My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
On-line version ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 n.1 Jan./Feb. 2006
ORAL MEDICINE AND PATHOLOGY
Granulomatous facial reaction to injected cosmetic fillers
A presentation of five cases
Rafael Poveda 1, José V. Bagán 2, Judith Murillo 3, Yolanda Jiménez 1
(1) Médico Estomatólogo. Adjunto del Servicio de Estomatología
(2) Catedrático de Medicina Bucal, Universidad de Valencia. Jefe del Servicio de Estomatología.
Hospital General Universitario de Valencia.
(3) Cirujana Maxilofacial. Adjunta del Servicio de Estomatología del Hospital general Universitario de Valencia
ABSTRACT
The use of substances to augment soft tissues as aesthetic purpose is associated with, among other undesirable effects, the appearance of foreign body granulomas. The improvements made to these substances have reduced the incidence of adverse reactions, but not eliminated them. We present five cases of foreign body reactions to three different products, dimethylpolysiloxane (silicone), bovine collagen, and polylactic acid, which were injected into the subcutaneous cellular tissue of the patients (all five were women), between two and sixteen years before the appearance of the foreign body reaction. All five presented painless, diffuse facial tumefaction, of firm, elastic consistency. The magnetic resonance image (MRI) studies showed signs of intense inflammatory reaction in the affected
areas.
The histology revealed the presence of foreign body granulomas with giant multi-nucleated cells.
The patients were treated with systemically administered corticoids, except in one case which did not require pharmacological treatment.
Key words: Granuloma, siliconoma, polylactic acid, silicone, bovine collagen.
RESUMEN
El uso de sustancias para el aumento de tejidos
blandos por motivos estéticos puede ocasionar la aparición de granulomas a
cuerpo extraño, entre otros efectos indeseables. Las mejoras introducidas en
dichas sustancias han conseguido la disminución de la incidencia de reacciones
adversas pero no su desaparición. Presentamos cinco casos de reacción a cuerpo
extraño por tres productos diferentes, dimetilpolisiloxano (silicona), colágeno
bovino, y ácido poliláctico, que habían sido infiltrados en el tejido celular
subcutáneo de las pacientes (las cinco eran mujeres) entre dos y dieciséis años
antes de la aparición de la reacción a cuerpo extraño. Las cinco presentaron
un cuadro de tumefacción facial difusa, no dolorosa y de consistencia duroelástica.
Los estudios de imagen con resonancia magnética mostraron signos de reacción
inflamatoria intensa de la zona afectada.
La histología mostró la presencia de granulomas a cuerpo extraño con células
gigantes multinucleadas.
Las pacientes fueron tratadas con corticoides administrados por vía sistémica,
excepto una de ellas que no precisó tratamiento farmacológico.
Palabras clave: Granuloma, siliconoma, ácido poliláctico, silicona, colágeno bovino.
Introduction
The use of filler substances to augment soft tissues dates back to the end of the 19th century. Initially autologous fat was used, later paraffin, silicone, and bovine collagen, with a long, and ever increasing list of products to the present day (1). The mechanism is similar in all types: these are supposedly inert materials that on being introduced into the integument cause an increase in the volume per se and a progressive infiltration of a collagen matrix which in turn contributes to the increase in volume (2).
Liquid silicone is derived from dimethylsiloxane polymers. It is administered following the microdrop injection technique described by Orentreich (3).
Bovine collagen is the substance most used at present, and constitutes the standard reference for the remaining filler materials. Multiple presentations of the product have been tried (associated to polymetacrylate spheres, to solubilized elastin peptides, in monomolecular form at 2% in aqueous solution, etc.).
Polylactic acid is a non-animal product presented in a lyophilized (freeze-dried) form and requires reconstitution with water before it is injected (1).
The use of these products is associated with certain undesirable effects, foreign body reactions being the particular interest of this article.
Clinical cases
Case 1
Fifty-five year-old woman, smoker of two packets of cigarettes a day, and occasional consumer of alcohol. Insulin dependent diabetes and with a stomach ulcer. Under treatment with insulin, citalopram, lorazepam, calcium dobesilate, raloxifene and atorvastatin.
