My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Osteoporosis y Metabolismo Mineral
On-line version ISSN 2173-2345Print version ISSN 1889-836X
Rev Osteoporos Metab Miner vol.11 n.4 Madrid Nov./Dec. 2019 Epub Apr 06, 2020
https://dx.doi.org/10.4321/s1889-836x2019000400003
ORIGINALS
Long-term efficacy and safety of polymethylmethacrylate (PMMA) in osteoporotic patients treated by percutaneous vertebroplasty
1Spine Pathology Unit. Traumatology and Orthopedics Service. Jiménez Díaz Foundation University Hospital. Madrid (Spain).
2Spine Pathology Unit. Department of Orthopedic Surgery and Traumatology. Villalba General Hospital. Madrid (Spain).
3Neuroradiology Service. Jiménez Díaz Foundation University Hospital. Madrid (Spain).
4Radiology Service. Jiménez Díaz Foundation University Hospital. Madrid (Spain).
5Clinical Epidemiology Service. Jiménez Díaz Foundation University Hospital. Madrid (Spain).
Objetive:
Currently, there are limited data on the long-term influence of polymethylmethacrylate (PMMA) on the integrity of vertebral bodies after percutaneous vertebroplasty (PVP). Interesting investigation is being carried out into the possible relationship between this technique and the appearance over time of osteolytic phenomena or cement fragmentation in the intervened vertebrae. The objective of our study was to investigate whether there is a loss of effectiveness and/or safety of PVP with PMMA in the long term.
Material and method:
X-rays were analyzed of intervened patients corresponding to the immediate post-operative and the most recent radiological study (PVP more than 15 years previous). With both radiological studies, we describe: the height of the vertebral body, the angulation of lamellar plates and osteolytic presence around the cement over time.
Results:
A total of 7 patients operated by PVP with PMMA 15 or more years earlier agreed to have a new radiograph in our center. After the analysis of their post-operative images (immediate and 15 or more years after surgery), no loss of height of the cemented vertebral body, differences in angulation in the lamellar plates, presence of osteolysis around the vertebrae was observed in any of the involved vertebrae cement or fragmentation of the injected PMMA.
Conclusions:
PMMA injected into the vertebral body remains stable over time (more than 15 years). There are no changes in the bone-PMMA interface, osteolysis and/or changes in the height of the vertebral bodies in the cases analyzed.
Key words: vertebroplasty; PMMA; spine surgery; vertebral fracture; osteoporosis; osteolysis
INTRODUCTION
Without a doubt, vertebral fracture (VF) is the most prevalent type of bone rupture in patients with low bone mass1. The most recent epidemiological data in the Spanish population indicate about 35% VF prevalence in women over 45 years of age2. In men, the prevalence at 50 years is estimated 5 times lower than that of the female population, although this increases beyond 70 years of age3.
Osteoporotic VFs (OVF) are conservatively treated, usually including rest, analgesia (in combination with muscle relaxants), orthotics and rehabilitation. This treatment is crucial in the first weeks post-fracture, so that proper follow-up usually resolves OVFs effectively. However, in 10-35% of patients, complications may arise from the fracture itself, such as delayed bone union, increased kyphosis, appearance of neurological disorders or the appearance of pseudo-arthrosis (Kümmell's disease). In these cases, patients frequently do not respond well to conservative treatment, complicating the management of their symptoms. This tends to worsen over time4.
Regarding these patients' failure to respond to conservative treatment, the appearance in recent decades of minimally invasive techniques, such as vertebroplasty (VP) and percutaneous kyphoplasty, has provided a good therapeutic alternative both for managing symptoms and avoiding serious long-term complications.
VP consists of injecting polymethylmethacrylate (PMMA) bone cement into the fractured vertebral body, with the immediate objective of curbing the vertebra's collapse, increasing its resistance and alleviating pain5.
The new cements available for use in cementoplasty require preparation in a highly specific monomer/polymer ratio that prevents alterations in the viscosity of the final mixture. This factor is crucial both for a correct polymerization and for the application of the cement itself, since it is during this phase when the mixture is injected into the affected vertebrae of the patient. Thanks to the improvement of its properties in recent years, the new cement mixtures minimize material leaks from the bodies and reduce the thermal effect on the healthy bone surrounding the fracture. Thus, the PMMA is more effective in repairing the OVF as well as making it more secure6,7. Although several studies demonstrate VP's short-term efficacy and safety8 9 10 11-12, its long-term stability has not yet been fully established.
