My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Osteoporosis y Metabolismo Mineral
On-line version ISSN 2173-2345Print version ISSN 1889-836X
Rev Osteoporos Metab Miner vol.13 n.1 Madrid Jan./Mar. 2021 Epub May 17, 2021
https://dx.doi.org/10.4321/s1889-836x2021000100008
SPECIAL ARTICLE
Care profile of susceptible patients with osteoporosis by telemedicine visits in the post-COVID-19 era
1Intermedial Care Hospital El Carme. Badalona Assistance Services. Badalona. Barcelona (Spain)
2Clinical Hospital. Barcelona (Spain)
3Hospital Moisès Broggi. Sant Joan Despí. Barcelona (Spain)
4Hospital of Terrassa. Consorci Sanitari de Terrassa. Barcelona (Spain)
5Sant Antoni Abad Hospital. Alt Penedés Garraf Health Consortium. Vilanova i la Geltrú. Barcelona (Spain)
6Sant Jaume Hospital. Maresme Health Consortium. Mataró. Barcelona (Spain)
7L'Hospitalet Public Health Hospital. Barcelona (Spain)
8Francolí Public Health Hospital. Tarragona (Spain)
Objetive
Define the profile of the candidate and non-candidate osteoporosis patient for assistance in osteoporosis teleconsultation, in the post-COVID-19 era. Proposal of a management protocol for outpatient follow-up.
Methods
We have carried out a bibliographic review through a systematic search in the Pubmed.gov databases of the available evidence of articles in English and Spanish with an inclusion date until October 2020, following the recommendations of the GRADE system (Grading of Recommendations, Assessment, Development and Evaluation). Database is aimed at locating and accessing relevant information for this review in an updated way.
Results
The profile of the patient candidate for teleconsultation would be of those who present a history of osteoporosis, previously diagnosed, with treatment and requiring follow-up. COVID-19 has occurred in a context in which the main causes of mortality are chronic diseases and the need to protect against transmission.
Conclusions
We propose a consensus for managing this patient, with differentiated sections for the different stages of the telematic care process. This will help in clinical decision-making and also in the process of follow-up and therapeutic adherence and, therefore, in optimal use of healthcare resources.
Key words osteoporosis; telemedicine; COVID-19; outpatient care
INTRODUCTION
Osteoporotic fractures represent a growing public health problem worldwide. At present, we lack adequate procedures for prevention, diagnosis, assessment, intervention and patient follow-up.
New technologies have provided new communication tools and have changed our mentality, with the possibility of carrying out, virtually, actions or procedures in our daily lives that until now required our physical presence, either for technical, cultural or social reasons1.
The COVID-19 pandemic, caused by the SARS-COV-2 virus, has triggered a global public health emergency with rapid evolution and tragic consequences. The fight against this disease is forcing to modify the forms of care, which includes transforming some face-to-face consultations into remote ones2.
Prior to the COVID-19 pandemic, telemedicine, in its different forms, was used in exceptional situations. One of the first uses was the tele-nursing practice that emerged in the UK and Canada at a primary care level.
During the alarm or lock-down period and the ensuing care crisis caused by the pandemic, which began in March 2020, we have been forced to carry out inquiries electronically. Osteoporosis, as a chronic disease, is a healthcare challenge in this new situation in our consultations, which we should take advantage of to assess its benefits and be able to overcome its barriers. For this reason, the definition of a clinical profile of the patient and the creation of a care circuit are absolutely necessary to ensure the correct care of these patients. However, today, the information available on the possible benefits or safety of this type of telematic care is quite limited3.
The objective of our proposal is to develop a protocol for the management of the patient in telematic follow-up, where it is essential to promote coordinated action between the different levels of care, Primary Care, Social Healthcare and Hospital, with the participation of doctors from the various specialties involved, as well as Nursing and Community Pharmacy, which facilitate detection, assessment and treatment, ensuring good adherence.
