My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.23 n.73 Murcia Jan. 2024 Epub Feb 23, 2024
https://dx.doi.org/10.6018/eglobal.571721
Reviews
Rehabilitation in the day-to-day of people with post-covid-19 neurological sequelae: scoping review
1Federal University of Santa Catarina, Florianópolis, Santa Catarina, Brazil
2Federal University of São João del-Rei, Divinópolis, Minas Gerais, Brazil
3Federal University of the State of Rio de Janeiro, Rio de Janeiro, Rio de Janeiro, Brazil
4Universidade Católica Portuguesa, Lisbon, Lisbon, Portugal
Objective:
To map available scientific evidence on rehabilitation in the daily lives of people with post-covid-19 neurological sequelae.
Methodology:
This is a scoping review according to the guidelines of the Joanna Briggs Institute. The included studies were based on the mnemonic strategy participants/ problem (adult people with neurological sequelae), concept (rehabilitation in everyday life) and context (covid-19 pandemic), with timeframe from 2020 to 2022, available in the seven selected databases, in Portuguese, English and Spanish, collected and analyzed according to PRISMA-ScR.
Results:
A total of 1,027 studies were recovered, and the sample consisted of 11 articles that presented rehabilitation programs for sequelae: fatigue, anosmia, cognitive and neuropsychological disorders. Among the main rehabilitation programs found, the following stand out: progression walking, breathing exercises; olfactory training using essential oils and cognitive approaches. From the findings, the rehabilitation process has been shown to be effective for the management of post-covid-19 neurological sequelae, and should be started early.
Conclusions:
Rehabilitation programs should involve a multidisciplinary team, since the disease presents persistent multisystemic symptoms, involving a holistic approach, which encompasses behavioral aspects related to self-care, physical rehabilitation, emotional support and health education, promoting recovery and improving the quality of life of individuals affected by the disease.
Keywords: Daily activities; Covid-19; Nursing; Pandemic; Rehabilitation
INTRODUCTION
Given the global scenario in which covid-19 has become a pandemic of great impact, it is essential to understand the implications of the disease on the central nervous system and its consequences on the daily lives of affected individuals. It is considered a multisystem syndrome because it affects several organs, manifesting symptoms and altering their physiology(1). Its clinical manifestations vary, with cardiovascular, respiratory, neuromusculoskeletal, psychological and other systemic complications, such as nutritional, hepatic, gastrointestinal, hematological, renal, endocrine and dermatological changes, which affect the functionality and quality of life of the patient(1).
The exact way that SARS-CoV-2 damages the central nervous system (CNS) is not yet well known, however, there seems to be strong evidence that occurs both hematogenously and retrograde neuronally, that is, the virus migrates to the brain through olfactory nerves, hence anosmia, causing damage to brain tissue due to hypoxia due to an exacerbated immune response(2).
Complications in the CNS may be secondary to hypoxia caused by a generalized inflammatory response(2), since SARS-CoV-2 does not directly attack brain cells; however, lack of oxygen may compromise brain physiology, causing tissue damage by interruption of blood circulation(3). Another evidence found was the presence of large amounts of microglia, brain tissue cells that have the function of monitoring the entry of foreign agents in the lower brain stem, in charge of controlling heart and lungs, and in the hippocampus, responsible for memory, justifying the possible complications reported in these organs(3).
The most frequent neurological symptoms related to covid-19 were: fatigue (85%), nonspecific cognitive complaints, reported as "brain fog" (81%), headache (68%), numbness/tingling (60%), dysgeusia (59%), anosmia (55%), myalgia (55%), dizziness (47%), pain (43%), blurred vision (30%) and tinnitus (29%), and at least 85% of patients reported at least four of these symptoms, resulting in a decline in their quality of life(4). There are also reports of cases that described neurological complications more severe than those mentioned above(5).
Since it is considered a multisystem disease, it requires the work of a multidisciplinary team for the rehabilitation of its persistent symptoms. Whenever possible, rehabilitation should begin early, still in intensive care(5). The National Institute for Health and Care Excellence (NICE) recommends that rehabilitation programs be progressive, preferably started within the first 30 days (post-acute phase) to have greater impact on patient recovery, and should be patient-centered and adapted to his/her individual needs, taking into account comorbidities that may affect progress or his/her ability to participate in a program(6). Considering the current scenario, a reflection, largely of the vaccination against covid-19, is essential to address this issue in the context of research on rehabilitation in the daily lives of people with post-covid-19 neurological sequelae.
