INTRODUCTION
Cancer is among the foremost reasons of death in the whole world. According to the World Health Organization (WHO) 2020 data, breast, lung, prostate, colon and rectum cancers are the most common types of cancer. High body mass index (BMI), unhealthy diet, low consumption of vegetables and fruits, sedentary life, tobacco use, and alcohol consumption are the behaviors associated with death from cancer. The effectiveness of cancer treatment is affected by factors such as metabolic disorders and malnutrition (1,2). The European Society for Clinical Nutrition and Metabolism (ESPEN) recommends regular evaluation of food intake, weight change and BMI in order to detect nutritional disorders in cancer patients at an early stage. The prevalence of malnutrition in cancer patients ranges from approximately 20 % to 70 %, with patient age, cancer type and cancer stage causing different outcomes. Disease-related malnutrition (anorexia, cachexia, and sarcopenia) is defined as a condition resulting from the activation of systemic inflammation by an underlying disease such as cancer. The inflammatory response leads anorexia and tissue destruction. Thus, loss of body weight, changes in body composition and decrease in physical function can be seen. The form of medical nutrition therapy in cancer patients is based on the patient’s medical history, appetite, type of cancer, stage of cancer and response to treatment (3-5).
Cancer is a genetic disease which may result in psychiatric illnesses (6). Since cancer is a complex disease that takes a long time to treat, it can also bring socioeconomic and mental problems. Depression, which is one of these mental problems, can often be masked and overlooked by other illnesses. In addition, anxiety can often accompany depression (7). The prevalence of psychiatric diseases among cancer patients is within a wide range of 30-60 % (8). In a systematic review and meta-analysis study that included forty studies covering a 15-year period, the prevalence of major depression and anxiety disorders defined by Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) or defined by the International Classification of Diseases 10th Revision (ICD-10) in cancer patients was found to be 22 % and 18 %, respectively. Improved screening and treatment for psychiatric disorders in cancer patients will likely improve quality of life and reduce both morbidity and mortality (9).
Folic acid and vitamin B12 act as coenzymes in the metabolic pathway of homocysteine. In serum folic acid and vitamin B12 deficiency, methionine synthetase activity is disrupted and plasma or serum homocysteine levels increase. High concentrations of homocysteine are toxic to neural cells. Homocysteine is thought to play a role in the pathogenesis of neurodegenerative and psychiatric disorders by disrupting neuronal plasticity and activating neuronal degeneration (10,11). In addition, vitamin B12 affects the methylation of neurotransmitters such as dopamine, serotonin, and norepinephrine at the molecular level, affecting the synthesis and levels of these neurotransmitters. It is stated that this situation is effective in the pathogenesis of various psychiatric and neurological disorders by disrupting the neurotransmitter balance (12). It has been suggested that a deficiency of serum vitamin D may be associated with depression, anxiety and stress. However, it is not clear whether serum vitamin D levels are associated with anxiety, independent of depression (13). In a study with healthy individuals, no significant relationship was found between serum 25(OH)D levels and anxiety scores (14). Many recent conflicting studies are investigating the possible relationship of depression and other mental disorders with vitamin D (15,16). This study was planned to evaluate the serum vitamin D and B12 levels, nutritional status, and depression and anxiety among adults diagnosed with cancer and individuals with characteristics similar to the patient group (PG) who were not diagnosed with cancer.