PROFILE OF THE PATIENT WITH OSTEOPOROSIS WHO ATTENDS OUTPATIENT CONSULTATIONS FOR VARIOUS MEDICAL SPECIALTIES
The profile of the patient with osteoporosis is diverse and various specialties converge in their care, developing their activity at all levels of care (rheumatologists, internists, family doctors, gynecologists, trauma specialists, geriatricians, physical therapists), different specialties for the same patient with osteoporosis. What varies is the reason for consultation, the vital moment and the location of the patient. Medical societies have collected the characteristics of patients with osteoporosis, making it possible to establish the characteristic profile in each specialty. The RETOSS (Rheumatology and Osteoporosis) study, promoted by the Spanish Society of Rheumatology (SER), analyzed the profile of patients with postmenopausal osteoporosis in the rheumatology consultation. These were patients with low calcium intake, a family history of fracture, a previous history of fractures, insufficient calcidiol levels, and aged over 70 years, in addition to a high incidence of back pain.
Most were referred from Primary Care (63%), Gynecology (13.8%) or Trauma (10%)4.
The OSTEOMED (Osteoporosis in Internal Medicine) registry, promoted by the Osteoporosis Working Group (GTO) and under the aegis of the Spanish Society of Internal Medicine (SEMI), showed that the main reasons for consultation in Internal Medicine services were confirmed vertebral fractures (17.2%), non-vertebral fractures (9.1%), back pain or kyphosis (9.8%), musculoskeletal pain (11.4%), and suspected secondary osteoporosis (7.2 %). Overall, it was a sedentary patient profile (36%), with low sun exposure (23%). An active search for patients receiving corticosteroids was recommended, and in this the Internal Medicine and Primary Care consultations play an important role. The patients were referred from Primary Care, other hospital services and other consultations of the Internal Medicine service itself5.
From the geriatrics perspective, the National Registry of Hip Fractures (NRHP) collects hip fracture patients older than 75 years admitted in 2017 in 54 hospitals in Spain. It is the Spanish prospective study of a patient with a higher mean age, mainly women, and with a high percentage of previous cognitive impairment, mostly without prior treatment for osteoporosis. Differences are evident between autonomous communities, such as access to functional rehabilitation units, the probability of returning home or secondary prevention of fractures6.
In an attempt to unify criteria for diagnosis, treatment and referral to the different specialists that converge around the patient with osteoporosis, the scientific societies of specialties involved in the treatment of osteoporosis presented a consensus document in 2017, establishing three well-differentiated profiles with postmenopausal osteoporosis (PMO)7.
A. Osteoporosis patient without fracture
The consensus agrees that in patients without risk of fracture, follow-up should be carried out by Primary Care or Rheumatology. In case of high risk of fracture, the follow-up by Rheumatology would be prioritized. Patients with early surgical or symptomatic menopause are subject to Gynecology care. In case of associated thyroid disease, she would be treated by Endocrinology.
Those patients with osteoporosis where a significant loss of bone mineral density is observed, despite correct pharmacological treatment, would require rheumatology care.
In all patients whose musculoskeletal condition also conditions pain or functional loss, an assessment and subsequent follow-up by Rehabilitation would be recommended.
As complementary examinations, bone densitometry (dual radiological absorptiometry –DXA–) and lumbar spine radiography are recommended every 2 years. The consultation should also serve to underline adherence to treatment.
B. Patient with osteoporosis with vertebral fracture
In acute vertebral fracture, especially involving the posterior wall, it is the Traumatology Service that must assess the surgical option, which must be accompanied by a medical evaluation by Rheumatology, Internal Medicine or Geriatrics according to age and comorbidities5.
The importance of having an FLS (Fracture Liaison Service), or a Bone Metabolism Unit, as a device that should assume responsibility for such fractures is highlighted8.
At the follow-up level after the acute moment, followup by rheumatology and rehabilitation or geriatrics is recommended in case of advanced age or functional or cognitive deficit. At the level of outpatient follow-up, primary care is recommended, provided there are specifically trained professionals.