She was referred to our service presenting a tumefaction on the lower part of both genian areas, the left lower lip and the right nasogenian sulcus of one months evolution, slow progressively growing, elastic in consistency, and painless (fig. 1). The patient noted that she felt worse in the mornings. She reported how she had received first local infiltrations of polylactic acid and then botulinum toxin typeA (Botox®) nine years, and one and a half years ago respectively. A blood analysis, orthopantomograph, MRI and a biopsy were requested. The analysis and the orthopantomograph did not reveal any significant alterations. The MRI showed hyperintense images of the mandibular and submandibular subcutaneous fat with discrete trabeculation related to inflammatory changes. The biopsy informed of chronic inflammatory infiltrate with eosinophiles and foreign body (silicone) giant cells situated in the submucosa and fascicles of striated muscle. Treatment was initiated with deflazacort 15 mg per day for 10 days and then gradually reducing the dosage until withdrawing it completely one month and ten days later. The patient noticed a clear improvement although bilateral tumefactions of firm consistency persisted on palpation.
Case 2
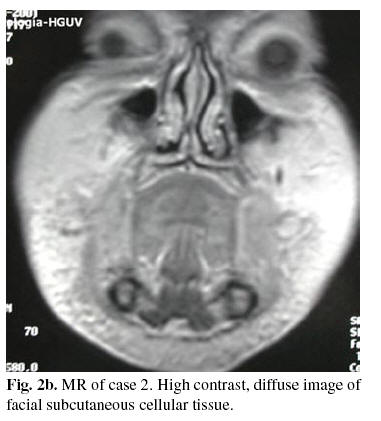
Female 72 years old, non-smoker nor consumer of alcohol and with no clinical history of interest attended our service presenting, since eight days previously, a firm, diffuse, facial tumefaction, poorly defined although more marked on the lips and the chin, with no adenopathies nor alteration in the general state of health (fig. 2a).
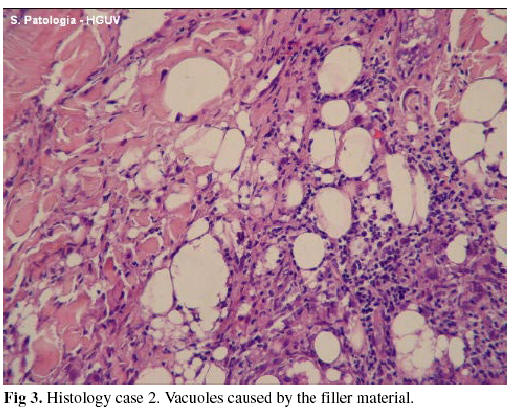
The patient informed that 16 years earlier she had undergone treatment with injections of dimethylpolysiloxane (silicone) in the lips, cheeks and chin. A blood analysis, orthopantomograph, FNAB, MRI and biopsy were requested. The first three provided no data of any help in the diagnosis. The MRI revealed an intense inflammatory process affecting almost the entire subcutaneous cellular tissue covering the maxillae and the floor of the mouth and also a large part of the buccal mucosa (fig.2b). The involvement was diffuse and with an extensive contrast. The biopsy showed a lesion compatible with a silicone-induced foreign body granuloma (fig. 3).
Treatment commenced with deflazacort 30 mg/day, reduced to 15 and 7.5 at three and two days respectively. One month later the patient noticed a worsening of the condition so treatment with deflazacort 30 mg/day was reinstated. Three months later, the tumefaction persisted and so treatment continued with 7.5 mg/day of deflazacort. Ten months later, the medication was withdrawn. The patient had no problems, but the firmness remained in the infiltrated areas.
Case 3
70 year-old woman, occasional smoker and consumer of alcohol, with a history of arthrosis, cataracts, detached retina and depression. She came to our service presenting a generalized, bilateral, facial tumefaction which did not remit with antibiotic treatment (fig. 4). Two years previously she had undergone treatment with facial collagen infiltrations in the upper lip. The patient told how a previous outbreak a year earlier had resulted in the extraction of a molar tooth. An orthopantomograph was requested and a biopsy taken. The radiography showed no signs of any interest. The biopsy revealed discrete perivascular lymphoid infiltrates together with a focus of steatonecrosis and giant multinucleated cells of a type associated with a foreign body reaction. The final diagnosis was infiltration by bovine collagen. Treatment commenced with Deflazacort 30 mg/day. A gradual improvement of the symptoms occurred over the next two weeks. The medication was withdrawn and two weeks later a new outbreak occurred in the right mandibular area that required renewed corticoid treatment until its resolution 10 days later.