The importance of immunization against covid-19 is crucial to prevent systemic and neurological complications caused by the virus. Vaccination has been shown to be effective in reducing disease severity, preventing hospitalizations, and protecting against SARS-CoV-2 variants. Therefore, it is essential that people are immunized according to the guidelines and recommendations of health authorities, thus suggesting the reduction in the risk of acute disease; moreover, vaccination can have a protective effect against the sequelae of the disease(7).
In this context, it is essential to understand and map the available scientific evidence on rehabilitation in the daily lives of these individuals, in order to promote effective interventions that improve their quality of life, as well as enable multidisciplinary health teams for the early rehabilitation of people with post-covid-19 neurological sequelae, in the post-acute scenario, since these professionals have fundamental skills in assessing functional needs, mental health of this population, and may contribute to the quality of life and the resumption of activities of daily life.
This study aimed to map scientific evidence for the rehabilitation in the daily lives of people with post-covid-19 neurological sequelae.
METHODOLOGY
This is a scoping review, since it aimed to map and synthesize available evidence, identifying studies that address the correlation between different variables and certain factors regarding neurological rehabilitation after covid-19(8). The guidelines of the Joanna Briggs Institute (JBI) and the recommendations of the international guidelines Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR)(9))were followed, and the research protocol was registered in the Open Science Framework (https://osf.io/7kge4/). The inclusion criteria were research articles of qualitative and quantitative approaches, experience reports, empirical and theoretical studies, official documents of national and international programs, as well as institutional guidelines on the rehabilitation of people with post-covid-19 neurological sequelae, in Portuguese, English and Spanish. Studies that were still ongoing at the time of the searches, which did not detail the neurological rehabilitation process of people with post-covid-19 neurological sequelae or that did not address neurological rehabilitation and were not freely accessible were excluded from the study.
The mnemonic strategy PCC was used to elaborate the research question: participants/problem, concept and context, integrating this scoping review studies that called as "participants", adult people with neurological sequelae; "concept" daily rehabilitation; and "context" covid-19 pandemic, reaching the starting question: "What is the scientific evidence used for the rehabilitation of adult people with covid-19 neurological sequelae?".
The search strategy was developed in three stages. In the first stage, with the help of the sectorial librarian of the Federal University of Santa Catarina, the descriptors and Boolean operators were defined, as well as the search strategy was built and the following databases were listed for the search Web of Science, Latin American and Caribbean Health Sciences Literature (LILACS), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Excerpta Medica Database (EMBASE) and, Cochrane Library. The application of the filters was also defined: full text, period from 2020 to 2022, in English, Portuguese and Spanish.
The research considered the time space from 2020 to 2022. The search in the databases occurred on January 17, 2022, with a new search made on June 15, 2022, using the descriptors selected from the section Medical Subject Headings (MeSH) and Health Sciences Descriptors (DeCS), with the Boolean operators "OR" and "AND" for their crossing. From the above, the search strategy was set up: ("Coronavirus Infections" OR "Covid-19" OR "SARS-CoV-2" OR "SARS Virus" OR "SARSCoV2" OR "SARS2" OR "covid" OR "COVID-2019" OR "COVID 2019" OR "SARS-COV-2" OR "2019-nCoV" OR "2019ncov" OR "coronavirus" OR "nCoV 2019") AND ("Neurologic Manifestations" OR "Neurologic Manifestation" OR "Neurologic Symptom" OR "Neurologic Symptoms" OR "Neurological Manifestation" OR "Neurological Manifestations" OR "Post-COVID-19 Sequelae" OR "Post-COVID-19 Syndrome" OR "Central Nervous System Diseases" OR "Anosmia" OR "Hyposmia" OR "Hyposmias" OR "Loss of Smell" OR "Smell Loss" OR "Ageusia" OR "Hypogeusia" OR "Hypogeusias" OR "Hysterical Ageusia" OR "Hysterical Ageusias" OR "Loss of Taste" OR "Taste Blindness" OR "Taste Loss" OR "Taste-Blindness") AND ("Rehabilitation" OR "Habilitation" OR "Neurological Rehabilitation" OR "Rehabilitation Services").