METHODS
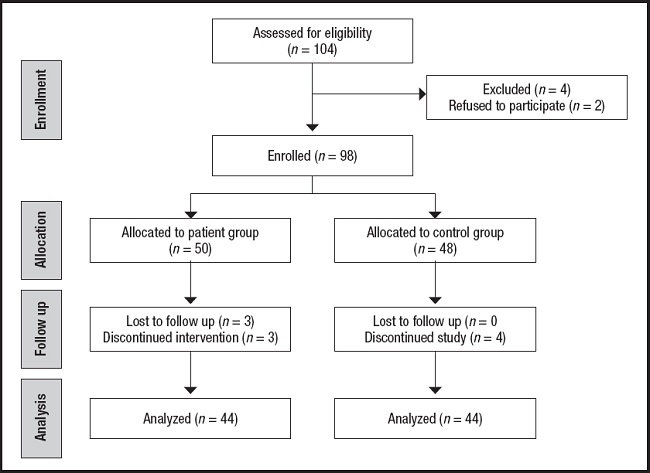
This study was carried out with 44 patients aged 18 to 64 (PG) who were diagnosed with cancer and applied to the Chemotherapy Unit of a university hospital located in Erzincan, Turkey, for treatment, and 44 healthy volunteers (control group, CG) with no diagnosis of cancer, who had similar characteristics to the age and gender-matched patient group and applied to Internal Medicine of the same hospital. In order to find out whether the sample size is sufficient in the study, post-hoc power analysis was performed using the G.Power 3.1.9.2 program. Patients diagnosed with cancer were followed up in two periods, after the first course and the last course of chemotherapy while the chemotherapy treatment was in progress. The data of the study were collected in winter and spring seasons. Exclusion criteria included pregnancy and breastfeeding, being diagnosis with diabetes, obesity, depression, and anxiety. The study was approved by the ethics committee of Ankara Yildirim Beyazit University (Project number: 2019-133) and all subjects were given written consents in compliance with the Declaration of Helsinki. The questionnaire form was administered by the researcher using face-to-face interview technique in order to find out the demographic characteristics, health conditions, lifestyle habits, and nutritional habits of the individuals (Fig. 1).
ASSESSMENT OF DIETARY INTAKES
The nutritional habits of the participants were assessed by a food frequency questionnaire and 24-hour dietary recall form. Average energy and nutritional values of consumed food were analyzed using Computer Aided Nutrition Program, Nutrition Package Information Systems Program (BEBIS) developed for Turkey (17).
ASSESSMENT OF ANTHROPOMETRIC MEASUREMENTS
All measurements were taken by researcher. Participants’ body weight was obtained using the SECA 799 Digital Scales. The height of participants was recorded using the SECA 220 mechanical measuring tape after the Frankfurt plane conditions were met. Waist circumference (WC) (cm), hip circumference (HC) (cm), and mid upper arm circumference (MUAC) (cm) were measured and recorded by the researcher using a non-stretching tape measure. Triceps skinfold thicknesses (TST) (mm) were measured using a Holtain Skinfold Caliper. BMI values were calculated by dividing the bodyweight of the individuals by the square meter of their height (kg/m2) (18). The waist-hip ratio (WHR) was calculated by dividing waist circumference by hip circumference (19).
BIOCHEMICAL PARAMETERS
Blood samples were collected from each participant after a 10-12 hour night fast. Biochemical tests were analyzed in the laboratory of the university hospital and the test results were obtained from the hospital database.
EVALUATION OF MALNUTRITION STATUS
Malnutrition risk was assessed with Patient-Generated Subjective Global Assessment (PG-SGA) considering the medical history and nutritional symptoms of cancer patients having applied to the Chemotherapy Unit (20-22).
ASSESSMENT OF ANXIETY AND DEPRESSION STATUS
Depression and anxiety levels were assessed using the Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI) (23-26).
STATISTICAL ANALYSIS
Data were analyzed using SPSS (Statistical Package for Social Sciences) version 22 (IBM SPSS Statistics 22). In order to compare two groups, when parametric test conditions were met, the Independent groups t-test (Student’s t) was used; in cases where they were not provided, the Mann-Whitney U test was used. Whether there was a difference between the groups in terms of qualitative variables was determined through the Pearson’s Chi-squared (χ2) test. To evaluate the relationships between the scales and some research findings, Pearson product moments correlation analysis was implemented. Dietary associations were assessed by odds ratios and 95 % confidence intervals. The factors affecting BDI and BAI scores were analyzed using linear regression. A p-value < 0.05 was considered to be statistically significant.