This paper is the first to evaluate the bone status of fractured osteoporotic vertebrae that were cemented by PVP and that have a follow-up of µ15 years. Our main objective is to assess the long-term bone integrity of the intervened vertebrae, to thus clarify the safety and efficacy of the technique over time.
MATERIAL AND METHODS
Study population
We present a series of 7 clinical cases in which their postsurgical follow-up is analyzed descriptively. This is a singlecenter study, carried out at the Fundación Jiménez Díaz University Hospital (FJD) in Madrid (Spain) with the approval of the Ethics Committee of the same hospital. Thus, for its realization, the monitoring and compliance with the standard ethical standards set forth in the Helsinki Declaration of 1964 and its subsequent revisions is confirmed (Tokyo 1975, Venice 1983, Hong Kong 1989, Somerset West 1996, Edinburgh 2000, Seoul 2008 and Fortaleza 2013)13.
Our study population was selected through a database belonging to our Spinal Pathology Unit (SPU-FJD), where information and other relevant clinical data of those patients operated by PVP are collected by usual clinical practice. As screening criteria, patients with a diagnosis of OVF and with post-surgical follow-up ≥15 years were selected from this database, which met another set of additional criteria described below.
Inclusion and exclusion criteria
The criteria to be met for inclusion within the study population included: having reached adulthood regardless of gender; bone densitometry values (DXA column) compatible with osteoporosis or osteopenia; diagnosis of OVF, failure of conservative treatment reported in the medical history; intervention by percutaneous VP carried out exclusively by SPU-FJD surgeons; and patients who will be clinically and radiologically monitored at 15 or more years after surgery (PO≥15a).
Similarly, patients were excluded who, even if meeting the above criteria, presented VF any non-osteoporotic or doubtful etiology, had presented infection or any other type of post-operative complication and/or were subsequently intervened by instrumentation (instrumented vertebral arthrodesis).
Study variables and image analysis
Data related to the study variables: sex, age at the time of surgery, weight, height, body mass index (BMI), T-score values, number of OVFs, surgical approach, vertebral cementation level (cervical, thoracic, lumbar), presence of osteolysis foci and presence of fragmented material were extracted from the database belonging to the UPC-FJD. All these variables were documented and stored in electronic format, creating a data file owned by the UPC-FJD. Each set of data was recorded in relation to a random code that was assigned to each patient thus guaranteeing the confidentiality of their data14.
Radiologists from the Neuroradiology Service (FJD) analyzed the images of each patient corresponding to immediate post-operative (PO) (radiographic paper support) and the PO≥15a (exported using Surgimap®software). This analysis searched for vertebral bone alterations, foci of osteolysis around the material and/or cases of fragmented PMMA. In addition, measurements were made of the heights (anterior, middle and posterior) and angulation of the plates of each of the intervened vertebrae.
RESULTS
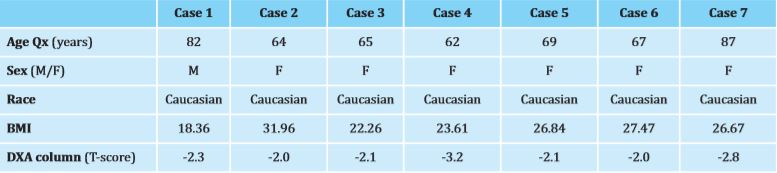
After reviewing the SPU-FJD database, we obtained a total of 69 records corresponding to patients operated by PVP in our hospital 15 years or older. From this total of cases, we observed 26 follow-up losses (38% with respect to the total number of records) as we were unable to contact these patients or know their current status. However, we contacted a total of 43 patients or their relatives, which allowed us to know a total of 30 cases of exitus (70%) and 13 cases of patients still alive (30%) (Figure 1). Among the living patients, 7 of them agreed to undergo a new radiography, these images being the most recent radiological studies and corresponding to the follow-up PO≥15a after the VP. Thus, we obtained a series of 7 cases of patients having undergone VP surgery with a radiological follow-up of 15 years or more.