In the second stage, the titles of the studies were read and duplicated articles were excluded. Independently, two researchers examined the studies blindly, seeking to identify articles that corresponded to the research question, based on reading the titles and abstracts. In the third stage, the pre-selected articles were fully read independently by the researchers, and the studies that did not meet the inclusion criteria were excluded. In addition, a search was performed in the references of the selected articles to find studies that were not identified by the search strategy, in view of the specificity of the theme studied and the scarcity of published articles, considering the predefined time space. There was no need for a third investigator to reach consensus on study eligibility.
In the seven sources of information surveyed, 1,027 studies were located; 61 were excluded by duplication, leaving 966 studies for selection; of these, 674 were excluded from reading the title. Of the 292 remaining articles, after reading the title and abstract, 221 studies were excluded because they did not meet the eligibility criteria, such as: they did not address studies on the rehabilitation of people with post-covid-19 neurological sequelae and/or project studies that did not clearly present the results, leaving 71 articles for full reading. After full reading, 63 articles were excluded for not detailing the rehabilitation process of people with post-covid-19 neurological sequelae, resulting in eight articles, in these eight articles, a search was made in their references, also independently by the same two researchers, where three more articles were listed for the composition of the final sample of this review.
After full reading of the selected articles, the quality of evidence of the studies was evaluated, according to the classification developed by Evidence-Based Practice (EBP), defined as an approach that associates the best available scientific evidence with clinical experience and patient choice to assist in decision-making(10).
There are five levels for characterization of evidence strength: level 1, strong evidence of at least one systematic review of multiple well-designed and controlled randomized studies; level 2, strong evidence of at least one randomized study with appropriate design, adequate and controlled size; level 3, evidence of studies without randomization and well delineated, as a single group pre and post-cohort, time series or paired case-control; level 4, evidence of non-experimental and well-delineated studies, conducted in more than one research group or center; level 5, opinions based on clinical evidence from respected authorities, reports from expert committees or descriptive studies(10).
Data extraction was performed considering the protocol previously established and the selection flow was adapted from the recommendations of the international guide PRISMA-ScR(10). The articles included for this scoping review were organized in a synoptic chart in Microsoft Word®spreadsheet, containing the following information extracted from the selected articles: author(s)/ database/ country/ year/ level of evidence; title/ type of study/ sample (if any); sequel/rehabilitation program; main results. Both the synthesis of the extracted data and the analysis were performed descriptively, in order to gather the knowledge produced on the theme explored in the review.
RESULTS
Through the search strategy, 8 articles were identified for the final sample of this scoping review, and from the search in the references of the selected articles, 3 articles were identified that fit the eligibility criteria; thus, the final sample of the review was composed of 11 articles.
Figure 1shows the process of identification, selection, eligibility and inclusion of recovered articles:
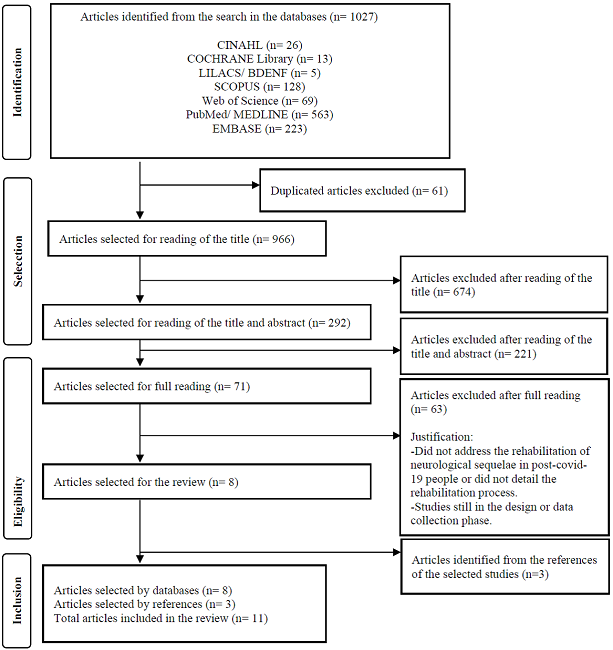
Source: created by the authors, adapted from PRISMA-ScR
Figure 1: Flowchart of the process of identification, selection, eligibility and inclusion of recovered articles. Florianópolis, SC, Brazil, 2023(9).
The most representative year, with eight articles, was 2021, and three articles from 2020. Regarding the classification according to the EBP, two articles were classified at level 2; one article at level 3; four at level 4; and five articles at level 5. The studies were conducted in the United Kingdom (n=4), United States (USA) (n=4), Brazil (n=1), Canada (n=1), and all were published in English.
