My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Osteoporosis y Metabolismo Mineral
On-line version ISSN 2173-2345Print version ISSN 1889-836X
Rev Osteoporos Metab Miner vol.10 n.1 Madrid Jan./Mar. 2018 Epub Apr 03, 2023
https://dx.doi.org/10.4321/s1889-836x2018000100005
Originals
Prevention and early diagnosis of childhood osteoporosis: are we doing the right thing?
1Unidad de Reumatología Pediátrica - Servicio de Pediatría - Hospital Universitario Son Espases - Palma de Mallorca (España)
2 Sección de Reumatología Pediátrica - Unidad de Gestión Clínica de Pediatría - Hospital Regional Universitario de Málaga - Málaga (España).
3 Unidad de Reumatología Pediátrica - Hospital Universitario y Politécnico La Fe - Valencia (España)
4 Servicio de Reumatología - Estructura Organizativa de Gestión Integrada (EOXI) - Complejo Hospitalario Universitario de A Coruña - A Coruña (España)
5 Unidad de Gestión Clínica de Pediatría - Hospital Universitario San Cecilio - Granada (España)
6 Servicio de Reumatología - Hospital Santa Creu i Sant Pau - Barcelona (España)
7 Unidad de Reumatología Pediátrica - Hospital Sant Joan de Déu - Esplugues de Llobregat - Barcelona (España)
8Grupo de Investigación en Litiasis Renal y Biomineralización - Instituto de Investigación Sanitaria de la Universidad de las Islas Baleares (IUNICS) - Palma de Mallorca (España)
9 Departamento de Pediatría y Farmacología - Facultad de Medicina - Universidad de Málaga - Málaga (España)
Objectives:
To assess prevention, early diagnosis and training received regarding osteoporosis among the pediatrics professionals in our area.
Material and methods:
Survey directed to physicians of pediatricians of Primary Care (PC) and Specialized Care (SC) in order to evaluate their activity in prevention, detection and training received in osteoporosis. The survey was disseminated through the relevant scientific societies.
Results:
420 pediatricians participated (324 from PC and 96 from SC). 93.5% of PC pediatricians and 89.6% of SC pediatricians valued the physical activity of the patients; 85.19% and 35.4% of them, respectively, the intake of dairy products. 45.68% of PC and 70.2% of SC recommended calcium and vitamin D supplements in the case of low nutritional intake, whereas 39.2% of PC and 47.2% of SC favored follow-up. 39.6% of SC pediatricians requested bone densitometry for this disease or risk treatment, and 47.9% measured the levels of 25-OH-vitamin D. 25.93% of PC and 45.3% of SC asked about the existence of fractures, 90.4% and 96.8% requested etiopathogenic mechanism. 40% of PC and 86.2% of SC requested a bone densitometry or referred to the specialist for fractures due to low trauma energy, with specific criteria in 13.7% and 5.86%, respectively. 92% of PC and 82.3% of SC had not received recent training in childhood osteoporosis.
Introduction
Bone mass increases during childhood and adolescence until it reaches its maximum value shortly after puberty 1,2. Several factors are involved in this process among which the genetic load determines up to 80% while the remaining 20% depends on modifiable external factors, such as nutrition, exercise and exposure to sunlight and osteotoxic substances, among others 3 4-5. The optimization of all of them is essential to achieve the maximum bone mass at the end of development 6.
Children suffering from chronic conditions usually have difficulties reaching an optimal peak of bone mass. In general, they present a higher incidence of malnutrition, practice less physical exercise and are less exposed to solar radiation because of their disease 7. In addition, the inflammatory activity present in some diseases inhibits bone formation and stimulates its reabsorption, as in the case of some medication treatments (especially glucocorticoids) 8.
Several studies indicate that the best way to prevent adult osteoporosis is to favor optimal bone mass peak acquisition at the end of the growth stage 910-11. Thus, controlling bone mineralization during childhood is an unavoidable obligation for pediatricians, who must promote healthy living habits in their patients, minimize osteotoxic medication use and recognize warning signs to make an early diagnosis if there is bone metabolism disorder.
Our study aimed to evaluate preventive activity and early diagnosis of osteoporosis that is currently carried out, as well as the training received in this field, by primary care (PC) pediatricians and hospital pediatricians who care for children with chronic diseases in our country.
Material and methods
Two online surveys were prepared, one for PC sector pediatricians and the other for pediatricians in specialized care (SC). These surveys collected data on prevention, detection and treatment of children at risk of osteoporosis in routine clinical practice. It also queried them about the training received about this condition.