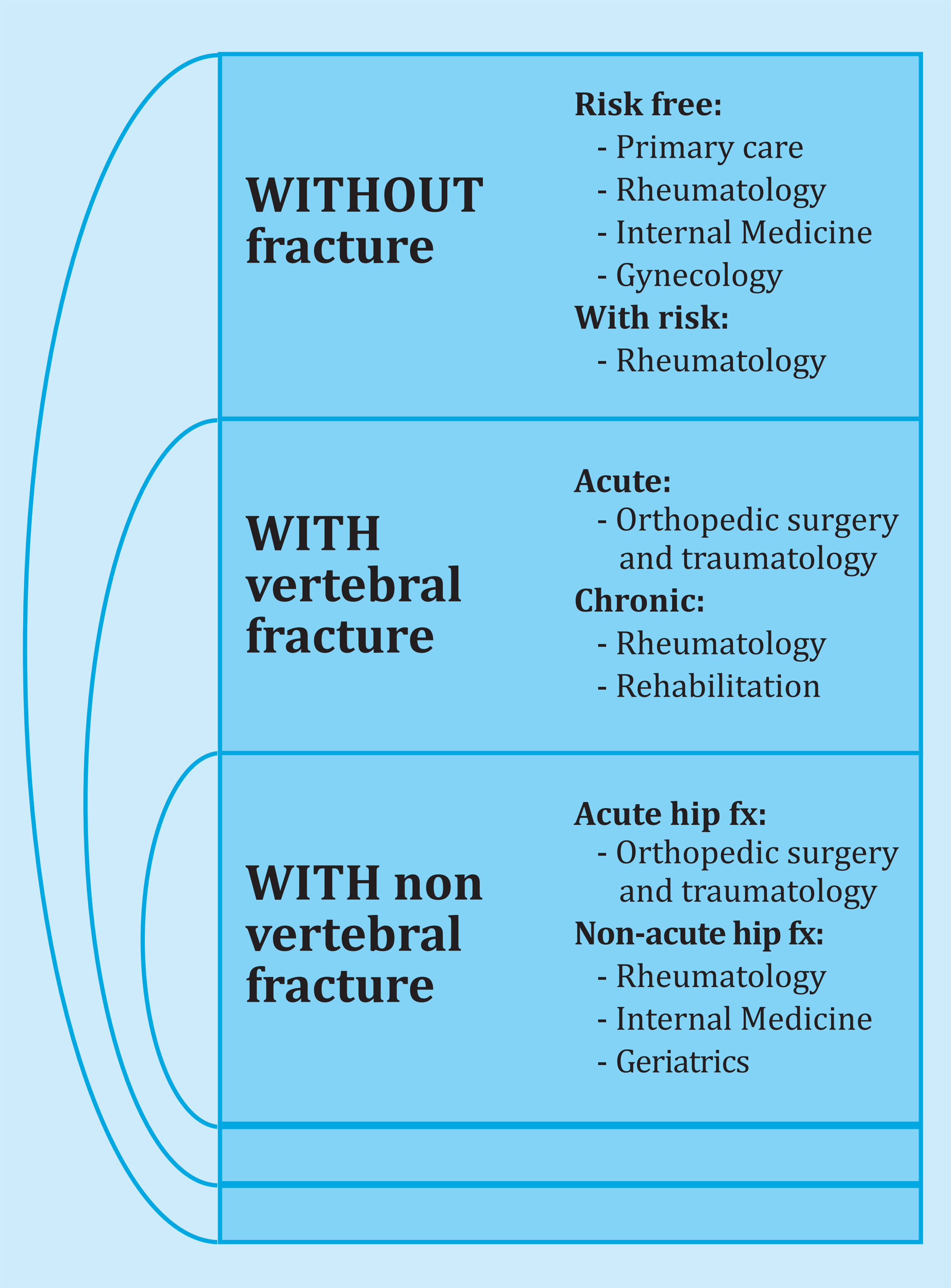
Figure 1. Medical care circuits for patients diagnosed with postmenopausal osteoporosis (PMO) according to the patient's profile. Adaptado de Blanch et al.7
C. Osteoporosis patient with non-vertebral fracture
These fractures correspond mainly to hip and distal radius fractures. The acute phase care corresponds to Traumatology, but the care by interdisciplinary teams integrated in an FLS or orthogeriatric unit have shown improvements in both complications and mortality, as well as functional improvement at discharge. They also improve coordination with primary care and secondary prevention of new fractures10.
To sum up, regardless of the referring specialty, the recommendation is:
Attention to the fracture by multidisciplinary units. To highlight the role of the FLS.
Coordination between levels of care, especially highlighting the role of Primary Care in secondary prevention.
Establish standardized evaluation and follow-up measures (risk of fracture, pain, functional capacity, quality of life).
IMPACT OF COVID-19 INFECTION FOR OSTEOPOROSIS OUT-PATIENT CLINICS
During the period of the recent health crisis, telemedicine has been the main contact tool for patients of hospitals and outpatient clinics. Previously, its use had been rather sporadic11.
One of the most affected hospital environments has been outpatient facilities, both due to the limitation of face-to-face visits by patients and the availability of doctors given the great overload in hospital wards.