RESULTS
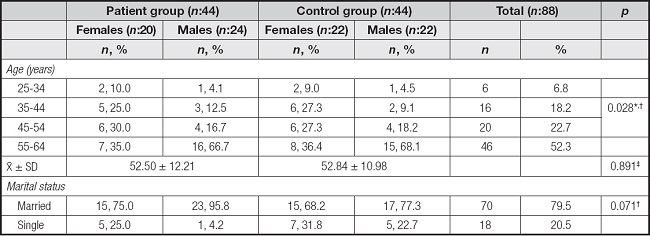
Table I shows the distribution of 44 cancer cases and 44 controls by demographic characteristics. There was a similarity in the mean age of the individuals in PG and CG (52.50 ± 12.21 years and 52.84 ± 10.98 years). The majority of men (95.8 % in the PG, 77.3 % in the CG) and women (75.0 % in the PG, 68.2 % in the CG) in both groups were married.
In this study, the patients who had gastrointestinal system cancers were 31.8 %, and those who had non-gastrointestinal system cancers were 68.2 % (data not shown). The group of individuals according to their anthropometric measurements are given in table II. The average BMI after the first cure in the PG was 29.07 ± 3.30 kg/m2 in women and 27.1 ± 3.98 kg/m2 in men. It was 25.97 ± 3.18 kg/m2 in women and 24.36 ± 3.26 kg/m2 in men after the last cure of chemotherapy. The average BMI was 24.14 ± 3.21 kg/m2 in women and 25.94 ± 2.35 kg/m2 in men in the CG. The difference between the mean BMI of the two groups is statistically significant (p < 0.05).
Table II. Anthropometric measurement averages of individuals, standard deviations (X̅ ± SD) and lower and upper values.
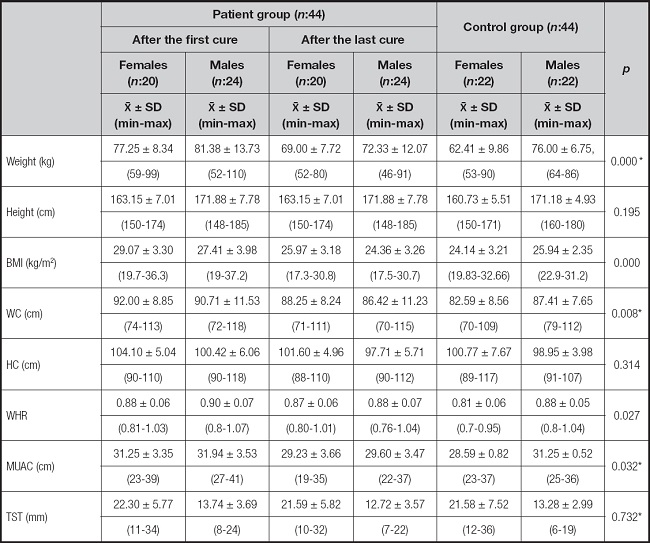
Mann-Whitney U test.
WC: waist circumference; HC: hip circumference; WHR: WAIST-HIP RATIO; MUAC: mid-upper arm circumference; TST: triceps skinfold thickness.
*p < 0.05.
In table III, serum vitamin D and B12 levels of individuals are given. Mean serum vitamin B12 was 311.7 ± 127.1 pg/ml after the first cure in PG, 313.7 ± 151.3 pg/ml after the last cure, and 342.8 ± 150.4 pg/ml in CG (p > 0.05). Serum vitamin D mean was 18.2 ± 10.2 ng/ml after the first cure in PG, 15.84 ± 8.4 ng/ml after the last cure and 22.17 ± 15.8 ng/ml in CG (p > 0.05).
Table III. Serum vitamin D and B12 levels of individuals after the first and after the last cure.