The surveys were designed using Google Docs technology and disseminated through different scientific societies between November 2014 and October 2015. In addition, in order for the survey to reach the maximum number of physicians, recipients were urged to forward the questionnaire to their pediatric colleagues working in this area. Each participant was sent both surveys indicating that they had to answer one or the other whether they were working in PC or SC activity. A descriptive study of our obtained data was carried out. The results were expressed as percentages. Statistical analysis was carried out using the SPSS v21 package.
Since the surveys did not include patient data and were anonymous and voluntary, ethics committee approval was not required. However, the study was reported to the committee coordinating center, which accepted the approach. The researchers were the only ones who had access to the survey data, which were collected exclusively for statistical purposes.
Results
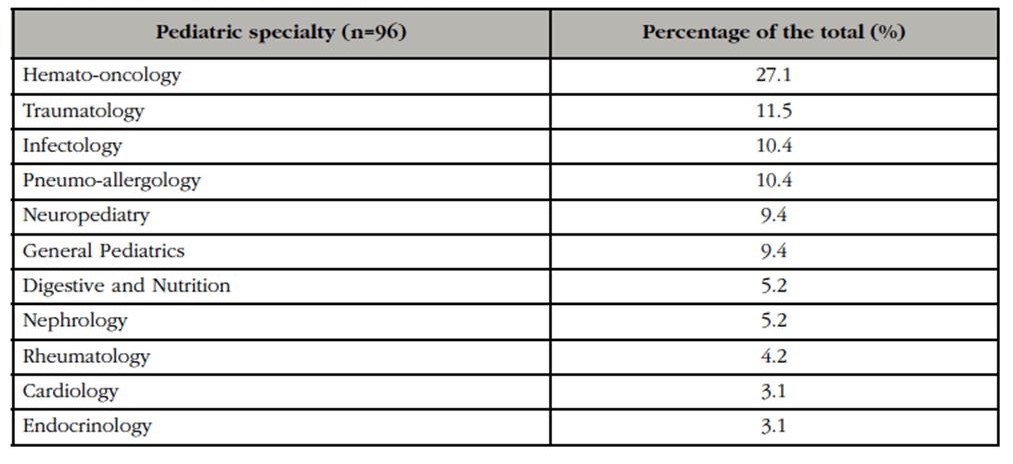
In all, 420 professionals participated in the survey, 324 PC pediatricians and 96 from different pediatric specialties. The pediatric specialty of those surveyed in the hospital setting is shown in Table 1.
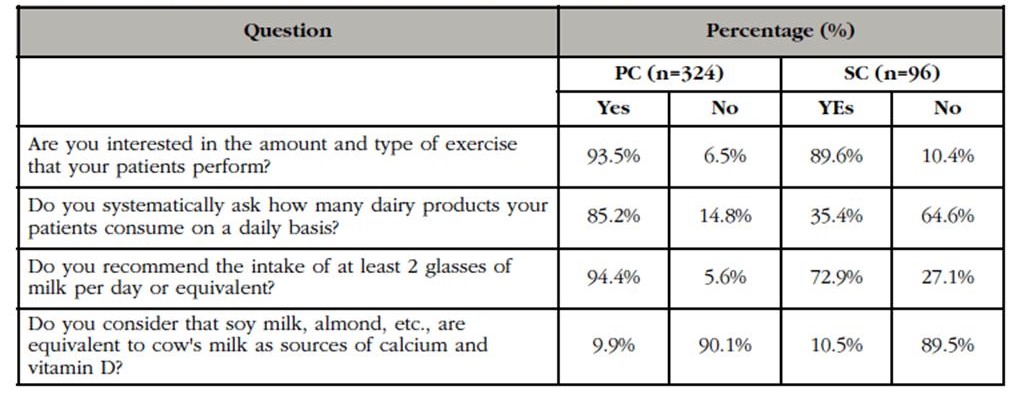
Regarding preventive habits assessment, 93.5% of PC pediatricians and 89.6% of SC reported assessing the patients’ amount and type of physical exercise and concerning daily intake of dairy products, 85.2% and 35.4%, respectively. The detailed results are shown in Table 2. Regarding preventive treatment, 45.68% of primary and 70.2% of specialized pediatricians referred to calcium and vitamin D supplements to patients with low nutritional intake of these elements. Complementary test follow-up in the patients who received a supplement was carried out by 39.2% of the PC and 47.2% of the SC.