Case 4
A 54-year-old woman with a history of osteoporosis, polyps and breast cancer. Under treatment with ossein-hydroxyapatite (Osteopor®), extract of melilotus officinalis (Esberiven®) and a homeopathic preparation for allergy (Lymphomyosot®). She was referred by her dentist, because of the appearance, 15 days earlier, of a swelling of the lips and cheeks that had varied in intensity and location, sometimes being noticed more on one side than on the other. The patient was worried that it might be an oral metastasis of breast cancer. Twelve years previously she had received silicon infiltrations in the upper nasolabial folds. A tumefaction of firm consistency was present in both jugal mucosa up to the retrocommissural area. A blood analysis was requested the results of which were normal, and a biopsy was taken which confirmed a silicone-induced foreign body reaction. Given the improvement in the patient it was decided not to initiate any treatment and to carry out periodic revisions.
Case 5
A forty-three year-old woman with no previous illness of interest who had received silicon injections in the lips and cheeks 10 years before. At 2-3 years of the infiltrations her face began to swell for which she received anti-inflammatory treatment. Given that the treatment was ineffective she underwent surgery to remove the foreign body. As a result of the surgery the patient was left with a facial paralysis without resolving the swelling. When she came to service the patient related continuous episodes of inflammation that required permanent treatment with corticoids (deflazacort) which had caused an increase of 5kg in weight. On physical examination the patient presented labial and buccal mucosa tumefaction above all on the right side, firm in consistency. A biopsy was taken which revealed a silicone-induced foreign body reaction.
Discussion
The clinical and epidemiological characteristics of the cases presented in this study are summarised in Table 1.
Independently of the filler material used in each case, the mechanism and the end result are the same. The injected product induces a reaction in the surrounding conjunctive tissue with the more or less stable deposition of collagen that persists independently of whether the filler material is phagocytized or not (2). In short, an increase in the volume of the soft tissues is produced, which is the desired effect.
The supposed innocuousness of these products (they were considered inert initially) was put rapidly into doubt on observing adverse reactions directly related with their use. Given that silicone was the first material used on a large scale, and with little sanitary control, it is responsible for the majority, and the most virulent, of the adverse reactions described (4). It should be noted, however, that adverse reactions have been described to practically all the products used, and, of course, with the three materials implicated in this study (5).
Although the possible systemic toxicity of some of these products, in particular silicone, has been suggested, deposits being detected in the liver, spleen and kidneys following subcutaneous injection, the fact is that it has not been possible to establish a relationship with diseases of the conjunctive tissue, nor with other diseases (6, 7). Neither has it been possible to detect anti-silicone antibodies (8).
Local toxic effects include pain, edema, ecchymosis, erythema, dyschromia, alterations in cutaneous texture, overcorrection, and local embolic phenomena (3). In some, fortunately rare, cases extensive ulcers can be produced that can affect muscle,bone and nervous structures (9, 10).
The granulomatous foreign body reaction appears after a variable period (2, 9, 10, 12 and 16 years in the cases presented) and from 5 months to 15 years in the literature reviewed (11).
The mechanism remains unknown, although it has been suggested that an infection could set off an immunological cross-reaction (12) or that retarded immunity stimulation may occur (13).
The clinical symptoms include tumefaction normally solid, although other manifestations such as flare, burning sensation, pain and sensitivity to touch, which do not appear in the cases presented here, have been described (11).
The histology is characterized by giant multi-nucleated cells as a foreign body reaction. Vacuoles corresponding to the filler material are frequently found, particularly with silicone. With other products the filler material may not be detected (2).
