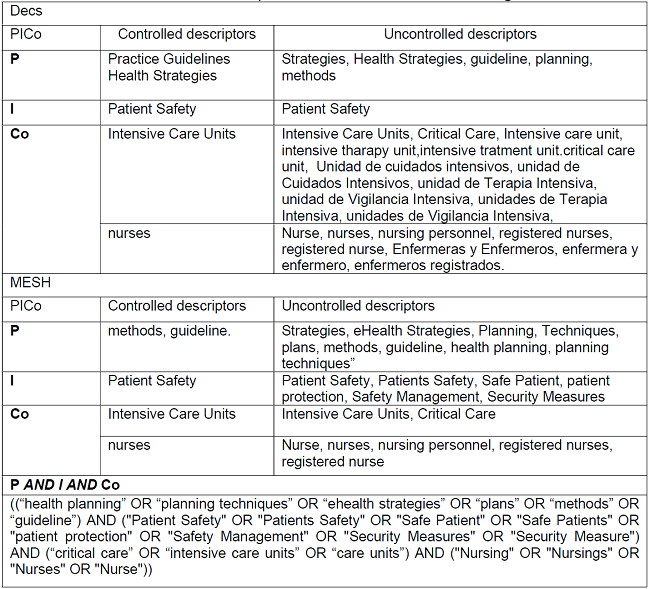
For the operationalization of the search, the controlled descriptors indexed in Descriptores em Ciências da Saúde (DeCS), Medical Subject Headings (MeSH) were used. The Boolean operators used for electronic scanning were OR and AND. Table 1presents the PICo question and the controlled descriptors.
A total of 377 articles were identified, then they were selected after reading the title and abstract, verifying that the investigations met the inclusion and exclusion criteria, as a result of this process a total of 47 articles remained, subsequently proceeded to rigorously reading each one of them, focusing attention mainly on the methodology and the results, finally remaining 13 articles
RESULTS
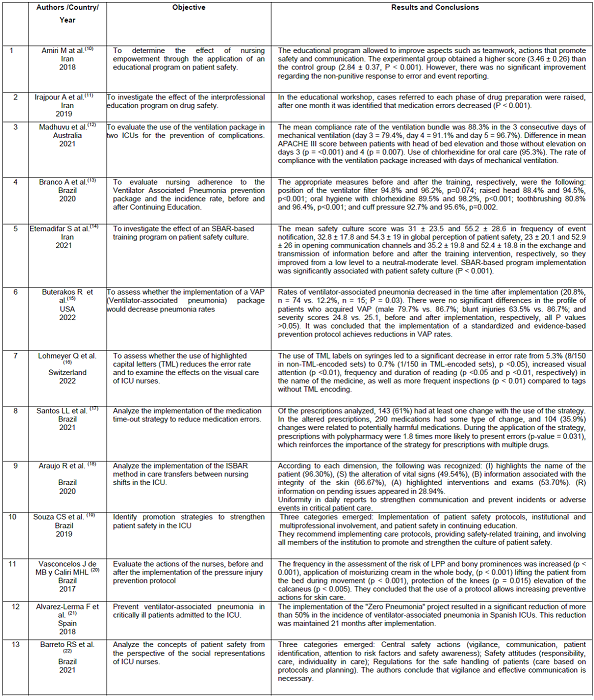
The 13 articles selected 84.62% (11/13) were quantitative studies and 15.38% (2/13) qualitative study. The investigations came from Brazil 46.15% (6/13), Iran 23.08% (3/13), and Australia, the United States, Spain, Switzerland 7.69% (1/13) respectively. The main characteristics of the 13 studies that make up the sample of this review are shown in Table 1
DISCUSSION
From the results found in the reviewed articles, the strategies were classified into the following categories:
Prevention of ventilator-associated pneumonia
Pneumonia associated with mechanical ventilation (VAP) is one of the most common intrahospital infections (IAS) and represents 24% and 27% of mortality in intensive care units(23). For this reason, many countries have focused various efforts to reduce damage and improve patient care in mechanical ventilation.
The strategies found are based on two clear elements: Establishing a VAP prevention program or package(12) (15) (21)and the continuous education of health personnel, especially nursing personnel, who are responsible for the continuous care of critically ill patients ((13).
