Introduction
The Escala sobre la Representación Cognitiva de la Enfermedad [Cognitive Illness Representation Scale], known as ERCE (De los Santos-Roig, 2009), was developed in Spanish based on the Common Sense Model and is composed of five subscales (identity, causes, consequences, control/cure, and course) which assess patients' perceptions about illness. Prior works on this scale (De los Santos-Roig & Pérez-Meléndez, 2013) showed first psychometrical guarantees of ERCE: items as appropriate indicators of construct definition (expert judgments), content validity (specification tables, items development, expert judgments, pilot study), items analysis (descriptives, homogeneity, and discrimination between extreme groups). An exploratory factorial analysis (EFA) showed a four-factor solution for “consequences” and a three-factor solution for “control/cure” dimensions, which accounted for an acceptable percentage of variance (76.01% and 51.58%, respectively). This was in accordance with previously defined facets. In addition, evidences about reliability (Chronbach's alpha) and stability of items' scores (test-retest) were also found (De los Santos-Roig & Pérez-Meléndez, 2014).
The aim of this study is go further providing known-groups validity evidences of ERCE scale by clustering diabetic patients in a profile (+/- cognitive illness representation, CIR) and by studying its relations with metabolic control, health outcomes, and psychological distress. Similarly to other widely-used instruments (e.g., IPQ, IPQ-R, BIPQ), each of the five subscales of the ERCE has its own score. The scores of the subscales cannot be combined into a total overall score. Because of this, the use of strategies such as cluster analysis makes it possible to consider participants' answers globally in all CIR components. The usefulness of cluster analysis lies in its ability to group individuals with similar scores and to study the influence of certain “CIR patterns” on response to treatment, self-care, metabolic control (Skinner et al., 2011), or coping (Medley, Powell, Worthington, Chohan, & Jones, 2010). This is undoubtedly very useful to design much more specific and relevant clinical interventions and to make progress in the assessment of CIR by moving away from the traditional treatment of the scores (French & Weinman, 2008).
According to the Common-Sense Model of Self-Regulation of Health and Illness (Leventhal et al., 1997; Leventhal, Brissette, & Leventhal, 2003; Petrie & Weinman, 2012), patients' beliefs about their disease act as schemata that determine how they cope with and adjust to illness. These beliefs, called “cognitive illness representation” (CIR) in the model, seem to be shaped by perceptions regarding the following components: symptoms and their relationship to the illness (identity), causes, consequences, perceived control over the illness, and course of the illness (evolution and perceived duration). Many studies have found evidence of CIR in several illnesses and conditions including diabetes (Harvey & Lawson, 2009; Hoving, Van der Meer, Volkova, & Frings-Dresen, 2010; Knittle, Maes, & De Gucht, 2010). In diabetes, these beliefs are known to be related to self-care, adherence to treatment, metabolic control, and prognosis (Broadbent, Donkin, & Stroh, 2011; Nie, Han, Xu, Huang, & Mao, 2018; van Puffelen et al., 2015; Vedhara et al., 2016; Wisting et al., 2016). As McSharry, Moss-Morris, and Kendrick (2011) showed in a meta-analysis of nine cross-sectional studies and four randomized controlled trials, stronger identity or attributing more symptoms to diabetes, perceiving higher impact or consequences on patient's life, and seeing diabetes as cyclical or unpredictable had significant positive associations with HbA1c, poorer metabolic control, and poorer self-care. In contrast, perceiving greater personal control was negatively associated with HbA1c. Vedhara et al. (2016) examined illness beliefs in patients with diabetes and foot ulceration. When controlling for other potential clinical and demographic determinants, they found that identity was a significant predictor of time of death.