The differential diagnosis should include erysipelas, allergic contact dermatitis, facial edema with eosinophilia, cheilitis glandularis apostematosa, Aschers syndrome, orofacial granulomatosis, Crohns disease, Melkersson-Rosenthal syndrome or sarcoidosis (11.14). Likewise, cutaneous leishmaniasis, leprosy or tuberculosis can also present as a granulomatous inflammation of the skin (13).
The etiological treatment (removal of the injected substance) presents problems that are still difficult to resolve at present. For the symptomatic treatment, systemic, local corticoids (12), minocycline (15) and imiquimod at 5% (16) have been described. Our cases were treated with systemic corticoids during the outbreaks since it was considered that the filler material could not be removed surgically.
![]() Correspondence
Correspondence
Rafael Poveda Roda
Hospital General Universitario de Valencia
Av/ Tres Cruces s/n
46.014 Valencia
E-mail: poveda_raf@gva.es
Received: 30-03-2004
Accepted: 25-03-2005
References
1. Klein A, Elson M. The history of substances for soft tissue augmentation. Dermatol Surg 2000;26:1096-105 [ Links ]
2. Lemperle G, Morhenn V, Charrier U. Human histology and persistence of various inject able filler substance for soft tissue augmentation. Aesthetic Plast Surg 2003;27:554-66. [ Links ]
3. Orentreich D. Liquid injectable silicone. Clin Plast Surg 2000;27:595-612. [ Links ]
4. Allevato MA, Pastorale EP, Zamboni M, Kerdel F, Woscoff A. Complications following industrial liquid silicone injection. Int J Dermatol 1996;35:193-5. [ Links ]
5. Lombardi T, Samson J, Plantier F, Husson C, Kuffer R. Orofacial granulomas after injection of cosmetic fillers. Histopathologic and clinical study of 11 cases. J Oral Pathol Med 2004;33:115-20. [ Links ]
6. Sanchez-Guerrero J, Colditz G, Karlson E, Hunter D, Speizer F, Liang M. Silicone breast implants and the risk of connective tissue diseases and symptoms. N Eng J Med 1995;332:1666-70. [ Links ]
7.Gabriel S, OFallon M, Kurlan L, Beard CM, Woods JE, Melton LJ. Risk of connective-tissue diseases and other disorders after breast implantation. N Eng J Med 1994;330:1697-702. [ Links ]
8.Oliver DW, Walker MS, Walters AE, Chatrath P, Lamberti BGH. Antisilicone antibodies and silicone containing breast implants. Br J Plast Surg 2000; 53:410-4. [ Links ]
9.Rapaport M, Vinnik C, Zarem H. Injentable silicone: cause of facial nodules, cellulitis, ulceration and migration. Aesth Plat Surg 1996;20:267-76 [ Links ]
10.Mastruserio N, Pesqueira M, Cobb M. Severe granulomatous reaction and facial ulceration occurring after subcutaneous silicone injection. J Am Acad Dermatol 1996;34:849-52 [ Links ]
11.Ficarra G, Mosqueda-Taylor A, Carlos R. Silicone granuloma of the facial tissues: A report of seven cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:65-73. [ Links ]
12.Bigatà X, Ribera M, Bielsa I, Ferrándiz C. Adverse granulomatous reaction after cosmetic dermal silicones injection. Dermatol Surg 2001;27:198-200. [ Links ]
13.Maas C, Papel I, Greene D, Stoker D. Complications of Injectable Synthetic Polymers in Facial Augmentation. Dermatol Surg 1997;23:871-7. [ Links ]
14.Yanagihara M, Fujii T, Wakamatu N, Ishizaki H, Takehara T, Nawate K. Silicone granuloma on the entry points of acupuncture, venopuncture and surgical needles. J Cutan Pathol 2000;27:301-5. [ Links ]
15.Senent P, Bachelez H, Ollivaud L, Vignon-Pennamen D, Dubertret L. Minocycline for the treatment of cutaneous silicone granulomas. Br J Dermatol 1999;140:985-7 [ Links ]
16.Baumann L, Halem M. Lip silicone granulomatous foreign body reaction treated with Aldara (Imiquimod 5%). Dermatol Surg 2003;29:429-32. [ Links ]











 text in
text in