My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Pharmacy Practice (Granada)
On-line version ISSN 1886-3655Print version ISSN 1885-642X
Pharmacy Pract (Granada) vol.4 n.2 Redondela Apr./Jun. 2006
|
Original research |
Reducing the use of benzodiazepines and cyclopyrrolones in clinical practice
Reducir el uso de benzodiazepinas y ciclopirrolonas en práctica clínica
Viggo Rask Kragh JØRGENSEN, Birgit Signora TOFT, Max
van Soest FOGH.
|
ABSTRACT Objective: Recently, the use of benzodiazepines (BZD) and cyclopyrrolones
(CP) has drawn a great deal of attention. About 100,000 patients - approximately
2% of the Danish population - are believed to be addicted to BZD. This
article describes a simple and effective method of reducing the use of
dependency-producing drugs in clinical practice. Key words: Benzodiazepines. Cyclopyrrolones. Substance-related disorders. Adverse effects. Denmark. |
RESUMEN Objetivo: Recientemente, el uso de benzodiazepinas (BZD) y ciclopirrolonas
(CP) ha absorbido gran atención. Unos 100.000 pacientes aproximadamente
el 2% de la población danesa- se cree que son adictos a las BZD.
Este artículo describe un método simple y efectivo para
reducir el uso de medicamentos productores de dependencia en la práctica
clínica. Palabras clave: Benzodiazepinas. Ciclopirrolonas. Alteraciones relativas a substancias. Efectos adversos. Dinamarca. |
Viggo Rask Kragh JØRGENSEN, Specialist in General Practice. General Practitioner.
Medical Advisor. Medicinenheden Ringkjøbing Amt. Denmark.
Birgit Signora TOFT. Pharmacist, PhD. Medical Advisor. Medicinenheden Ringkjøbing
Amt. Denmark.
Max van Soest FOGH. Specialist in General Practice. General Practitioner. Denmark.
INTRODUCTION
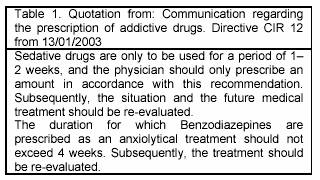
The use of benzodiazepines (BD) in Denmark has decreased slightly during recent years, whereas the use of cyclopyrrolones (CP) has shown an increase during the same period.1 Accordingly, the accumulated use of both drugs decreased by a mere 1-2 percent in 2003. The prescription of dependency-producing drugs in Denmark is regulated according to Danish directive CIR nr 12 13/012003 (table 1).
There are about 100.000 people addicted to BD in Denmark, comprising approximately 2 percent of the population.2 This is one of the reasons why the use of these dependency-producing drugs has drawn a great deal of political attention during recent years. In 2003, Minister of the Interior and Public Health, Lars Lykke Rasmussen, gave physicians a 1-2 year deadline to "get their prescription patterns in order". Failing this, it was warned that sanctions such as increased supervision or the implementation of other restrictions may be initiated. However, the subsequent decrease in the use of both drugs in 2004 is estimated at only 1.7 percent, far from the official Danish objective of a 50 percent reduction.3
Over the past five years, it has been the aim of Ringkøbing Amt (County) to reduce the prescription of dependence-producing drugs. Different initiatives have been implemented, including lectures, educational sessions and group supervision, as well as counselling by a General Practitioner and supervision under the guidance of specialists in this particular field of medicine. In addition to these initiatives, the regional Medical Officer of Health has intensified the process of identifying physicians having patients with a large turnover of dependence-producing drugs.4 The physicians in question have been asked to explain how they intend to reduce their use of dependence-producing drugs. The total reduction in the use of BD and CP in Ringkjøbing County as a result of these joint efforts was approximately 4 percent between 2003 and 2004. The various initiatives outlined above have undoubtedly contributed to maintaining focus on the problem, and have paved the way towards further initiatives, one of which is presented in this article.
The attention given to the use of BD and CP is justified, due to a number of serious side effects associated with the use of these drugs (table 2).5,6 Pseudodementia and an increased tendency to imbalance can occur among elderly patients. Paradoxal side effects such as anxiety, hallucinations and violent behaviour have been reported in isolated cases. Besides the direct effect of the drugs they are addictive with both physical and psychological symptom. Tolerance to these drugs may arise readily. When reducing dosages, the original symptoms these drugs were intended to cure may return in full force the so-called rebound effect.
The hypnotic effect of these drugs decreases after only a few weeks and the anxiolytic effect disappears within a few months. Only the side effects remain if the drugs are taken away. After a few months treatment there will be no positive effect of the drugs.
From the first of January 2004, two General Practice clinics situated in the town of Thyborøn in Western Jutland initiated schemes to reduce the use of dependence-producing drugs, in order to meet the demands of Danish directive CIR nr 12 13/012003. (table 1). By publishing the results of these efforts, we hope to inspire other colleagues to reduce their use of BD and CP through the implementation of simple methods.