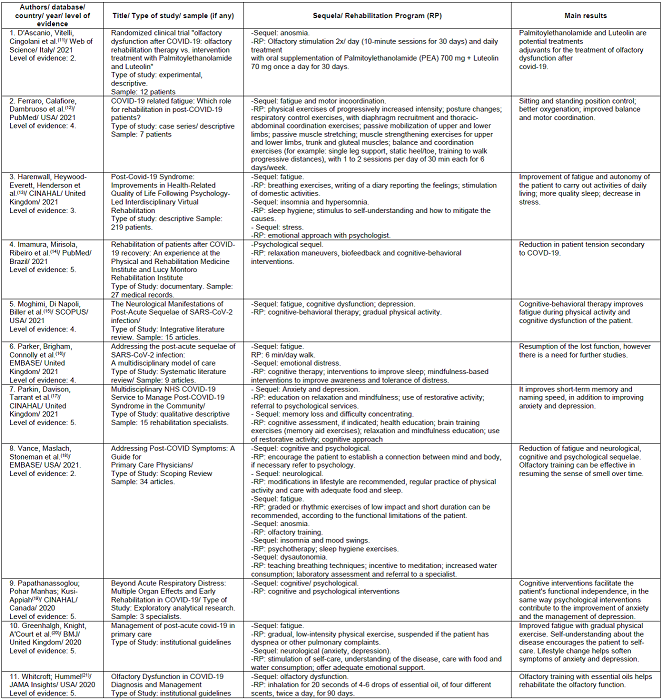
Chart 1presents a descriptive summary of the scoping review findings, containing author (s)/ database/ country/ year/ level of evidence; title/ type of study/ sample (if any); sequel/ rehabilitation program; main results:
DISCUSSION
The neurological sequelae cited in the selected studies were classified as neurocognitive, neuropsychological and olfactory disorders, in addition to fatigue, which was preponderant in most studies. Among the neurocognitive disorders, there was emphasis on insomnia/ hypersonia, change in motor coordination, memory loss, difficulty concentrating and dysautonomia. The most frequent neuropsychological disorders were psychological sequelae that fall into emotional distress, anxiety, stress, mood change and depression. Among olfactory disorders, anosmia was predominant.
In rehabilitation programs for post-covid-19 neurocognitive disorders, behavioral interventions such as Cognitive-behavioral Therapy(19,20) associated with physical exercise and mindfulness were performed to improve awareness and tolerance of suffering caused by illness(16), encouraging the patient to establish a connection between mind and body, as well as referral to psychology proved effective(18). Guidelines for sleep hygiene, stimulation of self-comprehension and self-care, and ways to mitigate the cause of the problem were effective to help with insomnia or hypersonia(13,16). For memory loss and difficulty concentrating, health education should focus on individualized and continued self-rehabilitation at home(22), through brain training exercises (auxiliary memory exercises) and relaxation activities(17). For dysautonomia, the teaching of breathing techniques, encouragement of meditation, increased water consumption, as well as laboratory evaluation and referral to the specialist are indicated(18). For motor incoordination, physical exercises of progressively increased intensity are oriented, with posture changes, associated with respiratory control exercises, with recruitment of the diaphragm and thoracic-abdominal coordination exercises; in addition to passive mobilization of upper and lower limbs; passive muscle stretching; muscle strengthening exercises of upper and lower limbs, trunk and gluteal muscles; balance and coordination exercises as unipodal support, static heels and toes, training to walk for progressive distances(12).
Rehabilitation programs for neuropsychological disorders include cognitive-behavioral therapy as an emotional support for better understanding of the process(12), being the most prevalent in the studies found(12,13,14,17), as well as the teaching of relaxation and biofeedback techniques(14). Regarding anxiety and depression, stress and emotional distress, rehabilitation programs should develop emotional interpellation with a psychologist, in order to reduce the effects of the disease on the patient’s daily life(13,16,17,18). Moreover, there should be health education about relaxation maneuvers to reduce the tension secondary to the disease(14,17). Changes in lifestyle, with a focus on self-care, such as regular physical activity, food care and adequate sleep were also reported(19,20).
For the rehabilitation of anosmia, olfactory training has been shown to be effective(18,21). The recommendation is to inhale essential oils (four different aromas), four to six drops for 20 seconds each, twice a day, for 90 days(21). In addition, oral supplement of Palmitoylethanolamide (PEA) 700 mg + Luteolin 70 mg (01 oral tablet/ day for 30 days) are potential adjuvant treatments for post-covid-19 olfactory dysfunction, when associated with olfactory rehabilitation(11).