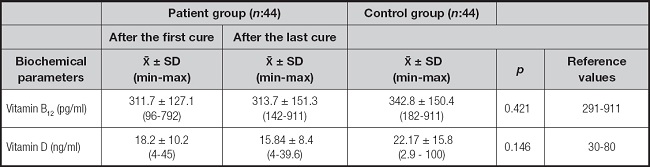
Mann-Whitney U test.
*p < 0.05.
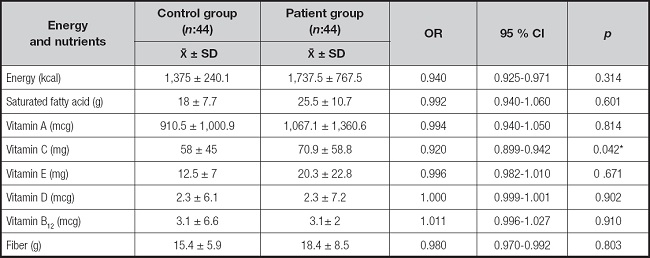
The dietary risk factor and the cancer risk were evaluated and given in table IV. It was determined that vitamin C intake decreased the risk of cancer (for vitamin C, OR: 0.920, 95 % CI: 0.899-0.942). No relationship was found for energy and other nutrients.
The correlation status between the BDI and BAI scores of the individuals in PG and CG and serum vitamin D and B12 values were examined in table V. BDI scores of individuals in PG after the first cure (13.35 ± 6.61 in women, and 16.75 ± 8.07 in men) showed mild depression severity, and BDI scores after the last cure (21.15 ± 9.49 in women, and 22.63 ± 9.51 in men) showed moderate depression severity. Individuals in CG had minimal depression severity (9.68 ± 8.67 in women, and 8.23 ± 5.21 in men). BAI scores of individuals in PG after the first cure (16.15 ± 7.68 in women, and 18.46 ± 8.99 in men) showed moderate anxiety symptoms, and BAI scores after the last cure (27.35 ± 9.93 in women, and 27.58 ± 9.26 in men) showed severe symptoms of anxiety. In PG individuals, both BDI and BAI scores increased from the first cure to the last cure, and their depression and anxiety worsened (p < 0.001). Minimal to mild anxiety symptoms were detected in individuals with CG (9.68 ± 10.27 in women, and 5.86 ± 2.51 in men). PG-SGA scales scores increased from the first cure to the last cure (3.86 ± 3.66 after the first cure, and 11.34 ± 4.39 after the last cure) in PG individuals (p < 0.001) (data not shown). The relationship between serum vitamin D and B12 values, and scores from BDI and BAI after the first and last cure of individuals in PG was not found statistically significant. Results in CG were similar to PG (p > 0.05). In addition, the relationship between PG-SGA scale scores and serum vitamin D and B12 values were not statistically significant (p > 0.05).
Table V. BDI, BAI and PG-SGA scale scores and serum vitamin D and B12 values.
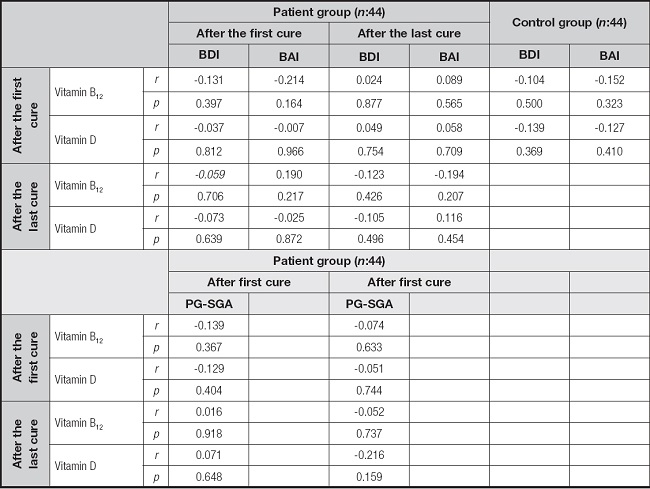
BDI: Beck Depression Inventory; BAI: Beck Anxiety Inventory; PG-SGA: Patient-Generated Subjective Global Assessment.
