INTRODUCTION. TELEMEDICINE, TELE-HEALTH AND E-HEALTH
Telemedicine consists of the exchange of health information between healthcare professionals and between healthcare professionals and patients through the use of information and communications technologies (ICT).
There are several definitions in the civilian and military setting, but all of them meaning the above concept1-3.
Nowadays, it is considered in its etymological definition, as «the practice of medicine over a distance…» or «the delivery of health care services, where distance is a critical factor…»4,5.
There are two major fields in telemedicine: the exchange of information between health care professionals (e.g. primary physician with specialists, nurse with physician, etc.) and between the health care professional and the patient. In Europe, especially in the military, the first field is the most common. The second needs much more technology because the number of patients potentially using telemedicine is huge, so millions of wearables to record patients vitals are necessary, and strong organization is needed, including artificial intelligence systems to process and analyze the billions of data points that the wearables send so that only the useful ones are received by the health care workers and algorithms to determine where the data goes, who receives it, and when it should be received.
Tele-health is a much wider concept than telemedicine, dealing not only with the exchange of information for clinical use (diagnosis, treatment, etc.) but also for «patient and professional health-related education, public health and health administration»6,7.
When it comes to telemedicine, reality usually goes in front of legality. Thus, although there are a lot of people already using this technology, ethical documents of both international and national medical organizations5,8,9 recommend its use only in specific circumstances for some cases during the clinical process and with specific requirements and legislation and guidelines and standards, most of which are still lacking.
E-health would be considered the widest concept and is defined as «in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterizes not only a technical development, but also a state-of-mind, a way of thinking, an attitude, and a commitment for networked, global thinking, to improve health care locally, regionally, and worldwide by using information and communication technology»10.
WHERE IS TELEMEDICINE AS A TECHNOLOGY?
Gartner, a leading research and advisory company in the U.S., has developed what it is called the Hyper Cycle of Emergent Technologies11 that «provides a graphic representation of the maturity and adoption of technologies and applications.» (Fig. 1)
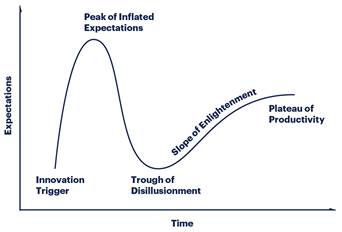
Figure 1. Hype Cycle of Emergent Technologies. Available at: https://www.gartner.com/en/research/methodologies/gartner-hype-cycle.
This Hype Cycle establishes five phases of a technology’s life:
«Innovation Trigger: The first phase of the cycle is the «launch», the presentation of the product or any other event that generates interest, presence and impact on the media. At this stage there are rarely usable products and commercial viability is not proven..
Peak of Inflated Expectations: At this stage the impact on the media usually generates unreasonable enthusiasm and expectations about the possibilities of technology. Some pioneering experiences may be successful, but there are usually more failures.
Trough of Disillusionment: Expectations are not met, because they are delayed, etc. Interest is being diluted and some investors are starting to fall. After the advertising boom of the second phase some technologies are no longer in vogue and, consequently, the media usually forget about them.
Slope of Enlightenment: Although the media have already no interest in the technology, some companies continue testing to understand the benefits that technology can provide and explore new practical applications. Some technologies begin to crystal lize the benefits they can bring and begin to be widely understood. Technologies are improved with 2nd and 3rd generation products and services.
Plateau of Productivity: A technology reaches the «productivity plateau» when its benefits are widely demonstrated and accepted. Finally, the criteria for determining commercial viability begins to become clear. The mass adoption of technology is beginning to become a reality. Technology is starting to provide benefits.» When we look at Digital Health Gartner’s Hyper cycle, we find that Tele-health is already considered to be in the «Plateau of Productivity»12. (Fig. 2)
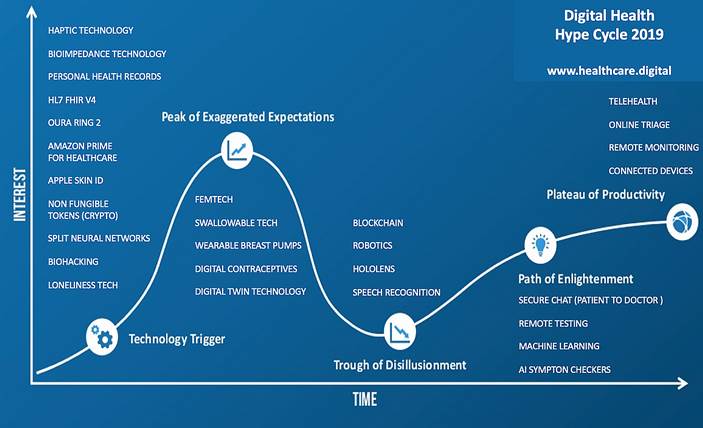
Figure 2. Gartner’s Digital Health Hyper cycle. Available at: https://www.healthcare.digital/single-post/2019/01/12/The-Digital-Health-Hype-Cycle-2019.