For the evaluation of the effectiveness of the established strategies, the investigations made use of a checklist containing the following dimensions: Hand washing(15),(21); elevation of the head of the bed 30° - 45°(12) (13) (15) (21); daily oral care with chlorhexidine 0.12-0.2%(12) (13) (15) (21); tooth brushing(13);cuff pressure(13) (15) (21); subglottic aspirations(15),(21), endotracheal tube rotation(15); evaluation of the mechanical ventilator circuit, humidifiers, filters(13) (15) (21); 24-hour administration of antibiotics(21); daily analysis of sedation variations and daily assessment for extubation(12) (15) (21); gastrointestinal prophylaxis(12),(15); DVT prophylaxis(12).
From the set of activities, it was found that only 50% refer to hand washing as the first activity. The Pan American Health Organization (PAHO) considers hand washing the first measure to reduce infections associated with health care (IAS)(24). Consequently, it is necessary that any guide and/or protocol start with this first action, avoiding assuming that the health team will carry it out.
Tooth brushing is the second action that is present in only one article(13). When contrasting it with the literature, we found that toothbrushing does not determine the decrease in VAP by itself. However, if it is associated with the use of chlorhexidine, better results are evident(25). This would explain why the other investigations would not consider it as part of their list of activities.
Subglottic aspiration is addressed by two articles(15),(21). The study by Pozuelo et al. found an effective result in reducing the incidence of VAP and mortality in the ICU(26). Therefore, it is recommended that all NAV prevention packages insert this activity.
Regarding gastric prophylaxis and DVT, no direct results were found to reduce the incidence of VAP or mortality in the ICU.
Likewise, the commitment and strict compliance with the safety measures for the prevention of infections during the entire hospital stay of the patient is necessary, with greater emphasis on the first 72 hours of admission to the unit, because it was identified that many of the cares on the checklist could not be fulfilled when faced with a high severity score (APACHE III). Nevertheless, as the days passed, the compliance rate improved(22). Reason why the four articles conclude that it is necessary to establish a safety culture in the organization. Because, VAP is the result of the interaction and/or omission of various factors(6).
Safety in the administration and management of medications
In June 2022, the Institute for the Safe Use of Medications (ISMP) published the report on the 10 highest-risk medication errors detected during 2021. These errors are related to: The incorrect identification of patients, omission or delay of medication, allergies or known adverse effects to medications, reconciliation of medication in care transitions, taking the patient's own medication in the hospital, verbal prescriptions, lack of use of smart infusion pumps, administration of high doses of IV paracetamol in children, similarity in name or appearance of medications, wrong IV administration of liquid oral medications(27).
However, given the wealth of interventions to respond to this problem, only three articles (25%) were found, which refer to the following topics: Education for the prevention of medication errors; preparation and administration of medications and; problems related to the prescription and dispensing of medicines.
Irajpour et al. (11)found that the implementation of an educational program aimed at various professionals and reflective critical analysis of scenarios related to medication errors, demonstrated significant changes related to medication error.
For their part, Lohmeyer et al. ((16)showed that to prevent errors in the preparation and administration of medications with similar names, the use of Tall Man Lettering (TML) in the middle or at the end of the drug name when labeling the syringes, favored more visual surveillance time and continuous verifications on the name of the drug.
Santos et al. (17)focused their activities on solving problems related to the prescription and dispensing of medicines, using as a strategy: The medication time out for the analysis of the medical prescription by the entire multiprofessional team, present in the daily rounds. The implementation of this strategy made it possible to prevent errors in the dispensing of harmful medicines.
The three articles coincide in directing all their interventions to promote sustained attention from the health professional during the writing of the therapeutics, preparation and administration of medicines. There is the possibility that organizations carry out various strategies to prevent errors in mediation, such as the use of the unit dose system or the elaboration of electronic prescriptions, but it was not possible to find these studies with significant results in the prevention of harm to the patient.
Pressure Injury Prevention
Clinical practice guidelines developed by the Pan Pacific Pressure Injury Alliance (PPPIA) , the National Pressure Injury Advisory Panel (NPIAP) and the European Pressure Ulcer Advisory Panel (EPUAP) define pressure injuries as those damages generated to the skin and/or tissues due to pressure, shearing or due to the use of medical devices or any other type(28).
The appearance of pressure injuries is a well-known problem in critical care units due to the characteristics of the patients that lead to restricted or limited mobility, use of muscle relaxants, vasopressors, fluid therapy and the demand for the use of various invasive devices that in combination can lead to the development of pressure injuries(4).
However, faced with this problem, during the search only one study with significant results was identified. The lack of more research does not allow us to provide relevant conclusions. However, it was possible to identify important actions such as: Daily injury risk assessment; observation of bony prominences; application of moisturizer all over the body and; lifting the patient from the bed during mobilization. The application of these actions had positive results in the prevention of injuries(20).