Furthermore, patients have limited or reduced attendance at face-to-face consultations for fear of being infected, which may lead to follow-up problems, cancellation of diagnostic tests or delay in requesting initial specialist visits12,13.
According to the Catalan Health Service data, in Catalan hospitals over the second quarter of 2020, initial visits of any specialty decreased by 50% compared to the same quarter of the previous year without recovering in the third quarter (70% of those made in 2019), the majority being by telemedicine. Before the health crisis, 13,500 face-to-face visits, 14,500 telephone visits and about 1,000 telematic consultations were attended daily in Primary Care centers; now face-to-face visits are around 18,000 a day, telephone visits around 86,000 and telematic consultations around 17,00014.
TELEMEDICINE IN THE COVID-19 ERA
Digital tools offer important opportunities to reshape current healthcare systems, and are not incompatible with face-to-face visits throughout the doctor-patient relationship. There will be times when the face-to-face consultation makes more sense (first visits) and at other times it will be more convenient to use telemedicine (follow-up).
There are different formats of telematic consultation:
By telephone. Through a phone call from the doctor to the patient.
Video call. It consists of calling the patient through a device that allows the patient and the doctor to see each other, which facilitates both identification and non-verbal communication.
Electronic consultation or e-consultation. Telematic contact between professionals and with the patient that would allow resolution of doubts.
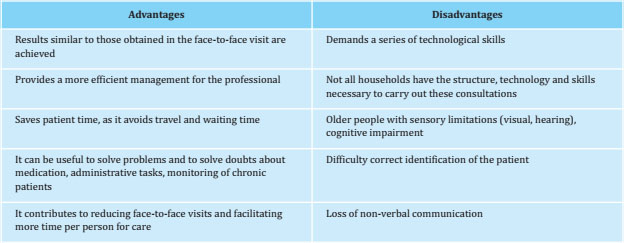
Telematic consultation has advantages and disadvantages (Table 1)15,16. The Catalan Health Service has published a document affirming that telematic care may be more useful in the follow-up visits of stable chronic patients who are well aware of their condition and do not require a physical examination17.
There is scientific evidence regarding telemedicine use in the field of osteoporosis18. Some telemedicine experiences have been carried out in countries with great distances between populations such as Australia and Canada, where the geography and distribution of health workers require a remote approach to the ambulatory care of health problems in the population19. A recent study from a Canadian osteoporosis telemedicine program found that participating patients perceived a number of benefits such as high-quality care, valued the experience and credibility of the treating physician, but also posed some drawbacks such as coordination of their care with the results of the complementary examinations carried out and, sometimes, the sub-optimal follow-up of other health professionals, such as physiotherapists20.
In the United Kingdom, telephone consultations are promoted in the clinical guidelines for follow-up consultations in the Fracture Liasion Service (FLS) with the aim of promoting adherence to osteoporosis treatment21.
The great challenge for the future is in the transition to the post-pandemic phase, since the key transformation of telemedicine is to change from a crisis mode (where the use of provisional or unapproved technologies has been allowed) to a sustainable mode where it is necessary for the different health centers to invest in systems that guarantee the safe transfer of data, the encryption of emails, guaranteeing patient privacy along with longterm technical support22,23.
Directive 2011/24/EU on the rights of patients in remote cross-border healthcare using telemedicine, describes them. Although future challenges must be posed in interoperability and compliance with the General Data Protection Regulation (GDPR).
PROFILE OF THE SUSCEPTIBLE PATIENT REGARDING TELEMEDICINE CARE
The profile of the patient with osteoporosis who comes to our consultations is getting older, with more associated chronic diseases and, probably, with a greater limitation for face-to-face access to follow-up medical consultations.
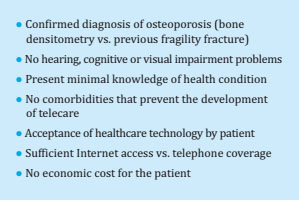
There are different formats of telematic consultation such as telephone consultation, video call, specific telematic platforms. The success of this communication lies in choosing, in a personalized way, the proposal that best suits each patient24. Thus, prior to the consultation, the person’s functional and cognitive situation, their cultural level, socio-family environment and the presence of sensory or compression deficits that would favor the presence of a relative during the consultation should be assessed.