A few years ago, Hagger and Orbell (2003) demonstrated that CIR is related to health outcomes; more recent studies (in terms of positive or negative CIR) continue to confirm their claim. Gois et al. (2012) and Hudson, Bundy, Coventry, and Dickens (2014) reported that positive CIR (i.e., lower scores on identity and consequences of the illness and higher scores on perceived control of it) was associated with better psychological adjustment (e.g., less anxiety and depression). Kohlmann, Rimington, and Weinman (2012) reported that a positive CIR profile was associated with better physical health (measured with the MOS SF-36 Health Survey) of coronary patients. In addition, a number of studies have shown that when patients hold negative perceptions about an illness, these beliefs are associated with disability and slow recovery and are indicative of a poorer prognosis (Galli, Ettlin, Palla, Ehlert, & Gaab, 2010; Petrie & Weinman, 2012; Thongsai, 2015). It seems that a negative illness representation leads to poorer health and lower adjustment than a positive CIR profile. Furthermore, clinical evidence continues to show that many patients with Type 1 diabetes still have poor metabolic control despite the efforts made to educate them (De los Santos-Roig et al., 2014; Ruiz-González et al., 2016). Considering CIR may help us to understand which other variables (e.g., perceptions, beliefs) are related to metabolic control, health outcomes, and self-care.
In Spain, however, few studies have explored this topic, probably due to the shortage of instruments available in this language to measure CIR. Beléndez Vázquez, Bermejo Alegría, and García Ayala (2005) tested the factor structure of the Spanish translation of the Illness Perception Questionnaire-Revised (IPQ-R; Moss-Morris et al., 2002), but only on a sample of subjects with hypertension. Pacheco-Huergo et al. (2012) adapted the Brief IPQ (BIPQ; Broadbent, Petrie, Main, & Weinman, 2006), and used it with a small sample of 30 chronic patients. Therefore, studies with other instruments and samples are still needed in Spain and in Spanish context. The aim of the present study was twofold: first, to provide validity evidence of the ERCE scale, due to the growing interest in assessing CIR of diabetes in applied research (Rees, Lamoureux, Xie, Sturrock, & Fenwick, 2015); second, to estimate the ability of ERCE scores to predict highly relevant variables (such as health outcomes and metabolic control), as observed in other studies (Clatworthy, Buick, Hankins, Weinman, & Horne, 2005; Clatworthy, Hanskins, Buick, Weinman, & Horne, 2007; Skinner et al., 2011). These two aspects of validity – theoretical and applied – have been dealt with in the most recent literature on the subject (Lissitz & Samuelsen, 2007; Sireci, 2007).
As ERCE was developed in phases, prior work about scale development and first psychometrical data was published in two papers (see De los Santos-Roig & Pérez-Meléndez, 2013, 2014). The present study was focused on validity evidences by testing estimated relations between ERCE scores/clusters and other variables as metabolic control, health status, and distress. So, the following hypothesis were made: (1) we expected all the subscales of the ERCE to be related to one another (i.e., we expected high “identity” to be related to high “consequences” and both to be related to low “control”, etc.); (2) we expected the fact of belonging to a given cluster (+/-CIR) to be associated with statistically significant differences in metabolic control (HbA1c), health outcomes (MOS SF-36 Health Survey), and psychological distress (PANAS and HADS), with poorer results for patients with a negative CIR; (3) finally, we expected patients' perceptions (i.e., CIR profile and perceived seriousness of illness) to have an interactive effect on outcome variables (i.e., HbA1c, health, and psychological distress).
Method
Participants
This study was conducted with a convenience sample of 152 patients with Type 1 insulin-dependent diabetes mellitus, who attended the Endocrinology Unit Day Hospital of San Cecilio University Hospital in Granada, Spain.
Table 1 Sociodemographic Data and Clinical Variables
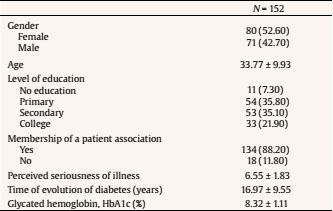
Note. Data are given as n (%) and mean ± standard deviation.
Sample selection and data collection took place in the room normally used for the diabetes education sessions that a small group of patients with diabetes attends for a couple of days each week. The diabetes educator selected all the participants who agreed to cooperate in the study except those with a physical or psychological impairment (e.g., visual impairment, psychopathology, prior diagnosis), those with a recent diagnosis (< 1 year), under-age patients (< 18 years old), and patients who did not have Spanish as their mother tongue.
Each patient signed an informed consent form. In the form, both the diabetes educator and the primary researcher explained the study procedure, its objectives, which data would be collected, and the anonymous nature of the study. The study received prior approval from the hospital ethics committee.