Concerning the rehabilitation of post-covid-19 fatigue, the studies point to low-impact physical exercises with progressively increased intensity, such as: respiratory control exercises, with the recruitment of the diaphragm and thoracic-abdominal coordination exercises; passive mobilization of upper and lower limbs; passive muscle stretching; muscle strengthening exercises of upper and lower limbs, trunk and gluteal muscles and balance and coordination exercises. It is recommended one to two sessions per day, 30 minutes each, for six days a week, and these exercises should be suspended when the patient presents some alarming signal, such as dyspnea and general malaise(12,13,16,18,20).
Findings so far suggest that some symptoms of covid-19 persist even after the period of acute infection; even in patients with mild forms of the disease, one third maintain at least one of the initial symptoms after 60 days of infection(23). The results are consistent with the conclusion of the need to identify the symptoms and early intervene in order to reinsert the individual to normal life, since these symptoms have a significant impact on quality of life characterized by reduced working capacity and habitual daily activities(24).
The covid-19 pandemic created the need for rehabilitation services and their recommendations at different levels of care and health support networks. Some of them were published from an evidence-based consensus to direct medical care and rehabilitation from the survivors of covid-19, as well as lessons learned from previous epidemics(5). The British Society of Rehabilitation Medicine issued a statement highlighting the need for rehabilitation care and coordinated networks of individualized post-covid-19 care for different systems such as pulmonary, cardiac, psychological, musculoskeletal, neurorehabilitation as well as other demands(25). The Stanford Defense Medical Rehabilitation Centre, also in the UK, has developed an agreement on rehabilitation in post-covid-19 people in partnership with specialists in the areas of rehabilitation, sport and exercise medicine, reumatology, psychiatry, psychology and others, working in their rehabilitation center(5).
In the hospital setting, a study with post-covid-19 people demonstrated a significant improvement in functional independence after a multidisciplinary rehabilitation program14. In addition, rehabilitation in post-covid-19 people should be initiated still in the acute phase of the disease and even if not institutionalized, rehabilitation should be oriented to accelerate the recovery process(26).
Relying on the fact that rehabilitation is done in team and that time is crucial to avoid the loss of functionality of people with post-covid-19 sequelae, the multiprofessional and interdisciplinary look aims to establish a rehabilitation plan that mitigates the sequelae presented as a result of the disease. Thus, multidisciplinary work is an important element to improve health teams and services, since it provides opportunities for the development and involvement of the various professional categories from the discussion of ideas by different views, providing a significant improvement in the quality of care offered(27).
From the perspective of rehabilitation nursing, the nurse plays a key role in the multidisciplinary team, actively collaborating with other members, family and community, from the nursing process, aiming to achieve levels of excellence in the rehabilitation process, from its construction to execution, in addition to improving function and promoting functional independence of the person, allowing this person to live with more quality(28). Therefore, such professional has a prominent role in the promotion of actions for the prevention and treatment of the disease, as well as for health education during the processes of readaptation/ reintegration of the person, thus facilitating his/her socialization and recovery of his/her dignity and uniqueness(29).
Health education is critical to the success of any rehabilitation program. Since covid-19 is a new disease, health education around its implications and possible consequences will need to be discussed with patients(30). There is a shortage of evidence-based guidelines regarding post-covid-19 rehabilitation of people. There is, therefore, a need for more research around the theme and the long-term impact that these individuals may have, as well as the effects in health services, since rehabilitation is an essential tool in the management of complex and multisystemic post-covid-19 dysfunctions(5).
CONCLUSIONS
Existing studies show the effectiveness of rehabilitation programs for the treatment of neurological sequelae in post-covid-19 individuals, and such programs must be developed early, with a multidisciplinary approach, considering the comorbidities of the patient and the socio-environmental context in which he/she is inserted. Rehabilitation programs for post-covid-19 neurological disorders involve a holistic approach, covering behavioral, physical and emotional aspects. The combination of behavioral interventions related to self-care, emotional support, physical rehabilitation and health education is essential to promote recovery and improve the quality of life of individuals affected by the disease.