So, world-wide, it is considered a well-established technology, but that is not what we see, at least in Europe. Why? Maybe because it is growing as an exponential technology does.
TELEMEDICINE AS AN EXPONENTIAL TECHNOLOGY
Ray Kurzweil, a famous American inventor and futurist, says that «the future is widely misunderstood. Our forebears expected it to be pretty much like their present, which had been pretty much like their past. The rapid growth of technology is actually accelerating progress across a host of domains. This has led to unexpected degrees of technological and social change occurring not only between generations, but within them»13.
Related to this is the concept of exponential growth of some technologies. What does exponential growth mean?
Most likely, telemedicine is an exponential growth technology. These technologies have a curious type of growth, compared with the classic linear technologies, perfectly described by different authors14. (Fig. 3)
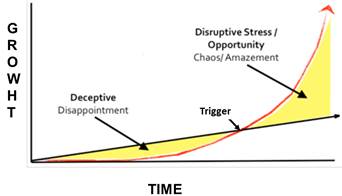
Figure 3. Exponential Disruption Rob Nail, CEO, Singularity at AAI16 by BootstrapLabs. Available at: https://www.youtube.com/watch?v=SGBLcvAGWAM
At first, they grow even slower than linear technologies, which is deceptive and creates a feeling of disappointment, but, at some point, there is a trigger that accelerates this growth like an explosion, thus making it exponential. But, what will be the trigger induces exponential growth for Telemedicine?
Probably it will be a combination of different things: cheap and comfortable wearables (like stickers or decals that children use) for the patients to send their vitals, improved communications technology (5G), artificial intelligence systems to analyze all the information sent, a complex and automatized organization of the system of telemedicine, etc.
HISTORICAL BACKGROUND OF SPANISH MILITARY TELEMEDICINE
The use of telemedicine in Spain started in the 1930s when Military Medical Officers on Navy Ships used the radio to send teleconsultations to the Navy Hospitals back in Spain that were answered by the Emergency Physicians on duty, who gave remote support with the means available at that time (radio)15.
In 1996, the «Gómez Ulla» Military Hospital Telemedicine Unit was founded during Hospital Centennial Celebration (and Tandberg Vision videoconference equipment was implemented). It was immediately used in Operations (at that time in Former Yugoslavia’s conflict) and, since then, has always been used in all the Operations were Spain has deployed personnel.
PRESENT OF THE SPANISH MILITARY TELEMEDICINE
Our main mission is remote health support to health professionals or military personnel deployed in Operations19-21, and remote22 or difficult-to-access locations23.
From the Reference Center at the Telemedicine Unit in the Central Defense Hospital «Gómez Ulla» we give remote health support to what we call «Remote Nodes» from the Army, Air Force, Navy, Guardia Civil Navy Ships, Civilian Naval Hospitals, Civilian Hospitals and NGO Hospitals.
Our main strength is to have all medical and surgical specialists of the hospital available to give remote support 24/7, which contributes to the Hospital mission as a Role 4 for Operations.
As any other Hospital Unit/Department we perform other tasks, apart from the clinical (remote) assistance, such as24:
Training personnel using Telemedicine Equipment in the Operational Theatre, connection for Clinical Sessions between hospitals, Smart Operating RoomTelemedicine Unit connection for surgery students/ residents/ nurses training, etc.
R &D: New equipment/ devices for the tactical environment.
Consulting: National / International (ESA, NATO) Working Groups.