The most relevant characteristics of the sample are shown in Table 1.
Design
An associative and cross-sectional study comparing two groups of diabetic patients (clustered in a positive or negative CIR profile) was conducted.
Instruments
The ERCE scale (De los Santos-Roig, 2009; De los Santos-Roig & Pérez-Meléndez, 2013; 2014), which consists of five non-summative subscales, was administered to assess CIR. The first subscale is identity, which contains a list of 20 symptoms where presence/absence is measured (i.e. sweating, headache, prickling, etc.). Then, patient have to answer about which of those symptoms are related to diabetes (Yes/No). Higher scores indicate more symptoms associated with diabetes. The causes subscale includes a list of 7 possible causes of the disease (e.g., environmental, psychological, biological) and 10 antecedent situations of hyper-/hypoglycemia episodes (i.e. stress, bad day, etc.). The latter were considered in the study. The patient has to tick if an antecedent is present in his/her life. High scores indicate that the patient is able to recognize and attribute different causes to high or low glucose levels. The remain three subscales are responded to on a 5-point Likert scale. Consequences subscale is composed by 16 items (12 about “current” and 4 about “future” consequences). Control/cure is compose by 12 representative items of various control sources; general control (2), personal control (4), treatment control (3), others´ control (2) and cure. Finally course is conformed by 2 items; evolution and duration. High overall scores indicate, respectively, that the illness has a great impact on the patient's life, that he or she can control it, and that the course of the illness is chronic. Cronbach's alpha indices in this study were calculated only for subscales composed by items with a type Likert scale (consequences and control/cure). So, Cronbach's alpha indices were .92 for the consequences subscale and .68 for the control subscale. Course is composed by two items, so alpha index is not appropriate in that case. The test-retest reliability of all the subscales except for causes (qualitative, yes/no) ranged from .63 (consequences) to .81 (course). At the beginning of the scale a general question was included regarding perceived seriousness of the illness (from 1 to 10). For more detailed information on subscales nature please see previous publications (De los Santos-Roig, 2009; De los Santos-Roig & Pérez-Meléndez, 2013; 2014).
Health outcomes were assessed with the Spanish version of the MOS SF-36 Health Survey (Alonso, Prieto, & Antó, 1995; Vilagut et al., 2005; Ware & Sherbourne, 1992; Ware, Snow, Kosinski, & Gandek, 1995). This questionnaire refers to patients' health status in the past four weeks. Items are grouped into eight subscales (i.e., physical functioning, physical role, bodily pain, vitality, social functioning, emotional role, general health, and mental health). Then, two higher-level components are formed by the sum of the respective subscales: overall physical health (composed of the subscales physical functioning, physical role, bodily pain, and general health) and overall mental health (composed of the remaining subscales). The scores of all the subscales range from 0 to 100 (higher scores indicate better health). The scale has psychometric guarantees [35]. In this study, Cronbach's alpha indices ranged from .76 (general health) to .91 (bodily pain).
Psychological distress was assessed with two scales. One of them was the Positive and Negative Affect Scale (Watson, Clark, & Tellegen, 1988), validated for the Spanish population by Sandín et al. (1999). This scale is composed of 20 items that assess negative affect (10 items) and positive affect (10 items). Participants were asked to respond on a 5-point Likert scale from 1 (totally disagree) to 5 (totally agree). The scale has been reported to have good reliability and validity evidence (Sandín et al., 1999). Cronbach's alpha indices range in men and women from .87 to .89 for positive affect and from .89 to .91 for negative affect. In this study the indices obtained were .90 and .84, respectively. The other scale was the Hospital Anxiety and Depression Scale, HADS (Zigmond & Snaith, 1983), which was used to assess anxiety and depression. The Spanish version was developed by De las Cuevas Castresana, García-Estrada, and González de Rivera (1995). It is composed of 14 items that ask patients how often they feel as indicated in the statement. The scale of each item ranges from 1 to 5 (never-every day). A recent meta-analysis (Terol-Cantero, Cabrera-Perona, & Martín-Aragón, 2015) showed a good internal consistency of the anxiety subscale, ranging from .74 to .87, and of the depression subscale, ranging from .75 to .87, according to the studies. In this study, Cronbach's alpha values were .77 and .70 for anxiety and depression, respectively. The validity evidence and factor structure of the scale have been also reported (Terol-Cantero et al., 2015).