Educational program aimed at patient safety in intensive care
Eleven of the investigations (91.67%) that make up the set of results of this investigation used education as an effective tool to achieve the objectives of their study. Likewise, it was identified that two of the articles (16.67%) made use of the ISBAR method, which allows fluid, precise communication, with minimal effort and time. This method describes four stages: Identification of the situation, analysis of the circumstances, evaluation of the effects that it can generate and finally the necessary recommendations are enunciated(29). Etemadifar et al.(14)carried out five sessions of the ISBAR based program for the experimental group, obtaining valid results with respect to the frequency of event notification, the global perception of patient safety, the opening of communication channels and the exchange of information. For their part, Araujo et al.(18)found that it was necessary to involve nurses in the elaboration of the list of activities to be evaluated, thus making it easier to follow the ISBAR method. From these two investigations it can be deduced that having uniformity in the daily reports allows preventing incidents or adverse events in the care of the critically ill patient.
With the study by Amiri et al. ((10)the development of skills that promoted the empowerment of nurses such as communication, mutual support, monitoring of situations, leadership and culture of patient safety was introduced, resulting in the experimental group scored higher than the control group. In the dimensions referring to the non-punitive response to errors and reported events, no significant improvement was found. These results are similar to the study by Maldonado at al. ((30)who refer that the fear of labor reprisals or ignorance of the safety culture could generate the omission of the report. Faced with this, the authors recommend permanent education on security, allowing spaces for reflection and awareness of the problem, and promoting trust.
In the studies referring to the application of packages for the prevention of VAP(12) (15) (21)the educational workshops were the starting point for the development of interventions in the health team. These workshops were made up of training sessions and skills training. Likewise, as part of the methodology, evaluations were carried out at the patient's bedside, and when an error was identified in the observed sequence or technique, it was immediately corrected by demonstration(15). To establish knowledge or allow reminders, brochures, posters or any visual aid containing guidelines or instructions for the procedure and/or care were used(21).
It is inferred in this section that in order to establish plans, protocols, programs or clinical guidelines, it is essential to start by teaching the entire multidisciplinary team involved in direct patient care, seeking reflection during educational sessions. Additionally, the knowledge acquired during clinical practice should be monitored, in order to recognize points that were not clear or recognize new problems.
Reflections of the health team regarding safety culture
The investigations of Souza et al.(19)and Irajpour et al.(11)coincide in using reflection as a tool to understand the concept of safety and prevention of adverse events, on the part of the health team. Because, healthcare personnel, especially nurses, acquire or strengthen their knowledge by analyzing and deducing about different situations that arise in the intensive care unit, in the daily exercise of their duties. Being necessary to have scientific knowledge, experience, but above all to have the capacity for critical observation, to then lead their activities or interventions towards health promotion and damage prevention during the hospitalization period of the critically ill patient(22).
In the work of Souza et al. ((19)found that the staff demanded protocols and procedures that should be shared with the entire hospital. The work of Barreto(22)responds to this request by finding that nurses felt more secure when carrying out their activities when they consulted the service protocols. Recognizing the importance of directing efforts to promote regulations related to critical patient care. The second category in which both investigations coincide is the commitment of all professionals to comply with safety statutes. Regarding the third category: continuing education, they also agree with Irajpour et al. ((21)because they conclude that scientific domain and constant analysis of the factors that influence the clinical picture of the patient are inherent to nursing work. From the analysis of the studies, we can deduce that it is important to continue with more research that reflects reflective caring and the perceptions of nursing staff to ensure safety in care. Well, understanding their concerns or conceptions, a set of strategies and activities can be developed to solve problems related to adverse events.
CONCLUSIONS
This study contributes to comprehensively identify the various strategies developed to benefit health care safety, the most representative being those related to the prevention of ventilator-associated pneumonia and safety in medication administration. Likewise, education was identified as an effective tool to achieve the objectives of 91.67% of the investigations in this review.
However, there are still many gaps regarding infections associated with the use of catheters and tubes. Which are currently only limited to reporting knowledge about the use and care of these devices. Likewise, it is suggested that all investigations related to the prevention of infections or injuries insert the keyword: "patient safety", to visualize the importance of this topic and find new strategies that allow harm-free health care.