Other: support to Military Medical Legal Assessment Boards and Military Justice Courts (declaration of Medical Experts in Trials).
Organization
One of the main needs when starting a Telemedicine System is organization (more than equipment, personnel or communications). So, before implementing the system, it is necessary to answer some questions, which could be called the Five Ws of a Telemedicine System:
Who is going to exchange information (only health care professionals, patients and health care professionals)?
Which ICT (information and communications technology) is going to be used to transmit the information (terrestrial lines or wireless; optic fiber or 5G; a combination)?
What kind of information is going to be transmitted (e-consultation, videoconference, patient registers, such as vitals and images including ultrasound)?
When will the exchange of information happen (in real time or synchronous, delayed or asynchronous, or both?
Why are you going to use Telemedicine (better diagnosis/ treatment, evaluate the need for evacuation/ transfer the patient, follow up)?
In the Spanish Military Telemedicine System, this organization is established25 so that any Remote Node (Medical Units in the Operational Theatre, Military or Civilians Ships, even military personnel) can reach our Telemedicine Unit through a 24/7 mobile phone/ e-mail. Most importantly, this call/ e-mail is received by Military Health Care Personnel (Military Nurse) in the Telemedicine Unit.
Our experience dictates that the teleconsultation usually needs some kind of management which must be done by Military Health Care personnel and not simply by a Call Center (for example, the specialist required to give remote support).
When the Alert Telemedicine Officer (as we call the Military Nurse Officer that receives and answers this e-mail/ call) receives the request of a teleconsultation, they get in touch with the specialist required to give remote support, sometimes answering by e-mail (e-consultation) or, if videoconference or additional tests (like tele-otoscopy, teleultrasound, etc.) are needed, they meet at the Reference Centre in the Telemedicine Unit. The 24/7 availability of the medical/ surgical specialist is guaranteed by the personnel on duty at the Central Defense Hospital and the command´s order that this hospital is the Role 4 or Higher Echelon for the Operations.
SPANISH MILITARY TELEMEDICINE CAPABILITIES
The capabilities are a key point when talking about Telemedicine. Telemedicine is frequently confused with videoconference, but telemedicine has many other capabilities that Spanish Miliary Telemedicine has used for a long time :
Vital Signs and EKG transmission (in Real Time = RT). A patient can be monitored and his/ her vitals (heart rate, respiratory rate, temperature, pulse oximetry, and the most important, EKG) sent and received at that moment, what is called «in real time» at the Reference Centre, so the specialist can study them and give better medical remote support.
External Exam Camera images transmission (RT). The deployed Telemedicine equipment has a high-resolution external camera that sends dynamic imaging but also allows freezing the image to increase resolution (for example, of a suspicious lesion in the oral cavity).
Cold Light Source images transmission: tele-otoscope, tele-ophthalmoscope and tele-dermatoscope: (RT). With these medical instruments connected to the equipment, otoscopy, ophthalmoscopy and dermatoscopy images obtained from the patient can also be sent in real time to help the specialist give remote support. Tele-Ultrasound (RT). Ultrasound is a widely used technology and very useful for diagnostic and therapeutic procedures. The remote operator needs some basic training, but with the so called Dual Video Technology (diagnostic ultrasound image and an image of the hand of the remote operator with the probe on the screen at the same time), and what we call «Agreed Language for tele-ultrasound26», the radiologist (or other specialist with ultrasound skills like a cardiologist27, urologist, etc.) is able to guide the remote operator to move the probe to get the needed image for ultrasound diagnosis. (Fig. 4)

Figure 4 Agreed language for TeleUltrasound (Hernandez-Abadía, A., Molina, P. et al, not published).