Finally, we obtained the most recent data on glycated hemoglobin (HbA1c) for each patient, except for n = 27 (17% of missing data). This measurement is obtained with a test conducted routinely on patients who are admitted in the day hospital.
Procedure
Data collection began once the study had been approved by the hospital ethics committee and patients had signed the informed consent form.
Table 2 Results of Patients in each Cluster (+/-CIR) regarding all Variables
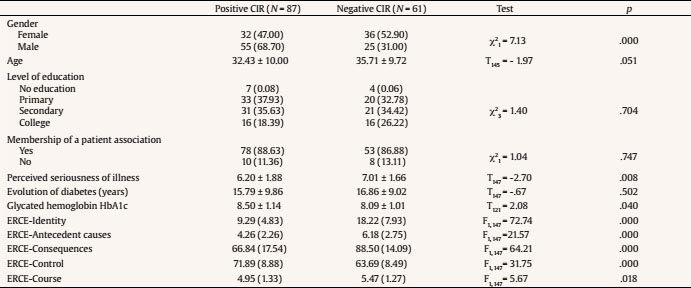
Note. Data are given as n (%) and mean ± standard deviation.
Instruments were administered in two sessions: the ERCE scale and SF-36 Health Survey on the first day and the psychological distress scales on the second day. Regrettably, not all patients answered all instruments. Most of them were unable to attend the second day of the assessment for several reasons: not being able to because of work, not being interested in continuing the study, living many miles away, etc. Figure 1 shows a flowchart with study attrition. Despite this, we decided to analyze all available data. The procedures followed during the full data collection period were the same for all patients, who completed the scales under similar conditions.
Statistical Analysis
Data analysis consisted of a series of bivariate correlation analyses between all ERCE subscales in order to estimate that all the components were related to one another as expected. After that, participants were clustered using a k-means cluster analysis considering the scores on all the ERCE subscales. The recommendations of Clatworthy et al. (2007) were followed and SPSS software (v.23) was used for these purposes.
Then a series of parametric tests (t-tests) and non-parametric tests (chi-square tests) were performed to estimate the statistical differences between +/- CIR groups in all variables (socio-demographic and clinical variables included) before conducting any other analyses.
Finally, the predictors (i.e., CIR and perceived seriousness of illness) were analyzed separately and jointly to determine their simple and interactive estimated effects on criterion variables. The PROCESS macro for SPSS was used to run the hierarchical regression analyses (Model 1) (Hayes, 2013). We introduced perceived seriousness of illness (PS) and CIR cluster (+/-) as predictor variables. We coded the CIR cluster condition as -.5 for negative CIR (i.e., more symptoms, more consequences, less control) and .5 for positive CIR. We also centered the continuous predictor variables (PS) before computing the interaction terms (Cohen, Cohen, West, & Aiken, 2013). The criterion variables were HbA1c, SF-36 subscales and overall physical and mental components, PANAS negative and positive affect, and HADS anxiety and depression subscales.
Results
Bivariate Correlations
First, we conducted bivariate correlations for all ERCE subscales. Results indicated that all the components were moderately but significantly correlated with at least another ERCE component. Specifically, identity scores were positively and significantly correlated with antecedent situations, r(149) = .389, p = .001, future consequences, r(149) = .262, p = .001, and overall consequences, r(149) = .224, p = .006, and marginally correlated with current consequences, r(149) = .13, p =. 098. Antecedent situations were significantly correlated with general control, r(149) = -.294, p < .0001, treatment control, r(152) = -.172, p = 035, control by others, r(152) = -.164, p = .034, and overall control, r(152) = -.273, p = .001. Correlations between control and consequences were statistically significant only for current consequences and general control, r(152) = -.174, p = .033. Finally, control was significantly correlated with course, r(152) = -.184, p = .023. Size effects of all correlations ranged from medium to high (3% to 15% of explained variance).
