INTRODUCTION
Lipofibromatous hamartoma (LFH) is a rare, benign tumor with less than 180 cases reported in the literature that affects peripheral nerves causing hypertrophy and infiltration of the perineurium and epineurium by fibroadipose tissue that surrounds and separates axonal fibers [1]. It has a predilection for the arms, affecting primarily the median nerve and its branches in 66–80% of cases [2]. Although a definitive diagnosis can be achieved by histopathology, a biopsy implies putting motor and sensory function of the nerve at risk. Imaging studies are a diagnostic alternative since pathognomonic data can be observed [3].
CASE REPORT
A 31-year-old man came to the plastic surgery clinic because of a 29-year history of a soft fixed mass in his right hand with areas of dysesthesia and anesthesia of the median nerve. The patient reported that this tumor appeared at 2 years of age, starting asymptomatically at the level of the radial part of the interdigital region of the right hand and extending distally towards the third finger during the first years, and later proximally towards the third finger, the central part of the palm, the wrist and the distal third of the forearm.
At 9 years he underwent a first and only surgical intervention with removal of approximately 70% of the tumor, reconstruction with Z-plasty, and placement of a skin autograft in the proximal third of the ulnar side of the third finger. The median nerve was not released at the level of the carpal tunnel. The pathology report of the biopsy that was processed in the same institution of the surgery was inconclusive describing the findings as a peripheral nerve with normal axonal fibers surrounded by abundant fibroadipose tissue.
Years after the procedure, the lesion reappeared with rapid growth, extending to the third finger, the thenar region, and the center of the palm with a volume increase in the radial side of the second finger and the back of the hand between the second and third metacarpal. For this reason, the patient came for medical evaluation.
On physical examination, scars were observed on the palm of the right hand, the third finger, and the distal third of the forearm with a soft, fixed and non-painful tumor being evident on palpation on the volar side of the hand and extending to the distal third of the forearm, the thenar region, the center and the radial side of the interdigital region, the third finger in its totality, and the radial side of the second finger with a notable separation of the space between the third and second metacarpal and an increase in volume of the dorsal region at this level (Figure 1).
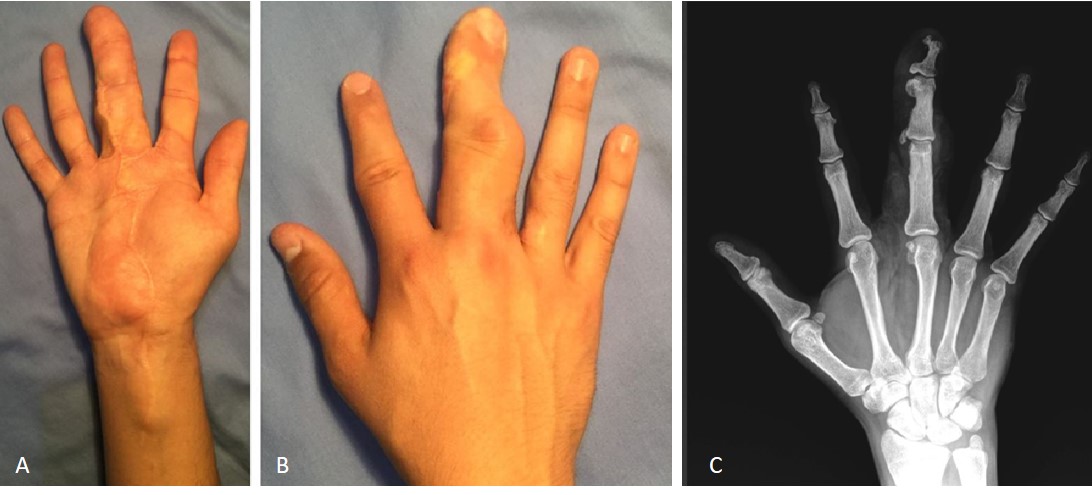
Figure 1. Lipofibromatous hamartoma of the median nerve, volar (A) and dorsal (B) aspect of the right hand.A Z-plasty and skin autograft in the proximal third of the ulnar face of the third finger is seen. Note the separation between the third and second metacarpal with an increase in volume. (C) Anteroposterior x-ray of the right hand. Exostoses are seen in the phalanges of the middle and index fingers. There is gigantism of the middle finger with increased distance between the second and third metacarpal (fourth collateral branch of the median nerve that infiltrates the second lumbrical nerve).