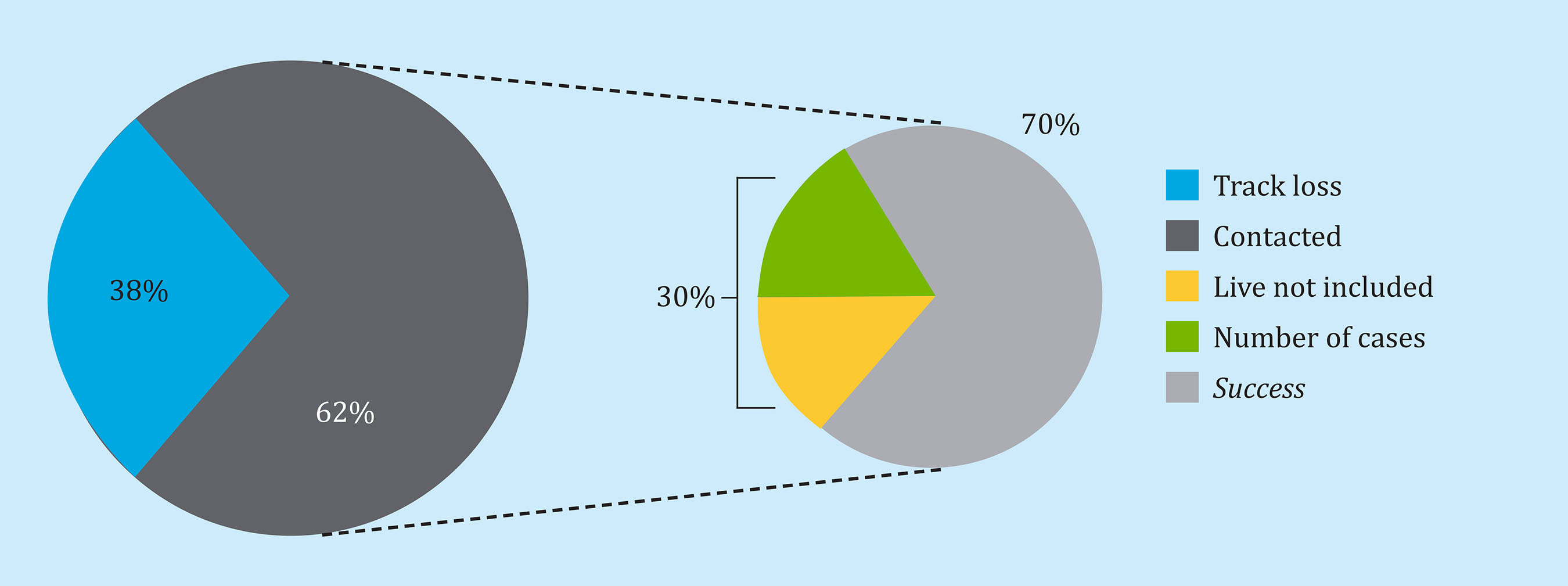
Figure 1. Summary graph of the study population. From a total of 69 patients operated by VP 15 or more years ago in our hospital, a total of 43 patients/relatives (62% of the total) were contacted. After confirming 70% of cases of death, the remaining 30% (13 patients) are invited to go to the hospital for a new radiological study (PO≥15 years). Finally, 7 patients accept and form the case series on which the study is based
This case series consisted of 6 Caucasian women and 1 male whose median age at the time of surgery was 67 years (min=62; max=87, interquartile range=18). The pre-operative BMI had a median of 26.67 (min=18.36; max=31.96, interquartile range=5.21) (Table 1). All patients in this series presented T-score values compatible with osteoporosis or osteopenia before surgery.
Table 1. Demographic data of the series of 7 patients operated 15 or more years ago by VP in the SPU-FJD
Age Qx: age at surgery; M: male; F: female; BMI: body mass index; DXA: dual energy x-ray absorptiometry.
In addition, in all cases the OVF intervened was single level (total number of intervened levels within the case series=7), the conservative treatment prior to surgery having been ineffective (Table 1).
SPU-FJD surgeons of the carried out the corresponding surgical interventions, with a uni-portal approach in 5 cases and bi-portal in 2 cases. The intervened vertebrae were in 4 thoracic cases: T7, T11 and T12 (2 cases of the latter) and in 3 lumbar cases: L3, L4 and L5.