This study contributes to identify the main findings related to the rehabilitation of people with post-covid-19 neurological sequelae, providing subsidies for rehabilitation practices by multidisciplinary teams at different levels of health care. In addition, the need for more research in the field of post-covid-19 rehabilitation is highlighted, specifically in individuals with neurological sequelae.
REFERENCIAS
1. Giovannetti AS, Pereira AS, Cocentino BCB, et al. Reabilitação no contexto pós-COVID-19: Projeto Reab pós-COVID-19 (Ebook). Ministério da Saúde: Brasília, 2021. Disponível em: https://www.gov.br/saude/pt-br/coronavirus/publicacoes-tecnicas/guias-e-planos/e-book-projeto-reab-pos-covid/view. Acesso em 07 fev. 2023. [ Links ]
2. Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: A literature review. J Clin Neurosci. 2020 Jul;77:8-12. DOI: 10.1016/j.jocn.2020.05.017. [ Links ]
3. Thakur KT, Miller EH, Glendinning MD, et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain. 2021 Oct 22;144(9):2696-2708. DOI: 10.1093/brain/awab148. [ Links ]
4. Graham EL, Clark JR, Orban ZS, et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 "long haulers". Ann Clin Transl Neurol. 2021 May;8(5):1073-1085. DOI: 10.1002/acn3.51350. [ Links ]
5. Barker-Davies RM, O'Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med 2020;54:949-959. DOI: 10.1136/bjsports-2020-102596. [ Links ]
6. National Insitute for Health and Care Excellence (NICE). COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (NICE); 2020 Dec 18. PMID: 33555768. [ Links ]
7. Kuodi P, Gorelik Y, Zayyad H, et al. Association between BNT162b2 vaccination and reported incidence of post-COVID-19 symptoms: cross-sectional study 2020-21, Israel. NPJ Vaccines. 2022 Aug 26;7(1):101. DOI: 10.1038/s41541-022-00526-5. [ Links ]
8. Cordeiro L, Baldini Soares C. Revisão de escopo: potencialidades para a síntese de metodologias utilizadas em pesquisa primária qualitativa. bis [Internet]. 31º de dezembro de 2020 [citado 28º de maio de 2023];20(2):37-43. DOI: https://doi.org/10.52753/bis.2019.v20.34471. [ Links ]
9. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018 Oct 2;169(7):467-473. DOI: 10.7326/M18-0850. [ Links ]
10. Cruz DALM, Pimenta CAM. Prática baseada em evidências, aplicada ao raciocínio diagnóstico. Rev. Latino-Am. Enfermagem. 2005;13(3):415-22. DOI: https://doi.org/10.1590/S0104-11692005000300017. [ Links ]
11. D'Ascanio L, Vitelli F, Cingolani C, et al. Randomized clinical trial "olfactory dysfunction after COVID-19: olfactory rehabilitation therapy vs. intervention treatment with Palmitoylethanolamide and Luteolin": preliminary results . Eur Rev Med Pharmacol Sci. 2021 Jun;25(11):4156-4162. DOI: 10.26355/eurrev_202106_26059. [ Links ]
12. Ferraro F, Calafiore D, Dambruoso F, et al. COVID-19 related fatigue: Which role for rehabilitation in post-COVID-19 patients? A case series. J Med Virol. 2021 Apr;93(4):1896-1899. DOI: 10.1002/jmv.26717. [ Links ]
13. Harenwall S, Heywood-Everett S, Henderson R, et al. Post-Covid-19 Syndrome: Improvements in Health-Related Quality of Life Following Psychology-Led Interdisciplinary Virtual Rehabilitation. J Prim Care Community Health. 2021 Jan-Dec;12:21501319211067674. DOI: 10.1177/21501319211067674. [ Links ]
14. Imamura M, Mirisola AR, Ribeiro FQ, et al. Rehabilitation of patients after COVID-19 recovery: An experience at the Physical and Rehabilitation Medicine Institute and Lucy Montoro Rehabilitation Institute. Clinics (Sao Paulo). 2021 Jun 14;76:e2804. DOI: 10.6061/clinics/2021/e2804. [ Links ]
15. Moghimi N, Di Napoli M, Biller J, et al. The Neurological Manifestations of Post-Acute Sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021 Jun 28;21(9):44. DOI: 10.1007/s11910-021-01130-1. [ Links ]