On dynamic assessment, there was evident atrophy of the opponens pollicis muscle with an inability to achieve adequate opposition of the thumb with the fifth finger. The rest of the dynamic assessment was within normal parameters. Sensitivity testing with the Semmes- Weinstein monofilament showed altered sensitivity of the median nerve with a deficit in the discrimination of 4/8 points in the right hand and a normal sensitivity of 8/8 in the left hand. Tinel´s sign was positive; however, the patient denied a history of symptoms due to carpal tunnel nerve compression. Phalen's test was negative. Electromyography was not performed.
The plain film revealed an increase in soft tissue volume around the middle finger with exostosis of the middle and distal phalanges of the middle finger and in the middle phalanx of the index finger, in addition to the gigantism of the middle finger. An increase in the distance between the second and third metacarpal was also seen, with fat density images corresponding to the fourth collateral branch of the median nerve that innervates the second lumbrical (Figure 1). No similar tumors or adenopathies were detected in the rest of the extremities.
Magnetic resonance imaging (MRI) was performed on T1-weighted sequences, where the tumor was identified in the carpal tunnel extending to the level of the proximal phalanx of the middle finger, separating the flexor tendons, and causing a mass effect and infiltration with atrophy of the second lumbrical muscle by fatty tissue and scattered nerve fibers. The tumor extended to the collateral branches of the median nerve on the radial and ulnar sides of the index and middle fingers, with distribution in the cutaneous branches of the nerve and with fat replacement of the muscles of the thenar region (Figure 2).
A computed tomography (CT) study showed fatty tissue infiltration in the soft tissues of the palm and on the index and middle finger, with distribution along the branches of the median nerve (Figure 2).
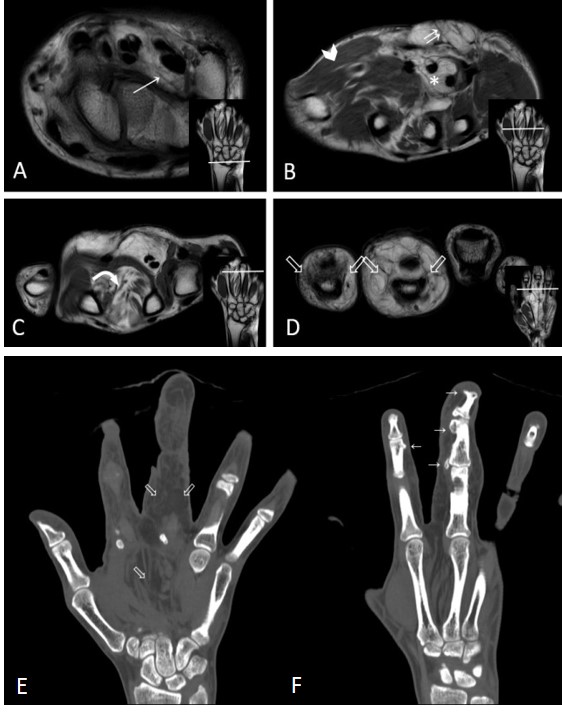
Figure 2. Magnetic resonance axial images of the hand in T1 weighted sequences.(A). Separation of the flexor tendons by fatty tissue is identified, observing fine hypointense lines distributed in the fatty tissue (arrow) that correspond to the median nerve. (B). Separation of the flexor tendons by fat tissue (asterisk). Note the distribution of the cutaneous branches of the median nerve infiltrated by fibroadipose tissue, conditioning separation of the nerve fibers (double arrow). Discrete atrophy with fatty replacement of the muscles (arrowhead). (C). Axial image at the distal metacarpal level. The lipofibromatous hamartoma follows the distribution of the fourth collateral branch of the median nerve between the second and third metacarpals, conditioning a mass effect and fatty infiltration with atrophy of the second lumbrical. (D). The lipofibromatous hamartoma is observed in the fourth to the collateral branches of the median nerve on the radial and ulnar sides of the index and middle fingers (hollow arrows). (E, F) Computed tomography of the lipofibromatous hamartoma of the median nerve with coronal reconstruction. (E). Infiltration of fatty tissue between the soft tissues (hollow arrow), at the level of the palm and on the index and middle fingers with distribution along the branches of the median nerve. (F). Exostoses (arrows) are also seen on the index and middle fingers.