The measurements taken by the FJD team of neuroradiologists allowed us to establish that there were no clinically significant differences in the height of the vertebral bodies (anterior, middle or posterior wall) of the patients comparing the PO and PO≥15a times (Table 2).
Table 2. PVP characterization, vertebral PO and PO measures ≥15a and data related to the presence of osteolysis/fragmentation foci of the PMMA of the series of 7 operated patients
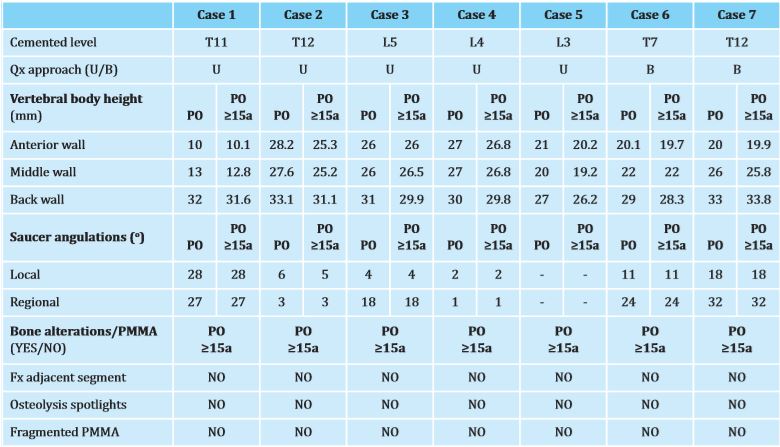
T: thoracic vertebra; L: lumbar vertebra; QX approach: surgical approach; U: uniportal; B: biportal; PO: immediate post-operative; PO≥15a: post-operative at 15 or more years of follow-up; Fx: fracture.
Similarly, except for case 5, in which the corresponding measurements could not be made, the remaining cases did not show differences in the angulation of the intervened vertebrae by comparing their PO and PO values ≥15a (Table 2).
In addition, in no case were fractures and/or height losses in segments adjacent to the original fracture (a single case recorded a new non-adjacent fracture). There was no osteolytic phenomena around the injected PMMA or fragmentation in the images analyzed corresponding to PO≥15a (Table 2, Figure 2).
DISCUSSION
OVFs constitute the most common simple fracture worldwide. In fact, in our country, the Spanish Society of Geriatrics and Gerontology (SEGG) provided data in 2017 that documents a 3-fold higher incidence of this type of fracture compared to hip fractures15.
Recent research lines have shown that, in addition to osteoporosis, factors such as advanced age, high BMI and/or fractures in thoracic levels (especially in the thoracolumbar junction) are significantly related to the failure of conservative treatment16,17. According to the clinical practice carried out in our center, we can establish a failure rate of conservative treatment in the management of acute OVFs of around 15%. These data are similar to those reported by some authors who place it close to 20% according to the specific type of VF18. In the series of 7 patients that we presented, all women were operated on in an advanced postmenopausal age, while the male patient underwent surgery was octogenarian. In addition, 3 patients presented BMI values compatible with overweight and 1 with obesity. As for the intervened vertebral level, 4 patients presented fractures in the thoracic vertebrae, of which in 2 cases the T12 (thoracolumbar junction) coincided. These data seem to support the relationship between the aforementioned risk factors and the failure of conservative treatment in their fractures.
Beyond 65 years of age, especially in women, the maximum level of prevalence of OVFs in the Spanish population is reached. Thus, our study accurately represents this situation with the case series analyzed. The profile of the recruited patients would be within a population group that, due to their demographic and physiological characteristics, is at risk of suffering an OVF.
Faced with an OVF with symptoms that cannot be managed by conservative treatment, PVP presents an effective option in the improvement of the patient's pain, functional status and quality of life, even in elderly cases19 21 22-22.
The safety and immediate effects of PVP are well documented in the literature23 24 25 26-27. However, so far, there are very few data that continue to demonstrate the effectiveness and safety of this technique in the long term28,29. In fact, the post-op follow-up periods published do not generally exceed 2 years9 10 11-12.
According to the latest data from the National Statistics Institute (NSI) updated in 2018, the life expectancy of the Spanish population stands at 83 years, taking into account both sexes30. This increase in the aging of the population provides new information that allows us to show PVP as a safe technique in the longer term.