16. Parker AM, Brigham E, Connolly B, et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. Lancet Respir Med. 2021 Nov;9(11):1328-1341. DOI: 10.1016/S2213-2600(21)00385-4. [ Links ]
17. Parkin A, Davison J, Tarrant R, et al. A Multidisciplinary NHS COVID-19 Service to Manage Post-COVID-19 Syndrome in the Community. J Prim Care Community Health. 2021 Jan-Dec;12:21501327211010994. DOI: 10.1177/21501327211010994. [ Links ]
18. Vance H, Maslach A, Stoneman E, et al. Addressing Post-COVID Symptoms: A Guide for Primary Care Physicians. J Am Board Fam Med. 2021 Nov-Dec;34(6):1229-1242. doi: 10.3122/jabfm.2021.06.210254. [ Links ]
19. Papathanassoglou E, Pohar Manhas K, Kusi-Appiah E. Beyond Acute Respiratory Distress: Multiple Organ Effects and Early Rehabilitation in COVID-19. Connect: The World of Critical Care Nursing, Volume 13, Number 4, 2020, 155-161. DOI: 10.1891/WFCCN-D-20-00008. [ Links ]
20. Greenhalgh T, Knight M, A'Court C, et al. Management of post-acute covid-19 in primary care. BMJ. 2020 Aug 11;370:m3026. DOI: 10.1136/bmj.m3026. [ Links ]
21. Whitcroft KL, Hummel T. Olfactory Dysfunction in COVID-19: Diagnosis and Management. JAMA. 2020 Jun 23;323(24):2512-2514. DOI: 10.1001/jama.2020.8391. [ Links ]
22. Piquet V, Luczak C, Seiler F, et al. Do Patients With COVID-19 Benefit from Rehabilitation? Functional Outcomes of the First 100 Patients in a COVID-19 Rehabilitation Unit. Arch Phys Med Rehabil. 2021 Jun;102(6):1067-1074. DOI: 10.1016/j.apmr.2021.01.069. [ Links ]
23. Fraser E. Long term respiratory complications of covid-19. BMJ. 2020 Aug 3;370:m3001. DOI: 10.1136/bmj.m3001. [ Links ]
24. Twomey R, DeMars J, Franklin K, et al. Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Phys Ther. 2022 Apr 1;102(4):pzac005. doi: 10.1093/ptj/pzac005 [ Links ]
25. Phillips M, Turner-Stokes L, Wade D, et al. Rehabilitation in the wake of Covid-19 - A phoenix from the ashes. British Society of Rehabilitation Medicine, 2020. Disponível em: https://www.bsrm.org.uk/downloads/covid-19bsrmissue1-published-27-4-2020.pdf. Acesso em: 27 mai. 2023. [ Links ]
26. Ceravolo MG, de Sire A, Andrenelli E, et al. Systematic rapid "living" review on rehabilitation needs due to COVID-19: update to March 31st, 2020. Eur J Phys Rehabil Med. 2020 Jun;56(3):347-353. DOI: 10.23736/S1973-9087.20.06329-7 [ Links ]
27. Marques JB, Aprígio DP, Mello HLS, et al. Contribuições da equipe multiprofissional de saúde no programa saúde da família (PSF): uma atualização da literatura. Rev Baiana Saúde Pública 2007; 31(2):246-255. Disponível em: http://files.bvs.br/upload/S/0100-0233/2007/v31n2/a248-257.pdf. Acesso em 25 mai. 2023. [ Links ]
28. Lima AMN, Ferreira MSM, Martins MMFP da S, et al. (2019). Influência dos cuidados de enfermagem de reabilitação na recuperação da independência funcional do paciente. Journal Health NPEPS, 2019; 4(2), 28-43. Acesso em: https://periodicos.unemat.br/index.php/jhnpeps/article/view/4062. Acesso em: 26 mai. 2023. [ Links ]
29. Associação Portuguesa dos Enfermeiros de Reabilitação (APER). Contributos para o Plano Nacional de Saúde 2011-2016. Porto; 2010. [ Links ]
30. Chinese Association of Rehabilitation Medicine; Respiratory Rehabilitation Committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary Rehabilitation Group of Chinese Society of Physical Medicine and Rehabilitation. [Recommendations for respiratory rehabilitation of coronavirus disease 2019 in adult]. Zhonghua Jie He He Hu Xi Za Zhi. 2020 Apr 12;43(4):308-314. Chinese. DOI: 10.3760/cma.j.cn112147-20200228-00206. [ Links ]
Received: May 28, 2023; Accepted: August 12, 2023











 text in
text in