No further surgery or treatment was performed after the evaluation due to the risk of a motor-sensory deficit as sequelae. Also, the patient did not want surgical treatment because of prior surgical sequelae. Since the functionality of his hand was relatively preserved and the patient did not present symptoms of carpal tunnel syndrome, it was decided not to perform a new surgery. The carpus and hand joints were immobilized with a splint for 1 week, and then physical rehabilitation was begun with grip, and finger extension, adduction, and abduction exercises, as well as cold/heat physical therapy for 1 month. The patient currently continues with the symptoms and motor-sensory deficit mentioned previously, and surgical intervention will be postponed until his functionality is affected.
DISCUSSION
MRI findings in LFH are considered pathognomonic [2]. On axial images the affected nerve is increased in size and the nerve fibers are separated and interspersed in the fibroadipose tissue giving it the image of a “coaxial cable” and “spaghetti” when seen coronally [4, 5]. The fibro-osseous tunnels of the arms restrict the distribution of the tumor in the nerve due to its inability to expand causing the tumor to proliferate more freely and irregularly [2, 5]. Axonal fibers are seen at low intensity in all sequences (T1WI and T2WI) [6, 7]. There is no associated inflammation or edema of the affected limb. Contrast medium (gadolinium) has not been demonstrated to be significantly useful in the diagnosis of LFH due to poor enhancement, representing a non-specific finding [8].
Ultrasound findings in LFH are also pathognomonic, observing a significant fusiform increase of the affected nerve that, when it affects the median nerve, characteristically extends from the distal part of the forearm to the palm or fingers of the hand [7]. The normal fibrillar pattern of the nerve is lost with the formation of a mass of hyperechogenic fatty tissue in the epineurium, interspersed with internal anechoic echoes that correspond to normal-appearing nerve fibers without showing an increased flow in color Doppler color scanning [2, 7]. When the patient refers carpal tunnel syndrome nerve fibers with focal tumefactions can be seen [5].
CT scans are not routinely carried out in hand tumors; however, fibers with soft tissue density surrounded by tissues with fat density at the level of the carpal tunnel can be observed [2]. In many cases of LFH, exostosis, ectopic calcifications, and focal bone gigantism in the territory of the affected nerve can be observed with subsequent premature interphalangeal osteoarthrosis [2, 3].
Although the definitive diagnosis is obtained by histopathology, MRI can be used in the diagnosis of the lesion since pathognomonic findings can be observed, especially when lesions are large. This avoids an unnecessary neural lesion caused by performing a biopsy [1, 2, 9]. We, like others [8], consider that an LFH biopsy represents an unnecessary risk since there is no therapeutic relevance and it puts the studied nerve at risk.
CONCLUSION
There is no definitive treatment for LFH [2]. When there are symptoms of compression of the carpal tunnel, surgical decompression can be considered but due to its complex architecture, the surgical approach of an LFH is a challenge. It can be difficult to identify an LFH with MRI without histology. However, the purpose of this work is to emphasize that MRI findings of LFH are pathognomonic and that it is not necessary to expose the patient to a biopsy, jeopardizing motor and sensory function of the limb. We propose MRI for the diagnosis of LFH with support from other imaging techniques such as CT and plain film radiography for surgical planning, if necessary.