In addition, there is some controversy among authors regarding a possible relationship between the realization of PVP and the appearance over time of new FV31 32-33. This reason justifies the analysis, such as the one we present here, where post-surgery follow-ups are recorded much longer over time.
In the 7 cases presented, the patients presented stability in the intervened vertebral bodies at the level of the anterior, middle and posterior walls with 15 or more years elapsed from the time of surgery. There are some published data that associate changes in the angulation of the lamellar plate after VF as a risk factor in the appearance of new VF31,34. In our series of patients analyzed, there were no clinically significant differences in this angulation after 15 or more years post-op which could justify, together with other factors such as maintenance of osteoporotic treatment, that these patients have not suffered new VF in adjacent segments.
The local response of the host to PMMA has been studied as a long-term phenomenon mainly in cases of implantation of total hip prostheses (THPs). In this type of prosthesis with peri-prosthetic cementation, the development of an inflammatory response by the surrounding bone to the implant cement is common. This reaction would derive, among other causes, as a consequence of the exothermic process during setting and the release of PMMA particles that appear due to wear and tear due to the compression exerted by the movement itself35.
Unlike the PMMA of the THPs, in the PVP the cement is interdigitated in the trabecular bone and is not subject to direct compression. This may explain why, as we present in our case series, no PMMA fragmentation or osteolytic phenomena is observed in PO≥15a.
In recent years, new PMMA formulations have been developed, for example, without setting temperature or coated with osteoblasts36 37-38. According to published data, these new cements do not seem to offer much more beneficial effects or greater efficacy than conventional PMMA compared to an OVF. Given current concerns regarding health costs, it would seem illogical to increase this expense in other PMMAs or in more expensive techniques such as balloon kyphoplasty without clinical data that clearly endorse it39. In addition, as we present, in our center we observe that 70% of the patients operated 15 or more years ago were exitus due to causes unrelated to their OVF. Meanwhile, those who were still alive presented stability of the injected PMMA after this time.
The present study describes the experience of a small group of patients (n=7 of 13 available) with a similar diagnosis. Due to the limitation in their number of cases there is no way to carry out statistics of inferential type, although descriptive study is possible.
CONCLUSION
This work constitutes the first evidence of PVP as a safe and effective technique in patients with a follow-up of 15 or more years after their surgery. PMMA kept both heights (anterior, middle and posterior) and vertebral angulation stable, in addition to not causing osteolytic phenomena or observing long-term material fragmentation.
REFERENCES
1 Griffith JF. Identifying osteoporotic vertebral fracture. Quant Imaging Med Surg. 2015;5(4):592-602. [ Links ]
2 Herrera A, Mateo J, Gil-Alvaroba J, Lobo-Escolar A, Artigas JM. Prevalence of osteoporotic vertebral fracture in Spanish women over age 45. Maturitas. 2015;80 (3):288-95. [ Links ]
3 Olmos JM, Hernández JL, Martínez J, Pariente E, Castillo J, Prieto-Alhambra D, et al. Prevalence of vertebral fracture and den-sitometric osteoporosis in Spanish adult men: The Camargo Cohort Study. J Bone Miner Metab. 2018; 36(1): 103-10. [ Links ]
4 Funayama T, Tsukanishi T, Abe T, Kumagai H, Izawa S, Noguchi H, et al. Prediction of treatment resistance in conservative treatment of osteoporotic vertebral fractures using lateral plain dynamic loading radiographs. J Spine. 2017;6(6):1000404. [ Links ]