Cluster Analysis: Parametric and Non-Parametric Tests
A k-means cluster analysis was performed. Results suggested that the sample should be divided into two groups (i.e., positive CIR and negative CIR), so the analysis was conducted this way. The two resulting groups can be described as follows: the positive CIR group had lower scores on identity and antecedent situations, lower scores on consequences and course, and higher scores on perceived control over diabetes compared to the negative CIR group. As shown on Table 2, a one-way ANOVA revealed significant differences between these two groups of patients in all the subscales of the ERCE. Size effect ranged from medium (Cohen's d = 0.32 for course) to high (Cohen's d = 1.20 for identity). Also, a series of t-tests and chi-square tests were conducted to analyze the potential statistically significant differences between the two groups in sociodemographic and clinical variables as well. As shown in Table 2, the two groups did not differ in any variables except for gender, χ2 = 7.13, p < .0001, perceived seriousness of illness, t(147) = -2.70, p = .008, and age, t(145) = -1.97, p = .051, marginally significant.
Regression Analyses
After verifying that the clusters clearly indicated two different groups of patients, we conducted a series of hierarchical regression analyses. We introduced all variables related to illness cognitions – cluster (+/-CIR) and perceived seriousness (PS) – as predictors of the criterion variables, which were HbA1c, health outcomes, and psychological distress. Table 3 shows means and standard deviations of all measured variables.
Results indicated that +/-CIR was a significant predictor of HbA1c and of all the subscales of the MOS SF-36 Health Survey (Table 4). All effect sizes rounded Cohen's d = 0.40 (medium effect). The ability of CIR cluster to predict PANAS-negative affect subscale was marginally significant, b = - 0.50 (0.26), t(61) = -1.90, p =. 06. CIR cluster did not predict any other subscale of psychological distress.
Table 4 Hb1Ac and Health Outcomes (MOS SF-36) as a Function of +/- CIR and Perceived Seriousness (PS)

Note. ms = marginally significant.
*p < .01, **p < .05.
Table 4 shows similar results for PS. Although PS was not a significant predictor of HbA1c or psychological distress, it significantly predicted almost all the physical subscales of the MOS SF-36. All effect sizes rounded Cohen's d = 0.40 (medium effect) except for general health sub-scale, which was d = 0.92 (high effect). Results for emotional role, mental health, and SF-36 mental health component were marginally significant (p < .09).
As for the interactions, results were significant for the AD36-physical role subscale, b = 0.42 (0.17), t(147) = 2.50, p = .01 (d = 0.41), and marginally significant for the SF36-emotional role subscale, b = 0.40 (0.22), t(147) = 1.83, p =.06. There was a significant interaction between PS and +/-CIR in prediction of HADS-anxiety, b = - 0.57 (0.27), t(161) = -2.08, p = .04 (d =.53). Table 4 and Figure 2 shows the statistically significant results. As shown on the figure, scores on the SF36- physical role subscale were significantly lower when PS was high, but only for patients in the negative CIR group, t(147) = 3.99, p < .0001. The same results were observed for the HADS-anxiety subscale: patients in the negative CIR group with high PS had significantly higher anxiety scores, t(61) = - 2.75, p < .0001.
Discussion
The starting hypotheses of this study were partially supported by the results. As regards the relationships between components, results agreed with our theoretical and empirical expectations, since moderate estimated intercorrelations were found between ERCE components. Overall, results indicated that having a large number of symptoms (identity) was associated with a high impact of the disease (consequences) as well as the attribution of a large number of situations as causes of these symptoms (antecedent situations). Moreover, consequences, antecedent situations, and a chronic course of the disease were associated with a low perceived control over it. These results replicate other authors' findings obtained with the IPQ-R and other instruments (Beléndez Vázquez et al., 2005; Broadbent et al., 2006; Hagger & Orbell, 2003; Moss-Morris et al., 2002).