*p < 0.05, Pearson Product Moment Correlation Analysis.
The regression analysis of the associations between vitamin concentrations, body mass index and PG-SGA, BDI and BAI in cancer patients is shown in table VI. Considering the results of linear regression analysis, it was found that the change in BAI score and the change in BMI, vitamin B12 level, and PG-SGA score were statistically significantly related (p < 0.05). A higher BAI score indicates an increased level of anxiety. It was found that with a decrease of one unit in BMI, the BAI score increased by 1.2 points (β = 0.311, p = 0.040), and with a decrease of in serum vitamin B12 level, BAI score increased by 0.015 points (β = -0.406, p = 0.006). A higher PG-SGA score points out an increased risk of malnutrition. In addition, it was determined that one-unit increase in the PG-SGA score, which reflects the nutritional status of cancer patients, caused an increase of 0.809 points in the BAI score (β = 0.389, p = 0.009).
Table VI. Regression analysis of the relationships between the concentrations of vitamins, BMI, and PG-SGA and BDI, BAI in cancer patients.
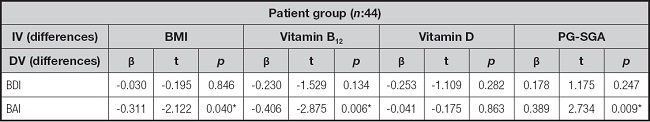
IV: independent variables; DV: dependent variables; BMI: body mass index; BDI: Beck Depression Inventory; BAI: Beck Anxiety Inventory; PG-SGA: Patient-Generated Subjective Global Assessment.
*p < 0.05, linear regression analysis.
DISCUSSION
Cancer is a severe health problem that causes morbidity and mortality (27). One of the most important conditions of a healthy life is adequate and balanced nutrition. Many chronic diseases cause metabolic changes in the body and cause nutritional disorders (28). In this study, the average BMI from the first cure to the last cure displayed a decrease in PG, similar to the literature (29,30). The decrease in food intake due to problems such as pain, fatigue, difficulty in swallowing, nausea and vomiting, oral mucositis, and diarrhea, which are the side effects of chemotherapy treatment, may have caused a decrease in the BMI averages of the patients.
In this study, the average serum B12 level was in the normal range for individuals in PG and CG. Also, serum vitamin D level was decreased during chemotherapy in PG. In a study comparing 93 individuals with advanced-stage colorectal cancer receiving chemotherapy treatment and 224 healthy adults, it was determined that serum vitamin B12 levels were sufficient before and during chemotherapy, and there were no significant differences between the control group (p > 0.05) (31). A study on postoperative nutritional deficiencies in patients with esophageal cancer or gastric cancer revealed that the incidence of vitamin B12 and vitamin D deficiencies was 6.35 % and 36.67 %, respectively, and the vitamin levels were significantly ameliorated after nutritional interventions (32). In this study, the mean daily dietary vitamin B12 intake for individuals in PG were 3.3 ± 2.6 mcg/day. In cancer patients, it is recommended to give vitamins and minerals approximately equal to the daily intake recommended for healthy individuals. In the absence of certain deficiencies in these individuals, the use of high doses of micronutrients is not recommended (3). According to the recommended dietary allowances (RDAs), to meet the nutrient requirement for vitamin B12 the average daily dietary intake should be 2.4 mcg/day (33). It is thought that vitamin B12 deficiency has not yet been reflected in biochemical parameters among individuals in PG and CG, since it is a late condition that develops as a result of not consuming foods containing vitamin B12 and inadequate absorption. In PG, the serum vitamin D average of individuals after the first cure was found to be higher than after the last cure (p < 0.05). The mean daily dietary vitamin D intake for individuals in PG was 2.3 ± 6.1 mcg/day. According to the RDAs, to meet the nutrient requirement for vitamin D the average daily dietary intake should be 15 mcg/day (33). In this study, vitamin D