REFERENCIAS
1. Zárate-Grajales RA, Salcedo-Álvarez RA, Olvera-Arreola SS, Hernández-Corral S, Barrientos-Sánchez J, Pérez-López MT, et al. Eventos adversos en pacientes hospitalizados reportados por enfermería: un estudio multicéntrico en México. Enferm Univ. octubre de 2017;14(4):277-85. [ Links ]
2. Saldaña DA, Rodríguez SM, Díaz JC, Cavallo E, Grajales RZ, Tolosa RV, et al. Estudio de eventos adversos, factores y periodicidad en pacientes hospitalizados en unidades de cuidado intensivo. Enferm Glob. 2016;15(2):324-40. [ Links ]
3. Gil-Aucejo A, Martínez-Martín S, Flores-Sánchez P, Moyano-Hernández C, Sánchez-Morales P, Andrés-Martínez M, et al. Valoración de la cultura de seguridad del paciente en la UCI de un hospital de segundo nivel al finalizar la tercera oleada de COVID-19. Enferm Intensiva [Internet]. 2021; Disponible en: https://www.sciencedirect.com/science/article/pii/S1130239921001176 [ Links ]
4. Strazzieri-Pulido KC, S. González CV, Nogueira PC, Padilha KG, G. Santos VLC. Pressure injuries in critical patients: Incidence, patient-associated factors, and nursing workload. J Nurs Manag. 2019;27(2):301-10. [ Links ]
5. Reis UOP, Passos S da SS, Santos LM, Reis MS, Berhends JS, Meira CM. Erros no preparo e na administração de medicamentos intravenosos. Rev Baiana Enferm [Internet]. 2020;34. Disponible en: https://scielo.php?script=sci_arttext&pid=S2178-86502020000100340&lang=pt [ Links ]
6. Galdea MÁP, Lorena MTK, Barreto ÁG. Neumonía asociada a ventilación mecánica en pacientes ingresados en UCI: Etiología y factores de riesgo. RECIMUNDO Rev Científica Investig El Conoc. 2018;2(3):140-50. [ Links ]
7. Costa CAB, Araújo FL, Costa ACL, Corrêa A dos R, Kusahara DM, Manzo BF. Bundle de Cateter Venoso Central: conhecimento e comportamento de profissionais em Unidades de Terapia Intensiva adulto. Rev Esc Enferm USP [Internet]. 2020;54. Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0080-62342020000100472&lang=pt [ Links ]
8. Sampathkumar P. Reducing catheter-associated urinary tract infections in the ICU. Curr Opin Crit Care [Internet]. 2017;23(5). Disponible en: https://journals.lww.com/co-criticalcare/Fulltext/2017/10000/Reducing_catheter_associated_urinary_tract.4.aspx [ Links ]
9. Oliveira VMC de, Gomes CN da S, Rocha D de M, Abreu WJCP, Galvão MTG, Magalhães R de LB. Nurses' knowledge, attitudes and practices regarding hepatitis b: an integrative review. Texto Contexto - Enferm [Internet]. abril de 2022;31. Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-07072022000100504&tlng=en [ Links ]
10. Amiri M, Khademian Z, Nikandish R. The effect of nurse empowerment educational program on patient safety culture: a randomized controlled trial. BMC Med Educ. 3 de julio de 2018;18(1):158. [ Links ]
11. Irajpour A, Farzi S, Saghaei M, Ravaghi H. Effect of interprofessional education of medication safety program on the medication error of physicians and nurses in the intensive care units. J Educ Health Promot. 2019;8:196. [ Links ]
12. Madhuvu A, Endacott R, Plummer V, Morphet J. Ventilation bundle compliance in two Australian intensive care units: An observational study. Aust Crit Care Off J Confed Aust Crit Care Nurses. julio de 2021;34(4):327-32. [ Links ]
13. Branco A, Lourençone EMS, Monteiro AB, Fonseca JP, Blatt CR, Caregnato RCA. Education to prevent ventilator-associated pneumonia in intensive care unit. Rev Bras Enferm. 2020;73(6):e20190477. [ Links ]
14. Etemadifar S, Sedighi Z, Sedehi M, Masoudi R. The effect of situation, background, assessment, recommendation-based safety program on patient safety culture in intensive care unit nurses. J Educ Health Promot. 2021;10:422. [ Links ]
15. Buterakos R, Jenkins PM, Cranford J, Haake RS, Maxson M, Moon J, et al. An in-depth look at ventilator-associated pneumonia in trauma patients and efforts to increase bundle compliance, education and documentation in a surgical trauma critical care unit. Am J Infect Control. 4 de febrero de 2022;S0196-6553(22)00064-5. [ Links ]