METHODS
Data originates from two General Practice clinics in Thyborøn, covering some 2300 patients. In close collaboration with Ringkjøbing Amt, both clinics implemented the regulations set out in Danish directive CIR nr 12 13/012003. Due to geographical considerations, two thirds of the patients where initially included, and by January 1st 2005 all patients were included in the study. Treatments included the benzodiazepines N05BA (anxiolytica) and N05CD (hypnotica drugs), as well as the cyclopyrrolone N05CF (hypnotica). The internet site of the Institute for Rational Pharmacotherapy (IRF; www.Ordiprax.dk) was used for evaluation, due to ease of access and a high degree of coverage and precision. The material compiled by the IRF originates from data reported to the Danish Board of Health covering the whole prescription drugs sold by pharmacies. For each prescription handled by the pharmacy, the prescribing physician's personal code, the patients' national registration number as well as the specific code regarding the drug in question was registered. This product-specific code contains information covering the anatomical therapeutic chemical (ATC)-code, package size and total amount of Daily Defined Doses (DDD) in the package.
A patient's guide, as well as a guide for medical staff was prepared, in order
to support the study of the applied interventions. The procedures implemented
by the physician were as follows:
No prescriptions were to be effected by telephone.
Prescriptions were only to be renewed by the physician following a personal
consultation.
Prescriptions were to be prescribed for 1 month at a time.
The subsequent use of dependence-producing drugs was evaluated and resulted in either the continuation of existing prescription patterns, or the introduction of a drug-reducing regime. The local press was informed about the intervention. This led to articles printed in the local newspaper in December 2003 and December 2004, explaining the reason and scope of the intervention.
Inclusion criteria: All patients receiving BD or CP (with the sole exception of patients suffering from a severe physical or psychiatric disorder) were included. The term severe physical disorder covered patients suffering from a terminal disease, or other diseases being monitored by a special ward only. Severe psychiatric disorders covered patients whose treatment was being monitored exclusively by a psychiatrist. Patients receiving high doses, as well as patients with prior failed drug reduction histories were not automatically excluded, unless they otherwise fulfilled the criteria of exclusion. The treatment of patients excluded from this study continued as before. The Public Health Department in Ringkjøbing Amt fully accepted the increase in consultations arising from this study.
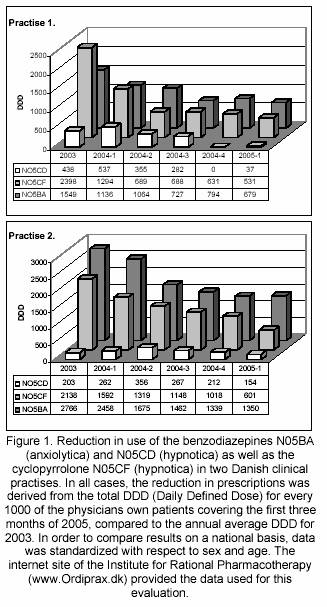
In all cases, the reduction in prescriptions was derived from the total DDD (Daily Defined Dose) for every 1000 of the physicians own patients covering the first three months of 2005, compared to the annual average DDD for 2003. Accordingly, the decline was registered over a 15-month period. In order to compare our results on a national basis, data was standardized with respect to sex and age.
RESULTS
The reduction in prescription of the anxiolytica N05BA in percentage in the two clinics was 56,4% and 51,4%, respectively. The initial level of prescription in clinic 2 was nearly 80% higher than in clinic 1. The highest reduction rate observed in the first three-month period of 2004 was in clinic 1, and amounted to 26%.
The use of hypnotics belonging to the BD group (N05CD) was nearly eliminated in clinic 1 (figure 1). In clinic 2, only two patients remained after the first three-month period of 2005 - both suffering from a severe physical disorder. This material is, however, too limited to have any statistical significance.
The use of the hypnotica N05CF, belonging to the CP group was reduced by 77.8% in clinic 1. The highest reduction rates were seen within the first six months of intervention. The corresponding reduction in clinic 2 was 71.8%. The reduction was more evenly distributed during the entire 15-month period of intervention.
The additional workload as a result of the intervention was initially approximately 4-5 weekly consultations for every 1000 patients. Subsequently, the number of additional consultations fell to three weekly consultations for every 1000 patients. After the first few consultations, an agreement was reached with the patient regarding subsequent prescription of the drug. The estimated loss of patients to other clinics in the area as a direct consequence of the project was 1-2 patients pr. 1000. The strain on the Primary Healthcare was not increased as a consequence of the project. Only one patient was referred to a psychiatrist, and in only a single case was the regional Outpatient Department contacted as a direct result of the intervention. Addiction treatment by hospitals or special units for addiction treatment proved unnecessary. No serious side effects were recorded, and the side effects recorded were anxiety, restlessness and sleeping disorders. No suicidal behaviour was registered by either of the two physicians. There was no need for therapeutic sessions, and no official complaints were recorded. In the opinion of both of the involved physicians, fewer detrimental effects of the intervention where observed than where expected.
DISCUSSION
While hypnotics from the BD group were never frequently used by either of the two clinics, prescription rates regarding hypnotics from the CP group were close to being among the top 25 % of all clinics in Ringkjøbing Amt in 2003.