Table 2 Evaluation of the preventive habits of childhood osteoporosis in the Child Health Program (PC) and in the chronic patient consultation (SC). (n=420 completed surveys)
Regarding the detection of patients with risk of osteoporosis in PC, only 25.93% of professionals asked specifically about fractures within the child health program. 90.43% reported assessing the etiopathogenic mechanism and 40% recognized that SC should be referred to patients with fractures due to low-energy trauma. 94.2% admitted not having specific referral criteria in the presence of osteoporosis (Table 3).
Table 3 Early detection and referral of PC patients. (n=324 completed surveys)

CHP: Children's Health Program.
As for managing chronic SC patients, 39.6% reported requesting a dual-energy densitometry (DXA) in case of prolonged corticotherapy or chronic disease that affected the bone although there were no fractures, and 49.7% did not monitor 25-OH-vitamin D levels in patients with risk factors. 86.2% requested DXA or referred to rheumatology or endocrinology for fractures due to commonplace injuries. 13.7% admitted having specific referral criteria in the presence of osteoporosis (Table 4).
In reference to the training received, 92% of PC pediatricians and 82.3% of those of SC had not received training in childhood osteoporosis in the last 5 years, and 88.27% and 79.8%, respectively, considered it insufficient.
Discussion
This is the first reported study of similar characteristics both nationally and throughout European. Our important finding is the great variability of prevention regarding childhood osteoporosis in our environment and the limited training in pediatrics.
The promotion of bone health in the pediatric age is the best strategy for reducing fracture risk and physical disability in old age 12. The need for osteoporosis prevention programs has been analyzed in different publications on behavior and knowledge in the adult population, although few have been effective 13. At the school level, programs aimed at improving children’s health are carried out, but these interventions are more effective when they come from the health personnel of reference 13. Therefore, it is the pediatrician who must identify children and adolescents at risk of presenting or developing low bone mass in order to apply appropriate preventive and therapeutic measures to prevent their progression and the appearance of fragility fractures 13.
The main measures for osteoporosis prevention in childhood are adequate daily intake of calcium and promotion of physical exercise, especially those forms that involve weight bearing 14. Other beneficial measures include the control of body weight, regular sun exposure and avoiding tobacco and alcohol 14. Adolescence is the time of greatest bone mass acquisition, so the presence of unhealthy lifestyle habits (low physical activity, decreased intake of dairy products, tobacco, alcohol, etc., relatively frequent at this stage of life) has a very negative impact on its final peak 15. Therefore, adolescents are the main risk group and the population on which prevention measures should focus, especially on women because of their greater risk of developing osteoporosis in adulthood 13. So pediatricians should explore patients’ living habits and correct those aspects that are harmful to the proper skeletal development in children and adolescents. In our study, most primary care pediatricians reported being interested in their patients’ physical activity and dairy intake and reported making specific recommendations to optimize these aspects.
In the case of children with chronic conditions, it is even more important to favor bone mass acquisition by promoting healthy lifestyles. These patients have a special risk of developing osteoporosis in adulthood, since any chronic systemic disorder can influence bone mineral density: nephropathies, metabolic, hematological, endocrinological, gastrointestinal and rheumatological diseases 16 17-18. However, in our study, although more than 80% of pediatric hospital specialists were interested in their patients’ physical activity, only 34.5% asked about the intake of dairy products as a matter of course.
The appearance of low impact fractures (resulting from bone fragility) means a significant decrease in bone mineral density, and appears in established phases of the disease 1 2-3. Therefore, the active search for children at risk is important, including in the medical history of child health programs, the assessment of the fractures they present and the monitoring of calcium and vitamin D levels. In our study, the low percentage stands out of pediatricians of PC that include in the case history the number and characteristics of the fractures of the child referred to SC for low impact fractures. On the other hand, more than half of SC pediatricians do not monitor vitamin D levels or bone mineral density in the chronic risk patient, although most assess the etiopathogenic mechanism and report the reference units of their center.