5 Deramond H, Depriester C, Toussaint P, Galibert P. Percutaneous vertebroplasty. Semin Musculoskelet Radiol. 1997; 1(2): 285-96. [ Links ]
6 Bardaji S, Borrós S. New developments in vertebroplasty materials. Afinidad. 2018;75(583): 165-74. [ Links ]
7 Lv Y, Li A, Zhou F, Pan X, Liang F, Qu X, et al. A novel composite PMMA-based bone cement with reduced potential for thermal necrosis. ACS Appl Mater Interfaces. 2015;7(21): 11280-5. [ Links ]
8 Leali PT, Solla F, Maestretti G, Balsano M, Doria C. Safety and efficacy of vertebroplasty in the treatment of osteoporotic vertebral compression fractures: a prospective multicenter international randomized controlled study. Clin Cases Miner Bone Metab. 2016;13(3):234-6. [ Links ]
9 Kotwica Z, Saracen A. Early and long-term outcomes of vertebroplasty for single osteoporotic fractures. Neurol Neurochir Pol. 2011;45(5):431-5. [ Links ]
10 Thillainadesan J, Schlaphoff G, Gibson KA, Hassett GM, McNeil HP. Long-term outcomes of vertebroplasty for osteoporotic compression fractures. J Med Imaging Radiat Oncol. 2010;54(4):307-14. [ Links ]
11 Tanigawa N, Kariya S, Komemushi A, Nakatani M, Yagi R, Kohzai M, et al. Percutaneous vertebroplasty for osteoporotic compression fractures: long-term evaluation of the technical and clinical outcomes. AJR Am J Roentgenol. 2011;196(6):1415-8. [ Links ]
12 Zuo XH, Zhu XP, Bao HG, Xu CJ, Chen H, Gao XZ, et al. Network meta-analysis of percutaneous vertebroplasty, percutaneous kyphoplasty, nerve block, and conservative treatment for nonsurgery options of acute/subacute and chronic osteoporotic-vertebral compression fractures (OVCFs) in short-term and long-term effects. Medicine (Baltimore). 2018;97(29):ell544. [ Links ]
13 World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. (64th WMA General Assembly, Fortaleza, Brazil, October 2013). [ Links ]
14 Jefatura del Estado. Sección I. Disposiciones Generales. Ley Orgánica 15/1999, de 13 de diciembre, de Protección de Datos de Carácter Personal. BOE num. 298, de 14 de diciembre de 1999, pps:43088-43099. [ Links ]
15 Sociedad Española de Geriatría y Gerontología (SEGG). Nota de prensa de Salud [citada el 23 de Feb de 2017]. En España la osteoporosis afecta a 3,5 millones de personas (Disponible en: https://www.segg.es/institucional/2017/02/23en-espa%C3%Bla-la-osteoporosis-afecta-a-3-mi-llones-y-medio-de-personas) [ Links ]
16 Zhang J, He X, Fan Y, Du J, Hao D. Risk factors for conservative treatment failure in acute osteoporotic vertebral compression fractures (OVCFs). Arch Osteoporos. 2019;14(1):24. [ Links ]
17 Muratore M, Ferrera A, Masse A, Bistolfi A. Osteoporotic vertebral fractures: predictive factors for conservative treatment failure. A systematic review. Eur Spine J. 2018;27(10):2565-76. [ Links ]
18 Shen J, Xu L, Zhang B, Hu Z. Risk factors for the failure of spinal burst fractures treated conservatively according to the thoracolumbar injury classification and severity score (TLICS): A retrospective cohort trial. Plos One. 2015;10(8): e0135735. [ Links ]
19 Zhu RS, Kan SL, Ning GZ, Chen LX, Cao ZG, Jiang ZH, et al. Which is the best treatment of osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment? A Bayesian network meta-analysis. Osteoporosis Int. 2019; 30(2):287-98. [ Links ]
20 Cheng J, Muheremu A, Zeng X, Liu L, Liu Y, Chen Y. Percutaneous vertebroplasty vs balloon kyphoplasty in the treatment of newly onset osteoporotic vertebral compression fractures. Medicine (Baltimore). 2019;98(10):el4793. [ Links ]
21 Clarendon F, Fahed R, Gabrieli J, Guermazi Y, Cormier E, Molet-Benhamou L. Safety and clinical effectiveness of percutaneous vertebroplasty in the Elderly (>80 years). Eur Radiol. 2016;26(7): 2352-8. [ Links ]
22 Nasuto M, Falcone M, Strizzi V, Florio L, Lauriola W, Ciccarese G. Vertebroplasty in elderly patients: A clinical effectiveness analysis. Curr Radiol Rep. 2018;6:30. [ Links ]