Surgical Tele-Mentoring (RT)28,29. Some years ago, we started to use this technology. It consists of obtaining a surgical field image in the operating room at the remote site projected on monitors both in the remote operating room and in the Reference Center of the Telemedicine Unit in Role 4, so that both (usually junior) surgical personnel at the remote site and experienced/ senior surgeons in the Hospital can watch it. Then, senior surgeons at the Role 4 use what we call the Surgical Tele-assistant. This system allows the drawings of the senior surgeons to be seen over the surgical field image and permits them to point specific areas of the surgical field image to highlight some key structure (such as a vessel, nerve, etc.) or aspect of the field. (Fig. 5)
SPANISH MILITARY TELEMEDICINE EQUIPMENT
The equipment used for telemedicine in Spain has different electro-medical devices that get different records from the patient (from vital signs to EKG, ultrasound image, ophthalmoscopy, otoscopy or dermatoscopy images, etc) and a CIS system able to send them in real time to the Medical Treatment Facility (Role) that is going to give remote health support. (Fig. 6)
SPANISH MILITARY TELEMEDICINE COMMUNICATIONS
As our mission is remote health support to health professionals or military personnel deployed in Operations and remote/difficult-to-access locations all over the world, our main communication is by Satellite, civilian or military, depending of the coverage in the area where teleconsultation is needed.
This is one of the big differences with civilian telemedicine, where optic fiber (or soon 5G or a combination of both) can be used with much more bandwidth (our system is very efficient, as we work usually with so very low bandwidth as 100-200 Kbps).
SPANISH MILITARY TELEMEDICINE FUTURE: RESEARCH AND DEVELOPMENT
There are several areas in which we have already done or are currently doing research:
Sensors (wearables): A project called e-Safe Tag30 was developed to send information from wearables (Instant Applicable Plaster Sensor) to portable devices to help in casualty classification and care in the field. Our vision about wearables is that if they are part of the soldier´s armor, there is a risk that they are damaged (by explosions or shrapnel, etc.) or mal-function due to blood, so they would be better carried (and put on the casualty) by the military health personnel at the point of injury as soon as they approach to the patient. (Fig. 7)
Portable Telemedicine Devices: Today, the technology permits using portable equipment to practice telemedicine with all the capabilities mentioned above. They are small backpacks or suitcases that include all the electro-medical devices needed to obtain images or records from the patient and a CIS component able to send them to the hospital in real time. As far as we know, there are not many on the market:
QOREHEALTH-SCHILLER Portable Solution (tactical backpacks, rugged portable cases and dufflebags)
TEMPUS PRO (PHILIPS).
SAFETRIAGE PRO (RDT)
We have tested two: QOREHEALTH-SCHILLER (QHS) Portable Solution in tactical exercises with Spanish Signal Battalion Regimiento de Transmisiones n.1 and TEMPUS PRO (TP) from the Antarctica Spanish Base connected to our hospital, Spanish Role 4. (Fig. 8)

Figure 8. Portable telemedicine devices. A) Available at: Qorhealth-Schiller: Qorehealth Product Catalog 2020 (not published). B) TEMPUS PRO: https://www.philips.co.uk/healthcare/product/HC989706000051/tempus-pro-rugged-advanced-monitor.
The conclusions of these preliminary tests are:
Both models allow us to practice telemedicine in tactical situations
QHS Portable Solution needs a greater bandwidth while the TP is able to work in a limited scenario of 32-64 Kbps which makes it really efficient considering the austere combat environment in which this equipment is going to be used.
Tempus Pro is less versatile, as it works in the mentioned 32-64 Kbps fixed bandwidth scenario, while QH can work in multiple telecommunications scenarios.
QHS is able to send images from several devices simultaneously, can send large files and has the capability to chat in degraded link conditions. The Tempus Pro can only send one image at a time, so if you carry out a medical test, it stops the communication and only restarts when the test is complete and can be sent. Also, TP can only send small files (QS can send much bigger ones) and you do not have a chat capability (QS has), so if the link malfunctions only audio is available for teleconsultations.
Augmented Reality Glasses: These ultra-portable devices used in Telemedicine allow remote military health care person nel to send images and sound and very importantly, receive (in a small screen in the glasses) remote support from the Medical Treatment Facilities on the field (Roles in the military terminology) or in the country (Central Hospital of Defense or Role 4). (Fig 9)

Figure 9. Augmented reality glasses. A) Available at: https://www.androidcentral.com/epson-moverio-bt-200-smart-glasses-now-available. B) Available at: https://www.bhphotovideo.com/explora/mobile/news/sony-smarteyeglass. c) Available at: https://blog.capterra.com/3-things-field-service-can-teach-any-mobile-workforce/
Our test in the field with various models (Sony, Epson, Fujitsu) ended with two basic conclusions:
They could be perfect in the tactical field for Special Operation Units, where there is always a shortage of personnel and material.