16. Lohmeyer Q, Schiess C, Wendel Garcia PD, Petry H, Strauch E, Dietsche A, et al. Effects of tall man lettering on the visual behaviour of critical care nurses while identifying syringe drug labels: a randomised in situ simulation. BMJ Qual Saf. 8 de marzo de 2022;bmjqs-2021-014438. [ Links ]
17. Santos LL, Camerini FG, Fassarella CS, Almeida LF de, Setta DX de B, Radighieri AR. Medication time out as a strategy for patient safety: reducing medication errors. Rev Bras Enferm [Internet]. 2021;74(1). Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672021000100174&lang=pt [ Links ]
18. Araujo R de M, Almeida LF de, Paula VG de, Nepomuceno R de M, Marins ALC. Aplicabilidade do método isbar em uma unidade de terapia intensiva adulto. Cogitare Enferm [Internet]. 2020;25. Disponible en: https://scielo.php?script=sci_arttext&pid=S1414-85362020000100364&lang=pt [ Links ]
19. Souza CS de, Tomaschewski-Barlem JG, Dalmolin G de L, Silva TL, Neutzling BR da S, Zugno RM. Estratégias para o fortalecimento da cultura de segurança em unidades de terapia intensiva. Rev Enferm UERJ [Internet]. 2019;27. Disponible en: https://scielo.php?script=sci_arttext&pid=S0104-35522019000100310&lang=pt [ Links ]
20. Vasconcelos J de MB, Caliri MHL. Ações de enfermagem antes e após um protocolo de prevenção de lesões por pressão em terapia intensiva. Esc Anna Nery [Internet]. 2017;21(1). Disponible en: https://scielo.php?script=sci_arttext&pid=S1414-81452017000100201&lang=pt [ Links ]
21. Alvarez-Lerma F, Palomar-Martinez M, Sanchez-Garcia M, Martinez-Alonso M, Alvarez-Rodriguez J, Lorente L, et al. Prevention of Ventilator-Associated Pneumonia: The Multimodal Approach of the Spanish ICU "Pneumonia Zero" Program. Vol. 46, CRITICAL CARE MEDICINE. TWO COMMERCE SQ, 2001 MARKET ST, PHILADELPHIA, PA 19103 USA: LIPPINCOTT WILLIAMS & WILKINS; 2018. p. 181-8. [ Links ]
22. Barreto RS, Servo MLS, Vilela ABA, Fontoura EG, Souza S de L, Santana N. Conceptions of patient safety through the prism of social representations of intensive care nurses. Investig Educ En Enferm [Internet]. 12 de junio de 2021 [citado 17 de mayo de 2022];39(2). Disponible en: https://revistas.udea.edu.co/index.php/iee/article/view/346563 [ Links ]
23. Vásquez Gaibor AA, Reinoso Tapia SC, Lliguichuzca Calle MN, Cedeño Caballero JV. Neumonía asociada a ventilación mecánica. RECIMUNDO. 30 de septiembre de 2019;3(3):1118-39. [ Links ]
24. La higiene de manos salva vidas - OPS/OMS | Organización Panamericana de la Salud [Internet]. [citado 27 de junio de 2022]. Disponible en: https://www.paho.org/es/noticias/17-11-2021-higiene-manos-salva-vidas [ Links ]
25. Zhao T, Wu, X, Zhang, Q, Li, C, Worthington, HV, Hua F. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev [Internet]. 2020;(12). Disponible en: https://doi.org//10.1002/14651858.CD008367.pub4 [ Links ]
26. Pozuelo-Carrascosa DP, Herráiz-Adillo Á, Alvarez-Bueno C, Añón JM, Martínez-Vizcaíno V, Cavero-Redondo I. Subglottic secretion drainage for preventing ventilator-associated pneumonia: an overview of systematic reviews and an updated meta-analysis. Eur Respir Rev Off J Eur Respir Soc. 31 de marzo de 2020;29(155):190107. [ Links ]
27. Instituto para el uso seguro de los Medicamentos. Boletín 51 (junio 2022) [Internet]. [citado 15 de junio de 2022]. Disponible en: https://seguridaddelpaciente.es/es/informacion/publicaciones/2022/boletines-errores--medicacion/boletin-51/ [ Links ]
28. European Pressure Ulcer Advisory Panel [Internet]. [citado 17 de junio de 2022]. Disponible en: https://www.epuap.org/ [ Links ]
29. Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. agosto de 2018;8(8):e022202. [ Links ]
30. Maldonado XAN, Nascimento ERP do, Lazzari DD. Nursing professionals and adverse event reporting. Texto Contexto - Enferm [Internet]. 2020;29(spe). Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-07072020000600315&lang=pt [ Links ]
Received: July 24, 2023; Accepted: August 12, 2023











 text in
text in