deficiency was detected in terms of both dietary intake and serum levels before and after chemotherapy. In a case-control study, before starting chemotherapy, 25(OH)D3 levels were found to be lower in cancer patients as per the control group. In addition, immediately after chemotherapy, 25(OH)D3 levels decreased slightly (-5.1 nmol/l, 95 % CI: -10.7-0.5, p = 0.082) but increased six months after chemotherapy (34). Another study observed a significant decrease in vitamin D levels after chemotherapy, with 82.4 % of subjects found severely deficient at baseline, and the rate increased to 89.0 % after chemotherapy (35). In this study, serum vitamin D mean was higher in individuals in CG than in PG. The difference between serum vitamin D mean for PG and CG was not statistically significant (p > 0.05). Yao et al. found that serum vitamin D levels were lower in the patient group (22.8 ng/ml) than in the control group (26.2 ng/ml) in their study with breast cancer patients (p < 0.001) (36). While cancer treatment continues, the prolongation of the time spent at home due to chronic pain and fatigue and the decrease in the time to benefit from sunlight may explain the decline in serum vitamin D levels from the first to the last cure. It is thought that the inability of individuals to get enough vitamin D with foods and supplements may also have an effect on this issue. On the other hand, the lower level of serum vitamin D levels in PG supports the relationship between vitamin D deficiency and cancer reported in previous studies.
In this study, it was found out that vitamin C taken with a daily diet diminishes the risk of cancer (OR: 0.920, 95 % CI: 0.899-0.942, p = 0.042). The results of a meta-analysis study showed that dietary vitamin C was inversely related to pancreatic cancer risk (37). In another meta-analysis including three prospective cohorts and seven case-control studies, it was stated that vitamin C intake was inversely associated with the risk of renal cell carcinoma (38). Supporting the consumption of foods rich in vitamin C and providing education on healthy nutrition and cancer risk are thought to be necessary in order to protect the health of individuals and reduce the risk of cancer development.
Vitamin D exerts beneficial effects on the nervous system by contributing to synaptic plasticity, neuroprotection, and dopaminergic system physiology. In addition, vitamin D exhibits anti-inflammatory effects in the brain, reducing the production of pro-inflammatory cytokines by activated microglia and increasing γ-glutamyl-transpeptidase in glutathione pathways, reducing oxidative load in neurons and microglia. Low serum vitamin D levels are noteworthy in patients influenced by neuropsychological diseases. Depression is caused by a change in neural activity resulting from an increase in glutamate that drives excitatory neurons. Vitamin D regulates nerve growth factor, which protects against glutamate toxicity, and glial-derived nerve growth factor, which protects against ischemia and 6-hydroxydopamine toxicity (39,40). Vitamin B12 plays a tremendous role in the nervous system by acting as a coenzyme in the metabolic pathway of homocysteine and by affecting the methylation of neurotransmitters such as dopamine, norepinephrine, and serotonin at the molecular level. Because vitamin B12 affects the synthesis and levels of neurotransmitters, its deficiency plays a role in the pathogenesis of various psychiatric and neurological disorders by disrupting the neurotransmitter balance (10-12). Since its deficiency is associated with depression, it is important to maintain normal serum vitamin D and B12 levels for optimal production of neurotransmitters associated with adequate function of the nervous system. Determining the depression and anxiety levels of cancer patients and providing supportive psychological treatments are very important in terms of self-acceptance of the illness, compliance with treatment and increasing the quality of life (9,41).