The moment to use them would be in the TFC or TACEVAC phases of the TCCC31 always after initial emergency care of the casualty has been completed (when health care personnel can pay attention to the instructions of a remote health support).
Telemedicine in the evacuation platforms: (armored ambulances, rotary or fix wing): This is another of our main R&D lines because receiving remote support from the specialists at Role 2/3 in the Operational Theatre or in Role 4 is an advantage to the medical personnel who travel with the casualty during tactical or strategic medevac. Some test have been done here in Spain, but we need to continue testing with fix wing used for strategic medevac (equipped with satellite communications) and the much more complicated and challenging scenario of rotary wing in the Operational Theatre.
Tele-Microbiology32: A microscopic field image was sent from a microscope in our Role 2 in Herat (Afghanistan) by just connecting a camera to the microscope and sending the image as any other through the «Telemedicine Tower», making it available on a monitor for all the Microbiology Department in the Role 4/ «Gómez Ulla» Hospital to evaluate in real time the patient’s blood prepared at the remote site. (Fig 10)
Robotic Tele-ultrasound: Some years ago, the Spanish Telemedicine Unit worked in an ESA project33 that tested this system for astronauts to be evaluated by ultrasounds from Earth. A robotic arm is placed over the astronaut and the Radiologist performs the ultrasound and makes a diagnosis from the image at the same time by moving the probe of the US equipment with a joystick. This technology was tested in Spanish Role 2 deployed in Afghanistan34.
Telemedicine integration with Military Health Information Systems and Electronic Health Records. We are currently working to integrate all the information with our Operational HIS, Cendala.
Tele-ICU: Leveraging the classic concept of «centralized or remotely-based critical care team networked with the bedside ICU team and patient via state-of-the-art audiovisual communication and computer systems»35,36, our systems gives our ICU specialist control over the remote electro-medical equipment of the critical care patient at some Medical Treatment Facilities, for example, on board Hospital of Spain’s Juan Carlos I Navy Ship. Tele-endoscopy: Any image taken with a fiberscope of any internal cavity could be sent in real time. We have tested this capability in laryngoscopy37 and bronchoscopy from the Operational Theater (Afganistan Spanish Role 2 at Herat) with good results and even using the previously mentioned tele-assistant.
Telemedicine and COVID 19: Due to the COVID 19 pandemic, the relationship between health professionals and patients has changed. There is an explosive rise in the use of Telemedicine in healthcare, as for the pandemic it can be useful not only for indi-vidual medical aspects (diagnosis, treatment, aftercare, etc.) but also public health aspects (early outbreaks detection, avoiding the spread of infection, helping social distance measures, saving personal protection equipment, etc.38. Due to the SARS CoV-2 pandemic, all health care facilities are implementing new strategies in the field of Telemedicine. Telemedicine/ Tele-health can be also useful for the exchange of information between experts to contain the pandemic, tele-mentoring of health personnel or patients, prescribe medications…
In the other hand, it can also be very useful for the diagnosis, treatment and follow-up of patients with other diseases that have their access to health care limited or delayed because of the pandemic, specially those with chronic diseases with the use of wearables or sensors.
CONCLUSION
The Spanish Military Telemedicine System is pioneer in this field in Spain. Today it works 24/7 to give remote health support to military personnel deployed in Operations and remote or difficult to access locations. The strength of the system is the availability of all medical/ surgical specialists at the Central Defense Hospital «Gómez Ulla» in Madrid to give remote health support based on being the Higher Health Support Echelon to Operations or Role 4. In addition to e-consultation and videoconference teleconsultation, it has other capabilities (transmission of vitals, ECG, images of otoscopy, ophthalmoscopy, dermatoscopy, tele-ultrasound and surgical tele-mentoring, all of them synchronous/ in real time).
The future of the system will include improved equipment (portable telemedicine devices, augmented reality glasses, sensors/ wearables) that will move Military Telemedicine to the point of injury, broaden its use (in evacuation platforms, tele-Microscopy, tele-Endoscopy, etc) and integration with Health Information Systems and Electronic Health Records for more complete remote support in diagnosis and treatment.


