It is the general belief of both physicians that healthy people should not use these drugs for extended periods. This view is shared by the National Board of Health (table 1). However, prior to this study no tangible actions to implement this view had been initiated. Among physicians, a resigned attitude concerning the implementation of drug-reducing regimes as a part of the physician's daily routine is common. Many General Practitioners believe that reductions in the use of dependence-producing drugs are nearly impossible, requiring specialist involvement, and that the situation is aggravated by the patients' perceived lack of motivation.
It is clear that in order for a physician to initiate a drug reducing regime, specific knowledge is required. While a comprehensive psychotherapeutically education is unnecessary, a sufficient knowledge of this topic can easily be acquired by most General Practitioners within a few hours by reading the basic literature.5-7 It is the opinion of the authors that the real obstacle hampering the solution of this problem are the physicians' own prejudices. By simply changing this attitude a major hurdle in eliminating this problem will be removed.
During the course of this study, staff-patient contact proved to be quite successful, as a result of working according to written instructions. Lengthy and tedious negotiations with patients were thus avoided. Patient reactions were essentially positive, with only a few being discontent and unable to understand why they should attend monthly consultations.
These monthly consultations exposed a whole group of patients, who previously had been invisible to the physician. Surprisingly, the majority of these patients were positive with respect to their involvement in a drug-reducing regime, and seemed well aware of the addiction problem as well as their lack the ability to deal with it on their own.
It is estimated that close to 100.000 patients are addicted to BD in Denmark.2 A problem of this magnitude cannot be dealt with by specialists only within a reasonable period. Inevitably, the patients own General Practitioner will have to assume the responsibility for solving this issue.
In the primary phase of the intervention, additional consultations amounted to 4-5 consultations for every 1000 patients, dropping to about 3 consultations after 15 months of intervention, despite the fact that the total number of patients increased significantly due to the geographical considerations mentioned earlier. A further decrease in consultations is expected as a result of the reduction of drug doses being prescribed. In order to allow comparison with the rest of the country, the Thyborøn results were standardized with respect to sex and age using the Institute for Rational Pharmacotherapy (IRF) data. The validity of the IRF data depends on the degree of precision linked to the entire prescription process - from the physician to the actual handling of the prescription by the pharmacy. The most common error is that of the physicians' registration number being incorrect, and this error occurs in some 4% of the data recorded. However, a bias at this level will not change the outcome of this study, or affect the general message.
In the field of General Practise, it is customary to inform colleagues when prescribing drugs during periods of vacancy. By implementing monthly consultations, we intended to eliminate the need for this precaution. Few prescriptions were ever received from neighbour clinics. Prescriptions issued to non-regional patients are not recorded by the Ordiprax system. Thus, we cannot eliminate the possibility of patients involved in this study receiving a prescription elsewhere. We believe, however, that the extent to which this may have occurred is minimal. The experiences drawn from this study clearly indicate the importance of a personal consultation on a monthly basis. By maintaining this strategy, most patients will be motivated to start a drug-reducing regime within a few months.
CONCLUSIONS
The authors believe that the results obtained here can easily be achieved in any other clinic, due to the simplicity of the procedures involved and the lack of time-absorbing educational requirements. Accordingly, the personal resources and time required to implement this strategy can easily fit into the every day life of any clinic. The procedures for reducing levels of BD and CP use include the cessation of BD and CP prescriptions being effected by telephone, as well as the requirement for a personal consultation on a monthly basis prior to the renewal of prescriptions. This simple recommendation will encourage the physician as well as the patient to consider whether the existing prescription pattern is to continue, or whether a drug-reducing regime should be initiated.
ACKNOWLEDGEMENTS
The authors thank Doctor Hans Holmsgaard, Thyborøn, for his cooperation and for letting us make use of his personal data. We also wish to thank the Medical Officer of Health Børge Sommer for his guidance and inspiration.
|
References |
1. Lægemiddelstyrelsen. Institut for Rationel Farmakoterapi. Juni 2005.http://www.ordiprax.dk [ Links ]
2. Hansen EH Helweg-Jørgensen S. Afhængighed af psykofarmaka set fra brugernes side.Danmarks farmaceutiske universitet. Lægemiddelforskning 1999. http://www.dfuni.dk/index.php/laegemiddelforskning_1999/1208/0/ [ Links ]
3. Methling I. Lægerne får kort frist til at bremse op. Politiken 2003, 31 december. [ Links ]
4. Sommer B. Benzodiazepiner i almen praksis. Månedskr prakt Lægegern. 2005.1385-90. [ Links ]
5. Ashton CH. Benzodiazepines: How they work and how to withdraw. The Ashton manual, Aug.2002. http://www.benzo.org.uk. [ Links ]
6. Lægemiddelstyrelsen. Institut for Rationel Farmakoterapi. Benzodiazepiner i almen praksis. September 2004, 1.udgave. [ Links ]
7. Ashton CH. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs 1994;48(1):25-40. [ Links ]











 text in
text in