After finding this evidence of the expected relationship between the components of CIR, we performed a cluster analysis to classify patients with different perspectives about illness and to verify whether the clusters obtained predicted differences in metabolic control (HbA1c), health outcomes, and psychological distress. Both groups of patients (+/-CIR) differed in all the variables of interest, thus providing validity evidence of ERCE scores. Results showed differences in HbA1c but in the opposite way to that expected: positive CIR group patients had less metabolic control (higher HbA1c values). These results are not consistent with some recent meta-analyses (Hoving et al., 2010; Kohlmann et al., 2012; McSharry et al., 2011), in which patients with high HbA1c had a negative CIR. This may be due to the large number of lost data (17%) or to patients having a positive but inaccurate view of their disease. Some misconceptions about illness have been reported to have a negative effect on self-care behaviors and outcomes (Astin & Jones, 2006; Ruiz-González et al., 2016). Regrettably, the accuracy of CIR was not assessed in this study. However, this does not seem to be a likely explanation since CIR cluster was found to be a significant predictor of health outcomes and psychological distress.
As regards health outcomes, CIR cluster predicted poor functioning (physical, emotional, and social), less vitality, more pain, and poor physical and mental health, as reported in other studies (Broadbent et al., 2011; Dempster, Howell, & McCorry, 2015; Hudson et al., 2014). Moreover, the literature has reported the existence of relationships between illness cognitions and quality of life, disability and fatigue, physical functioning, general health (Broadbent et al., 2011; Dempster et al., 2015; Hoving et al., 2010) and mortality. Vedhara et al., (2016) found illness perceptions predicted survival in patients with diabetes and foot ulceration. Chilcot, Wellstead, and Farrington (2011)7 found negative beliefs about the effectiveness of treatment predicted mortality in patients with end stage renal disease. More recently, Crawshaw, Rimington, Weinman, and Chilcot (2015) reported that changes in illness perceptions (i.e., from positive to negative beliefs), predicted mortality in cardiac patients. All these findings are in line with our results, as negative CIR was associated with poorer health, functioning, and quality of life and greater psychological distress. As regards mental health, studies suggest that patients' beliefs about the control of their disease are the best indicator of their mental health (Arran, Craufurd, & Simpson, 2014; Hudson et al., 2014; Zoeckler, Kenn, Kuehl, Stenzel, & Rief, 2014). Antecedent situations were expected to be associated with higher anxiety and depression scores and poorer psychosocial functioning (Arran et al., 2014; Hoving et al., 2010); in addition, the findings of other studies suggest that cyclical course is a significant predictor of aspects related to anxiety, depression, and pain (Arran et al., 2014; Evans & Paul, 2009; Zoeckler et al., 2014). In our study, patients with a positive CIR had fewer antecedent situations and more perceived control over their illness. Results indicated they had less bodily pain, better physical and psychosocial functioning, better mental health, and less negative affect. These results are in line with previous research and support the validity and clinical utility of the ERCE scale.
Finally, as both groups differed in all variables related to illness perceptions (CIR and perceived seriousness), the joint influence between CIR and PS on criterion variables were analyzed. Interesting results were found regarding functioning and anxiety. It seems that relations between CIR and criterion variables are mediated by PS but this affected only patients with a negative CIR. More research is needed to confirm these results and to explain this mediating role. In our study, PS was assessed only with one question in the scale, which may have been biased.
We would like to acknowledge the limitations of this study. First, it was conducted with a modest sample of patients who voluntarily agreed to participate, which may have caused some bias. Second, there was a large amount of missing data, due to invalid HbA1c data collection and to the loss of patients on the second day of assessment. The study had an associative design, so it is not possible to establish cause-effect relationships and internal validity is therefore not as relevant as in experimentation. In terms of external validity, this could be an important limitation to generalizing and extrapolating results, but we considered the convenience of presenting results as they were collected and analyzed and will take all conclusions with caution. Third, we did not control the fact that patients themselves may have distorted reality or made it more socially desirable. These methodological and design limitations should be taken into account when considering this study, which should be followed by more research, and when planning future studies with the ERCE scale.
In short, we found acceptable validity evidences of the ERCE to consider it a useful tool for measuring diabetes perceptions in a more global and interdisciplinary way. Nurses, health psychologists, doctors, etc. could use ERCE scale. Assessing patients' cognitive illness representations open up new ways to treat those who are at risk of poor control or poor adjustment or who simply do not adhere to treatment. This allows diabetes educators to adjust information and treatment to each individual, which in turn leads to a more efficient assistance and better support of patients.

