As for calcium supplements, multiple studies restrict their use to individuals with insufficient contributions through diet, not supporting systematic supplementation neither in healthy children nor with osteoporosis if they have an adequate contribution 19 20 21-22. Similarly, there are no data that allow us to systematically recommend supplementation with vitamin D 23,24. However, calcium and/or vitamin D supplements are recommended when the contribution of these elements is low at baseline. Adequate levels of vitamin D3 (25-OH Vitamin D) in childhood are between 20 and 30 ng/ml (75-50 nmol/l), although recent studies place optimal levels above 30 ng/ml. ml (75 nmol/l) 27,28. The recommended daily amount of vitamin D3 and calcium is shown in table 5. In the case of vitamin D, we can measure its plasma levels (25-OH vitamin D), while the calcium intake should be estimated by means of a dietary survey. In our study, only half of the PC pediatricians and 86% of SC referred to calcium and vitamin D supplements in these situations. Such supplementation implies the need to control plasma levels and to detect possible complications, such as hypercalciuria, renal lithiasis or cardiovascular complications 29,30. In our study, it is noteworthy that most pediatricians of both groups did not carry out analytical monitoring or follow-up with complementary examinations during treatment.
In terms of managing childhood osteoporosis guidelines, the European Society of Children's Endocrinology 28 and International Society of Clinical Densitometry (ISCD) 29 have published recommendations as has the nutrition committee of Spain’s Pediatric Society on infant nutrition and bone health 30. Despite this, most of the respondents from both the PC and SC groups reported that they lacked specific protocols to address this condition and referral networks for these patients, both at outpatient and hospital levels.
Furthermore, the training of our physicians regarding bone health is limited, the percentage being lower in PC pediatricians, a fundamental pillar in child care. In addition, most pediatricians in both areas consider their training on these aspects to be inadequate.
The main limitation of our work is that we could not ascertain the percentage of participation, since the surveys were not only disseminated by different scientific societies, but the participants were encouraged to forward the survey to their pediatric contacts who might be interested in taking part. Even so, taking into account the total pediatricians with healthcare activity in our country, we consider that the number of surveys implemented could be improved.
In addition, participation was voluntary, so it is likely that there is a certain participation bias. The physicians were more aware of the issue in question and responded to the survey. In any case, this does not invalidate the main conclusion of the study: the great variability in the approach of this entity.
In conclusion, the preventive activity in relation to childhood osteoporosis that is carried out in our environment varies greatly, and the training that pediatricians receive concerning osteoporosis is very scarce. In addition, there are no specific protocols in our environment to address children at risk. Consequently, adequate prevention and treatment measures are not being carried out in our child population, especially in patients with chronic disorders.
It is essential to optimize these aspects and involve pediatricians in detecting and preventing children at risk, to promote the maximum peak of bone mass in children, and thus reduce the incidence of osteoporosis in the future.
Bibliografía
1. Rauch F, Plotkin H, DiMeglio L, Engelbert RH, Henderson RC, Munns C. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2007 Pediatric Official Positions. J Clin Densitom. 2008;11:22-8. [ Links ]
2. Nevitt MC. Epidemiology of osteoporosis. Rheum Dis Clin North Am. 1994;20:535-9. [ Links ]
3. Diez Pérez A, Puig Manresa J, Martínez Izquierdo MT, Guelar Grimberg AM, Cucurull Canosa J, Mellibovsky Saidler L, et al. Aproximación a los costes de fractura osteoporótica de fémur en España. Med Clin. 1989;92:721-3. [ Links ]
4. Von Scheven E, Corbin KJ, Stagi S, Cimaz R. Glucocorticoid-associated osteoporosis in chronic inflammatory diseases: epidemiology, mechanisms, diagnosis, and treatment. Curr Osteoporos Rep. 2014;12:289-99. [ Links ]
5. Bryant RJ, Wastney ME, Martin BR, Wood O, McCabe GP, Morshidi M. Racial differences in bone turnover and calcium metabolism in adolescent females. J Clin Endocrinol Metab. 2003;88:1043-7. [ Links ]