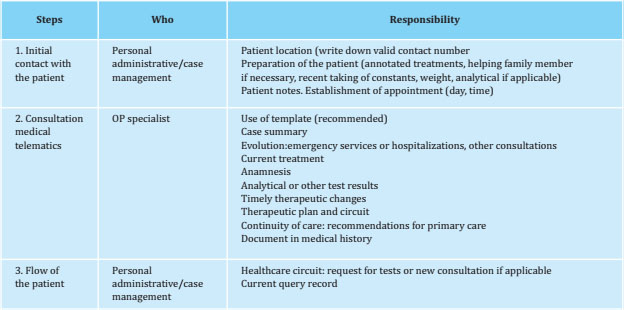
An important aspect is the role of nursing in telematic consultation. As in the FLS model8,9, it would be to establish initial contact with the patient who meets the inclusion criteria (Table 2) into inform them that the planned medical consultation will be telematic (specifying date and time), and preparing the patient in relation to relevant information for this visit (Table 3)13.
Subsequently, the osteoporosis specialist will carry out the telematic consultation in the available format, preferably following a template that allows structuring the visit in anamnesis, assessment of complementary tests carried out, summary of the case and decision-making in relation to the diagnosis and/or therapeutic plan.
All this should be recorded in the clinical history, to facilitate continuity of care. Finally, the administrative staff will manage, within the healthcare circuit, the complementary tests that proceed, and will schedule a new follow-up visit, if necessary.
CONCLUSIONS
Osteoporosis is a very prevalent chronic disease with great social and health repercussions that requires prolonged treatment over time, an aspect that sometimes complicates adherence to it.
This situation requires us to actively redesign the current healthcare of our patients to ensure a correct identification, assessment and monitoring in a safe and effective way. Knowing the clinical profile of patients referred to an osteoporosis consultation will help to improve the management of this disease.
COVID-19 has occurred in a context in which the main causes of mortality are chronic diseases, and where there are social inequalities, and this also has to do with the expansion of the pandemic. For all these reasons, the long-term care approach that should be used should make it easier for people to protect themselves against transmission. Important changes have been caused in the form of attention in our consultations, some of them will surely be reversed with the passage of time; Others, such as the increase in non-contact visits at the expense of face-to-face visits, are presumably to last once the pandemic is over.
The need to limit access to hospitals and infections has imposed telemedicine, but it is here to stay. There are many advantages that it can offer to professionals and users, becoming a key assistance tool. Faced with this scenario, it is imperative to move towards a more secure and protocolized telematic attention. This care must be carried out in a structured way to be cost-effective. For this, we will previously review the clinical and functional situation in which the patient is located and thus be able to correctly plan said assistance, indicating its need and suitability.
A posteriori, its articulation will be based on a series of guidelines divided into three major steps: the initial contact with the patient, the telematic medical consultation as such and the care flow of the process. The privacy of clinical data is ensured.
It is essential that health authorities make use of scientific knowledge to act in the complex and difficult situation we currently face, to maintain outpatient care for our patients with osteoporosis, prioritizing the evaluation of their results on the health of patients, as well as their impact on health systems in the short and long term.
Bibliografía
1 Cobos M, Rifà Ros A. Consulta no presencial. AMF. 2011;7:96-99. [ Links ]
2 Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020; 26(5):571-573. [ Links ]
3 Ohannessian R, Duong TA, Odone A. global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(2):e18810. [ Links ]
4 Bernad Pineda M, González Fernández CM, Fernández Prada M, Fernández Campillo J, Maeso Martín R, Garcés Puentes MV. Reumatología y Osteoporosis (RETOSS): osteoporosis posmenopáusica en la consulta de reumatología. Reumatol Clin. 2011:7(1):13-19. [ Links ]
5 Blázquez Cabrera JA, Sosa Henriquez M, Díaz-Curiel M, Sánchez Molini P, Arranz García F, Montoya MJ, et al. Perfil de los pacientes que acuden al médico internista para valoración de osteoporosis: registro OSTEOMED. Rev Clin Esp. 2020:S0014-2565(20)30174-0. [ Links ]