23 Traquilli P, Solla F, Maestretti G, Balsano M, Doria C. Safety and efficacy of vertebroplasty in the treatment of osteoporotic vertebral compression fractures: a prospective multicenter international randomized controlled study. Clin Cases Miner Bone Metab. 2016;13(3): 234-6. [ Links ]
24 Clark W, Bird P, Gonski P, Diamond TH, Smerdely P, McNeil HP, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016; 388(10052): 1408-16. [ Links ]
25 Kamei S, Noguchi T, Shida Y, Okafuji T, Yokoyama K, Uchiyama F, et al. The safety and efficacy of percutaneous vertebroplasty for patients over 90 years old. Jpn J Radiol. 2019;37(2):178-85. [ Links ]
26 Xie L, Zhao ZG, Zhang SJ, Hu YB. Percutaneous vertebroplasty versus conservative treatment for osteoporotic vertebral compression fractures: An updated meta-analysis of prospective randomized controlled trials. Int J Surg. 2017; 47:25-32. [ Links ]
27 Álvarez L, Alcaraz M, Pérez-Higueras A, Granizo JJ, de Miguel I, Rossi RE, et al. Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine. 2006;31(10): 1113-8. [ Links ]
28 Xu BS, Hu YC, Yang Q, Xia Q, Ma XL, Ji N. Long-term results and radiographic findings of percutanous vertebroplasties with polymethylmethacrylate for vertebral osteoporotic fractures. Chin Med J (Engl). 2012;125(16):2832-6. [ Links ]
29 Kim JH, Yoo SH, Kim JH. Long-term Follow-up of percutaneous vertebroplasty in osteoporotic compression fracture: minimum of 5 years follow-up. Asian Spine J. 2012;6(1):6-14. [ Links ]
30 Instituto Nacional de Estadística (INE). España en cifras 2018. (Disponible en: http://www.ine.es/prodyser/espa_ci-fras/2018/index.html). [ Links ]
31 Lee HJ, Park J, Lee IW, Yi JS, Kim T. Clinical, radiographic, and morphometric risk factors for adjacent and remote vertebral compression fractures over a minimum follow-up of 4 years after percutaneous vertebroplasty for osteoporotic vertebral compression fractures: Novel three-dimensional voxel-based morphometric analysis. World Neurosurg. 2019;125: el46-57. [ Links ]
32 Borensztein M, Camino Willhuber GO, Posadas Martínez ML, Gruenberg M, Sola CA, Velan O. Analysis of risk factors for new vertebral fracture after percutaneous vertebroplasty. Global Spine J. 2018;8(5):446-52. [ Links ]
33 Li H, Yang DL, Ma L, Wang H, Ding WY, Yang SD. Risk factors associated with adjacent vertebral compression fracture following percutaneous vertebroplasty after menopause: a retrospective study. Med Sci Monit. 2017;23:5271-6. [ Links ]
34 Han S, Jang IT. Analysis of adjacent fractures after two-level percutaneous vertebroplasty: is the intervening vertebral body prone to re-fracture? Asian Spine J. 2018;12(3):524-32. [ Links ]
35 Koulouvaris P, Ly K, Ivashkiv LB, Bostrom MP, Nestor BJ, Sculco TP, et al. Expression profiling reveals alternative macrophage activation and impaired osteogenesis in periprosthetic osteolysis. J Orthop Res. 2008;26(1):106-16. [ Links ]
36 Aghyarian S, Hu X, Lieberman IH, Kosmopoulos V, Kim HK, Rodrigues DC. Two novel high performing composite PMMA-CaP cements for vertebroplasty: An ex vivo animal study. J Mech Behav Biomed Mater. 2015;50:290-8. [ Links ]
37 Tai CL, Lai PL, Lin WD, Tsai TT, Lee YC, Liu MY, et al. Modification of mechanical properties, polymerization temperature, and handling time of polymethylmethacrylate cement for enhancing applicability in vertebroplasty. Biomed Res Int. 2016;2016: 7901562. [ Links ]
38 Goñi I, Rodríguez R, García-Arnáez I, Parra J, Gurruchaga M. Preparation and characterization of injectable PMMA-strontium-substituted bioactive glass bone cement composites. J Biomed Mater Res B Appl Biomater. 2018; 106 (3):1245-57. [ Links ]
39 Li CS, Chang CS, Liao WJ. Long-term follow-up study of osteoporotic vertebral compression fracture treated using balloon kyphoplasty and vertebroplasty. J Neurosurg Spine. 2015;23(l):94-8. [ Links ]
Received: June 30, 2019; Accepted: November 16, 2019











 text in
text in