6. Carrascosa A, Del Río L, Gussinyé M, Yeste D, Audí L. Mineralización del esqueleto óseo durante la infancia y adolescencia. Factores reguladores y patrones de normalidad. An Esp Pediatr. 1994:40:246-52. [ Links ]
7. Loud KJ, Gordon CM. Adolescence: bone disease. En: Walker, Watkins, Duggan, editores. Nutrition in Pediatrics. Basic Science and Clinical Applications. 3ª ed. Ontario. 2003. [ Links ]
8. Van der Sluis IM, de Muinck Keizer-Scharama SM. Osteoporosis in childhood: bone density of children in health and disease. J Pediatr Endocrinol Metab. 2001;14:817-32. [ Links ]
9. Daci E, van Cromphaut S, Bouillon R. Mechanisms influencing bone metabolism in chronic illness. Horm Res. 2002;58(Suppl 1):44-51. [ Links ]
10. Klibanski A, Adams CL. NIH Consensus Development Panel: Osteoporosis prevention, diagnosis and therapy. JAMA. 2001;285:785-95. [ Links ]
11. National Osteoporosis Foundation. Osteoporosis: Review of the evidence for prevention, diagnosis and treatment, and cost-effectiveness analysis. Executive summary. Osteoporos Int. 1998;8(Suppl 4):S3-6. [ Links ]
12. DeBar LL, Ritenbaugh C, Vuckovic N, Stevens VJ, Aickin M, Elliot D, et al. Youth: decisions and challenges in designing an osteoporosis prevention intervention for teen girls. Prev Med. 2004;39(5):1047-55. [ Links ]
13. Tussing L, Chapman-Novakofski K. Osteoporosis prevention education: behavior theories and calcium intake. J Am Diet Assoc. 2005;105:92-7. [ Links ]
14. Behringer M, Gruetzner S, McCourt M, Mester J. Effects of weight-bearing activities on bone mineral content and density in children and adolescents: A meta-analysis. J Bone Mineral Res. 2014;29:467-78. [ Links ]
15. Institute of Medicine (IOM). Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press; 2011. [ Links ]
16. Högler W, Ward L. Osteoporosis in Children with Chronic Disease. Endocr Dev. 2015;28:176-95. [ Links ]
17. Cassidy JT, Hillman LS. Abnormalities in skeletal growth in children with Juvenile Rheumatoid Arthritis. Rheum Dis Clin North Am. 1997;23:499-522. [ Links ]
18. García Nieto V, Ferrández C, Monge M, de Sequera M, Rodrigo MD. Bone mineral density in pediatric patients with idiopathic hypercalciuria. Pediatr Neprhol. 1997;11:578-83. [ Links ]
19. Galindo Zavala R, Núñez Cuadros E, Díaz Cordovés-Rego G, Urda Cardona AL. Avances en el tratamiento de la osteoporosis secundaria. An Pediatr (Barc). 2014;81:399.e1-7. [ Links ]
20. Recker RR, Cannata Andía JB, del Pino Montes J, Díaz Curiel M, Nogués i Solán X, Valdés Llorca C. Papel del calico y la vitamin D en el tratamiento de la osteoporosis. Rev Osteoporos Metab Miner. 2010;2(1):61-72. [ Links ]
21. Dibba B, Prentice A, Ceesay M, Stirling DM, Cole TJ, Poskitt EM. Effect of calcium supplementation on bone mineral accretion in Gambian children accostumed to a low-calcium diet. Am J Clin Nutr. 2000;71:544-9. [ Links ]
22. Greene DA, Naughton GA. Calcium and vitamin-D supplementation on bone structural properties in peripubertal female identical twins: A randomized controlled trial. Osteoporos Int. 2011;22:489-98. [ Links ]
23. Nieves JW, Melsop K, Curtis M, Kelsey JL, Bachrach LK, Greendale G, et al. Nutritional factors that influence change in bone density and stress fracture risk among young female cross-country runners. PM R. 2010;2:740-50. [ Links ]
24. Winzenberg TM, Shaw KA, Fryer J, Jones G. Calcium supplementation for improving bone mineral density in children. Cochrane Database Syst Rev. 2006;(2):CD005119. [ Links ]
25. Winzenberg T, Powell S, Shaw KA, Jones G. Effects of vitamin D supplementation on bone density in healthy children: Systematic review and meta-analysis. BMJ. 2011;342:c7254. [ Links ]
26. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clinic Endocrinol Metab. 2011;96:1911-30. [ Links ]
27. Bolland MJ, Avenell A, Baron JA, Grey A, Maclennan GS, Gamble GD, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: Meta-analysis. BMJ. 2010;341:c3691. [ Links ]
28. Shaw NJ. Management of osteoporosis in children. Eur J Endocrinol. 2008;159:S33-9. [ Links ]
29. Baim S, Leonard MB, Bianchi ML, Hands DB, Kalkwarf HJ, Langman CB, et al. Official Positions of the International Society for Clinical Densitometry and Executive Summary of the 2007 ISCD Pediatric Position Development Conference. J Clin Densitom. 2008;11:6-21. [ Links ]
30. Alonso Franch M, Redondo del Río MP, Suárez Cortina L. Nutrición infantil y salud ósea. An Pediatr (Barc). 2010;72:80.e1-11. [ Links ]
Received: October 17, 2017; Accepted: January 08, 2018











 text in
text in