The relationship between serum vitamin D and B12 values with BDI and BAI scores after the first and last cure of individuals in PG was not found statistically significant (p > 0.05). Zhao et al. found no significant relationship between serum 25(OH)D concentrations and the presence of depression in a study they conducted with 3,916 American adults aged 20 years and older (42). In another study, no significant correlation was found between serum 25(OH)D concentration and HADS-D (Hospital Anxiety and Depression Scale, subscale depression) scores of cancer patients evaluated at three time points during a total 24-month follow-up period. However, it is noteworthy that none of the patients reached the estimated mean requirements (EAR) of vitamin D (10 μg/day or 400 IU) at baseline or prospective phase, and 39.3 % had serum 25(OH)D levels below 75 nmol/l (43). The results are in line with the current literature. However, contrary to the findings in this study, some studies also found a significant negative relationship between vitamin D levels and depression scores (44,45). Factors such as differences in population groups (ethnic and other cultural differences), age group, seasonal variation, methods of detecting depression, and different types of methods used for serum vitamin D analysis are possible reasons for the emergence of contradictory results in the literature (45,46). In addition, Nanri et al., in a study they conducted on seasonal factors, found a relationship between 25(OH)D and depression symptoms in the winter months, but not in the summer months. It has been suggested that the working season has an enormous impact on results (47). This study was conducted between April and December, and it is thought that seasonal variation may be effective in the relationship between serum vitamin D levels and depression scores. Notwithstanding depression and anxiety scores were high, they were not affected by serum vitamin D and vitamin B12 levels, suggesting that being a cancer patient is a risk factor in itself.
In this study, according to linear regression analysis results, the change in BAI score was significantly associated with the change in BMI, vitamin B12 level, and PG-SGA score (p < 0.05). It was determined that with a decrease of one unit in BMI, the BAI score increased by 1.2 points (β = 0.311, p = 0.040), and with a decrease in serum vitamin B12 level, the BAI score increased by 0.015 points (β = -0.406, p = 0.006). In addition, it was determined that one-unit increase in the PG-SGA score, which reflects the nutritional status of cancer patients, caused an increase of 0.809 points in the BAI score (β = 0.389, p = 0.009). In cancer, body protein mass decreases and cachexia begins to appear. Loss of appetite and excessive weight loss can be seen in cancer cachexia. Similar to this study, while anxiety and depression levels increased during adjuvant chemotherapy in bladder cancer patients, BMI was found to be a potential predictor (48). In addition, in a study evaluating the nutritional status of 99 patients with advanced head and neck cancer with PG-SGA, poor nutritional status was positively correlated with higher levels of psychological distress (r = 0.37, p < 0.001) (49). Inadequate nutritional intake is frequently observed in patients. PG-SGA is a scale used to evaluate the nutritional status of cancer patients, taking into account body weight loss, disease, metabolic stress, and physical examination (50,51).
As stated in the findings of the study, chemotherapy treatment mediated the development of anxiety in cancer patients by changing vitamin B12 levels and anthropometric characteristics with its negative effect on nutritional status. Decreased food intake due to the side effects of chemotherapy treatment (such as pain, fatigue, difficulty in swallowing, nausea-vomiting, oral mucositis, diarrhea) may cause a decrease in the mean BMI of patients. Chemotherapy treatment may pave the way for the development of depression and anxiety by influencing the levels of vitamin D and vitamin B12 with its negative effects on physical activity and eating habits. New research may be conducted to observe the effects of nutritional interventions on anxiety and depression levels in cancer patients receiving chemotherapy treatment.
Cancer patients have a higher risk of developing depression and anxiety than those with other chronic diseases. However, this psychological state is often overlooked. It is predicted that interventions to improve nutritional status, gain adequate and balanced dietary habits, and preserve muscle mass in cancer patients will be effective on patients’ depression and anxiety. It should be ensured that cancer patients treated with chemotherapy follow a healthy and balanced diet plan that is suitable for their needs and has adequate vitamin and mineral content.
STRENGTHS
This case-control study evaluates the association of nutritional status and serum vitamin D and B12 levels with depression and anxiety in adult cancer patients receiving chemotherapy. In the literature, no definite conclusion has been reached in this area. For this reason, it is anticipated that this article will contribute to the discussions on the field. In addition, in this study, patients diagnosed with cancer were followed up in two periods, after the first course and the last course of chemotherapy while the chemotherapy treatment was in progress. The originality of this article stems from this point.