6 Sáez-López P, Ojeda-Thies C, Alarcón T, Muñoz Pascual, A, Mora-Fernández J, González de Villaumbrosía C, et al. Registro Nacional de fracturas de cadera (RNFC): Resultados del primer año y comparación con otros registros y estudios multicéntricos españoles. Rev Esp Salud Pública. 2019; vol 93: 18 de octubre e201910072. [ Links ]
7 Blanch J, Nogués X, Moro MJ, Valero MC, del Pino-Montes D, Canals L, et al. Circuitos de atención médica de la paciente con osteoporosis postmenopáusica en España. Rev Osteoporos Metab Miner. 2017;9(2):62-71. [ Links ]
8 Mitchell P, Åkessond K, Chandrane M. Implementation of models of care for secondary osteoporotic fracture prevention and orthogeriatric models of care for osteoporotic hip fracture. Best Pract Res Clin Rheumatol. 2016;30(3):536-558. [ Links ]
9 Capdevila-Reniu A, Casanova T, Sopena E, Cancio JM. Seguimiento telemático a los pacientes con fracturaspor fragilidad. Rev Esp Geriatr Gerontol. 2020;55(6):375-376. [ Links ]
10 Naranjo A, Ojeda-Bruno S, Bilbao Cantarero A, Quevedo Abeledo JC, Henríquez-Hernández LA, Rodríguez-Lozano C. Results of a model of secondary prevention for osteoporotic fracture coordinated by rheumatology and focused on the nurse and primary care physicians. Reumatol Clin. 2014;10(5):299-303. [ Links ]
11 Covid-19 Lliçons apreses per una reforma del sistema de salut de Catalunya. Consell de Col·legis de Metges de Catalunya. Juny 2020. [ Links ]
12 Fuentes B, Alonso de Leciñana M, Calleja-Castaño P, Carneado-Ruiz J, Egido-Herrero J, Gil-Núñez A, et al. Impact of the COVID-19 pandemic on the organisation of stroke care. Madrid Stroke Care Plan. Neurologia. 2020;35(6):363-371. [ Links ]
13 Barrios V, Cosín-Sales J, Bravo M, Escobar C, Gámez JM, Huelmos A, et al. Telemedicine consultation for the clinical cardiologists in the era of COVID-19: present and future. Consensus document of the Spanish Society of Cardiology. Rev Esp Cardiol (Engl Ed). 2020; 73(11):910-918. [ Links ]
14 Ena J. Telemedicina aplicada a COVID-19. Rev Clin Esp. 2020;220(8):501-502. [ Links ]
15 De la Fuente Ballesteros SL, García Granja N, Hernández Carrasco M, Hidalgo Benito A, García Álvarez I, García Ramón E. La consulta no presencia como herramienta de mejora de la consulta a demanda en atención primaria. Semergen. 2018;44(7):458-462. [ Links ]
16 Van Den Berg N, Schumann M, Kraft K, Hoffmann W. Telemedicine and telecare for older patients -A systematicreview. Maturitas. 2012;73:94-114. [ Links ]
17 Criteris i escenaris de priorització assistencial en el marc COVID-19 per al desenvolupament de l’activitat assistencial. Scientia (Dipòsit d'Informació Digital del Departament de Salut. Generalitat de Catalunya). Juny, 2020. [ Links ]
18 Paskins Z, Crawford-Manning F, Bullock L, Jinks C. Identifying and managing osteoporosis before and after COVID-19: rise of the remote consultation? Osteoporos Int. 2020;31(9):1629-1932. [ Links ]
19 Slater H, Dear BF, Merolli MA, Li LC, Briggs AM. Use of eHealth technologies to enable the implementation of musculoskeletal Models of Care: Evidence and practice. Best Pract Res Clin Rheumatol. 2016;30(3):483-502. [ Links ]
20 Palcu P, Munce S, Jaglal SB, Allin S, Chishtie JA, Silverstein A, et al. Understanding patient experiences and challenges to osteoporosis care delivered virtually by telemedicine: a mixed methods study. Osteoporos Int. 2020;31(2):351-361. [ Links ]
21 Gallacher S, Alexander S, Beswetherick N, Carr W DA, Gittoes N, Gray A, et al. Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. Royal Osteoporosis Society; 2019. [ Links ]
22 Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-962. [ Links ]
23 Garg V, Brewer J. Telemedicine security: A systematic review. J Diabetes Sci Technol. 2011;5:768-777. [ Links ]
24 Kanis JA, Harvey NC, McCloskey E, Bruyère O, Veronese N, Lorentzon M, et al. Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int. 2020;31(1):1-12. [ Links ]
Received: November 15, 2020; Accepted: January 11, 2021











 text in
text in